Vascular Occlusion Role in the Etiopathohegenesis of Idiopathic Sudden Sensorineural Hearing Loss: Risk Analysis with Hematological Parameters
By Selcuk Yildiz, Sema Zer TorosAffiliations
doi: 10.29271/jcpsp.2020.06.606ABSTRACT
Objective: To evaluate the concomittant metabolic disorders, mean platelet volume (MPV), and neutrophil to lymphocyte ratio (NLR) in patients with idiopathic sudden sensorineural hearingloss (SSNHL) in comparison to healthy controls.
Study Design: Case-control study.
Place and Duration of Study: Department of Otorhinolaryngology, Head and Neck Surgery, University of Health Sciences, Haydarpaşa Numune Training and Research Hospital, Turkey, from December 2016 to May 2019.
Methodology: Fifty-five patients aged 18-59 years and diagnosed with idiopathic SSNHL and 145 healthy individuals who applied for a hearing screening within the same time period (control group). Demographics, concomitant diseases, laboratory results, and outcome of pure tone audiometers were recorded. MPV and NLR were the outcome measures.
Results: The percentage of individuals with high MPV level was 10.9% in the idiopathic SSNHL group, it was identified as 2.8% in the control group (p = 0.040). The average NLR was higher in patients with idiopathic SSNHL than control group (1.7 (1.42-2.20) and 1.5 (1.29-1.88), p = 0.004). A NLR level of 2.01 and above is associated with 2.881 times higher risk of idiopathic SSNHL (odds ratio 2.881, 95% confidence interval 1.427-5.817).
Conclusion: High MPV and NLR values are associated with idiopathic SSNHL, suggesting the role of vascular pathologies in etiology of idiopathic SSNHL. Therefore, patients with idiopathic SSNHL should undergo detailed evaluation including hematological indices.
Key Words: Idiopathic sudden sensorineural hearing loss, Mean platelet volume, Neutrophil to lymphocytes ratio.
INTRODUCTION
Sudden sensorineural hearing loss (SSNHL) was first described by Klein in 1944. It is defined as hearing loss occurring in the sensorineural component at 30 dB and above in 3 consecutive frequencies within 72 hours.1
SSNHL can be seen in all age groups, but fewer cases have been reported in children and the elderly. It is most common between the ages of 30-60 and in the vast majority of cases, a single ear is involved. Its incidence is reported to be 5-20 / 100,000.2 However, since it is a disease that can recover spontaneously without a doctor's application, the incidence is thought to be higher than specified.
Since the treatment will be etiological, the underlying cause has an important role in the treatment of these patients. An underlying cause (acoustic neuroma, etc.) can be detected in only 10% of patients diagnosed with SSNHL. The rest of the group is considered as idiopathic.3 Treatment is started empirically as the exact cause of idiopathic SSNHL is not known. The most commonly used agents in treatment are steroids and antivirals and hyperbaric oxygen.
Various theories have been proposed to explain the cause of idiopathic SSNHL. The main ones are: viral infection, vascular occlusion, intraccochlear membrane rupture, and autoimmunity.4 In the proposed theories, vascular and inflammatory causes are prominent. In recent years, MPV and NLR have been extensively studied to investigate the etiopathogenesis and prognosis of microvascular diseases.5 It has been suggested that the risk of thrombosis increases with increasing size of platelets in microvascular diseases.5 Therefore, high MPV has been associated with increased incidence of microvascular complications in diabetes mellitus and increased mortality in coronary artery disease.6 NLR has been recognised as an indicator of inflammatory stres.7
Table I: Demographics and concomitant diseases of the study groups.
|
|
Total (n=200) |
Patients with idiopathic SSNHL |
Healthy controls |
p |
|
|
Age (year) |
42.83 ±9.19 |
41.75 ±11.24 |
43.23 ±8.29 |
0.307a |
|
|
Sex |
Female |
101 (50.5%) |
32 (58.2%) |
69 (47.6%) |
0.181b |
|
Male |
99 (49.5%) |
23 (41.8%) |
76 (52.4%) |
||
|
Concomitant diseases |
Hypertension |
22 (11.0%) |
9 (16.4%) |
13 (9.0%) |
0.135b |
|
Diabetes mellitus |
24 (12.0%) |
8 (14.5%) |
16 (11.0%) |
0.495b |
|
|
Hyperlipidemia |
13 (6.5%) |
2 (3.6%) |
11 (7.6%) |
0.521c |
|
|
aStudent’s t test, bChi-square test, cFisher’s Exact Test. SSNHL = Sudden sensorineural hearing loss. Data are presented as mean±standard deviation or n (%). |
|||||
Table II: Mean platelet volume and neutrophil to lymphocyte ratio of the study groups.
|
|
Total (n=200) |
Patients with idiopathic SSNHL |
Healthy controls |
p |
|
|
MPV |
Low (<4.5 fL) |
17 (8.5%) |
6 (10.9%) |
11 (7.6%) |
*0.040a |
|
Normal (4.5-8.5 fL) |
173 (86.5%) |
43 (78.2%) |
130 (89.7%) |
||
|
High (>8.5 fL) |
10 (5.0%) |
6 (10.9%) |
4 (2.8%) |
||
|
NLR, median (IQR) |
1.6 (1.32-1.93) |
1.7(1.43-2.20) |
1.5 (1.29-1.88) |
**0.004b |
|
|
NLR <2.01 |
156 (78%) |
35 (63.6%) |
121 (83.4%) |
**0.003c |
|
|
NLR ≥2.01 |
44 (22%) |
20 (36.4%) |
24 (16.6%) |
||
|
aFisher Freeman Halton Test, bMann-Whitney U test, cPearson Chi-Square test, p<0.05, p<0.01. SSNHL= Sudden sensorineural hearing loss, MPV= Mean platelet volume, NLR = Neutrophil to lymphocyte ratio, SD = Standart deviation, IQR = Interquartile range, fL = Femtoliter. Data are presented as n (%) or mean±SD, and median (IQR). |
|||||
Table III: Predictive value of neutrophil to lymphocyte ratio for idiopathic SSNHL in ROC analysis.
|
Predictive value of NLR |
ROC curve |
||||||||
|
Cut-off |
Sensitivity |
Specificity |
PPV |
NPV |
OR |
95% CI |
Area |
95% CI |
p |
|
≥2.01 |
36.4% |
83.5% |
77.56 |
45.45 |
2.88 |
1.43-5.82 |
0.631 |
0.544-0.718 |
0.004 |
|
NLR = Neutrophil to lymphocyte ratio, ROC = Receiver operating characteristic, PPV = Positive predictive value, NPV = Negative predictive value, OR = Odds ratio, CI = Confidence interval. |
|||||||||
Increased NLR values have been reported to be associated with high mortality in patients with coronary artery disease.8 Based on this information, we think that MPV and NLR levels change in idiopathic SSNHL and these changes show microcirculatory disorder and inflammatory process in etiopathogenesis.
The aim of this study was to evaluate MPV and NLR levels in idiopathic SSNHL patients according to healthy controls.
METHODOLOGY
It was a case-control study. Total sample was 200 people, 101 females and 99 males.Fifty-five patients (patient group) diagnosed with SSNHL at the ENT Clinic of University of Health Sciences, Haydarpaşa Numune Training and Research Hospital, Turkey, at the age of 18-59 between December 2016 and May 2019; and 145 healthy individuals (control group) who applied for hearing screening within the same period were included in the study. Patients with a history of anatomical external and middle ear disorders and ear surgery were excluded from the study.
Demographic data, medical history, concomitant diseases, physical examination findings, laboratory results and the formation of pure tone audiometers were recorded and statistically compared between patients and control groups. The normal MPV range in complete blood count was considered to be 4.5-8.5 femtoliters (fL).9 Neutrophil and lymphocyte counts were used to calculate NLR. In pure tone audiometry tests, thresholds at 250 Hz, 500 Hz, 1000 Hz, 2000 Hz, 4000 Hz, and 8000 Hz were recorded for the right and left ear for individuals.
The study data were summarised by using descriptive statistics (e.g., mean, standard deviation, median, interquartile range, frequency, percentage). SPSS 22 (Statistical Package for the Social Sciences) (IBM Corp, USA) was used for the statistical analysis. Shapiro-Wilks test and Box Plot graphics were used to evaluate the suitability of the data to normal distribution. In order to test the significance of difference in continuous variables between study groups, Student’s t-test or Mann-Whitney U-test was used for normally or not normally distributed data, respectively. Chi-square test, Fisher-Freeman-Halton test, and Fisher’s Exact testwere used for comparison of qualitative data between study groups. The predictive value of NLR for idiopathic SSNHL was evaluated using receiver operating characteristic (ROC) analysis and optimal cut-off point of NLR was determined with either high sensitivity or high specificity. The odds ratio was calculated as an estimate of relative risk of cut-off NLR on the idiopathic SSNHL as an outcome. Statistical significance was defined as p <0.05.
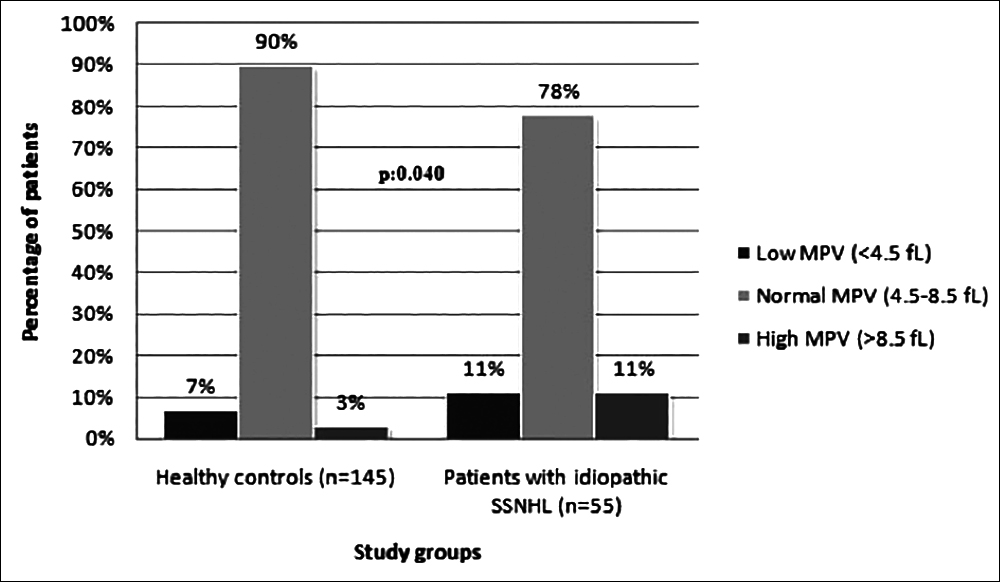 Figure 1: The mean platelet volume (MPV) of healthy controls and patients with idiopathic SSNHL. As the percentage of subjects with normal MPV level was lower in idiopathic SSNHL group than the control group, those of low or high MPV level was significantly higher (p=0.040). fL = Femtoliter, SSNHL = Sudden sensorineural hearing loss.
Figure 1: The mean platelet volume (MPV) of healthy controls and patients with idiopathic SSNHL. As the percentage of subjects with normal MPV level was lower in idiopathic SSNHL group than the control group, those of low or high MPV level was significantly higher (p=0.040). fL = Femtoliter, SSNHL = Sudden sensorineural hearing loss.
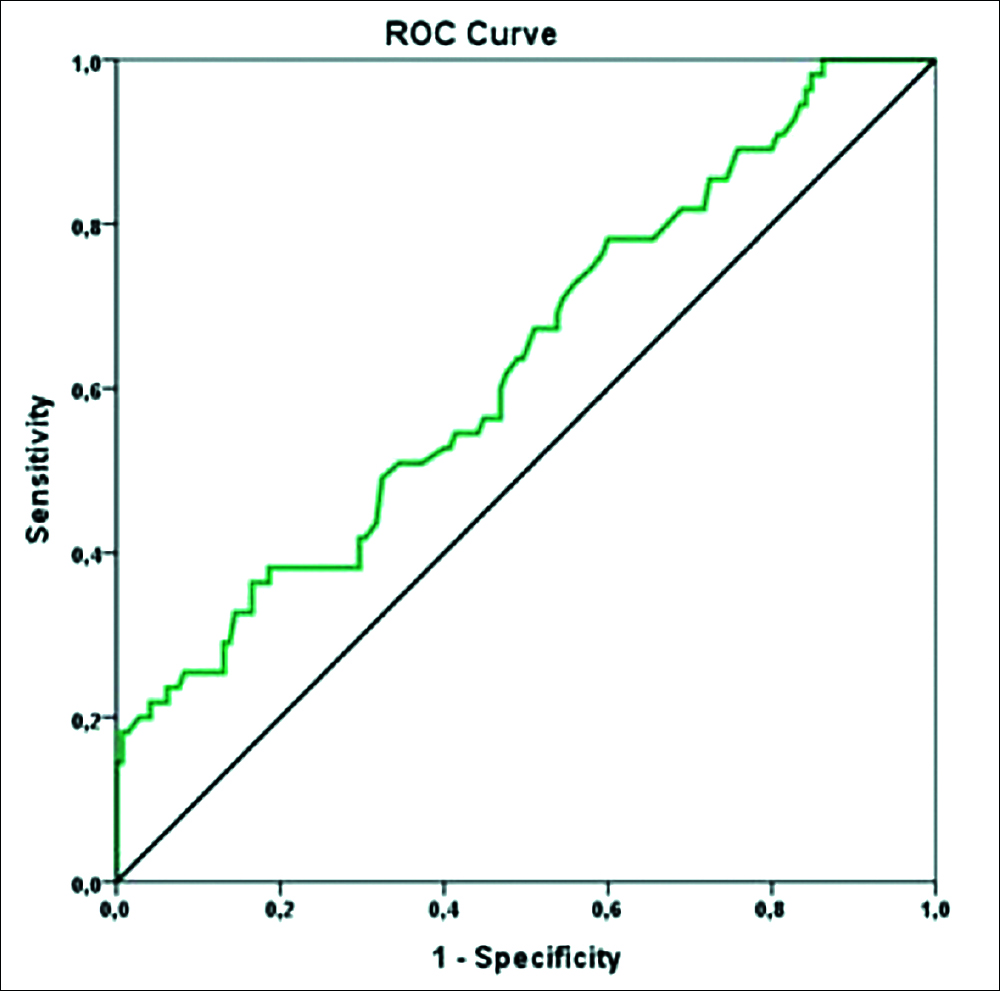 Figure 2: Receiver operating characteristic (ROC) curve for neutrophil to lymphocyte ratio (NLR) to predict idiopathic SSNHL.
Figure 2: Receiver operating characteristic (ROC) curve for neutrophil to lymphocyte ratio (NLR) to predict idiopathic SSNHL.
RESULTS
Demographic data (age and gender) of the case and control groups were compared and no statistically significant difference was found (p>0.05, Table I). Concomittant diseases (hypertension, diabetes mellitus, and hyperlipidemia) of the case and control groups were compared and no statistically significant difference was found (p>0.05, Table I).
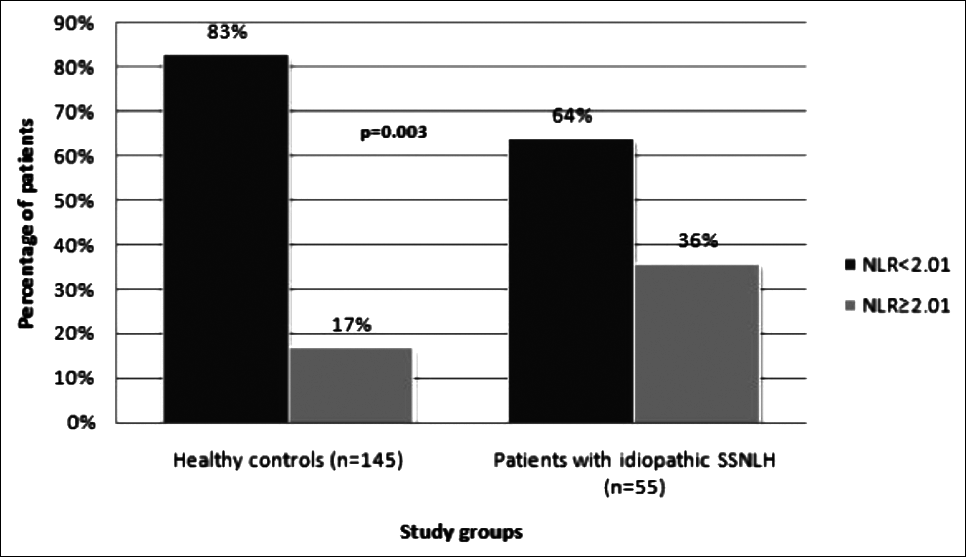 Figure 3:Distribution of individuals in idiopathic SSNHL and control groups with respect to neutrophil to lymphocyte ratio (NLR) cut-off value of 2.01. The percentage of patients having a NLR of 2.01 and above was 36% in the idiopathic SSNHL group and 17% in control group (p = 0.003, Pearson Chi-Square test).
Figure 3:Distribution of individuals in idiopathic SSNHL and control groups with respect to neutrophil to lymphocyte ratio (NLR) cut-off value of 2.01. The percentage of patients having a NLR of 2.01 and above was 36% in the idiopathic SSNHL group and 17% in control group (p = 0.003, Pearson Chi-Square test).
The percentage of individuals with high MPV level was 10.9% in the idiopathic SSNHL group, it was identified as 2.8% in the control group (p = 0.040) (Table II, Figure 1). The avarage NLR was 1.7 (1.42-2.20) in the idiopathic SSNHL group, it was found to be 1.5 (1.29-1.88) in the control group. The avarage NLR was statistically significantly higher in the idiopathic SSNHL group compared to the control group (p = 0.004, Table II).
The optimal cut-off value of NLR for idiopathic SSNHL was calculated as 2.01 (sensitivity 36.4%, specificity 83.5%) in ROC analysis (Table III, Figure 2). The percentage of patients with NLR 2.01 and above was 36.4% in the idiopathic SSNHL group and 16.6% in the control group (p = 0.003) (Table II, Figure 3). NLR level 2.01 and above has 2.881 times higher idiopathic SSNHL risk (rate ratio 2.881, 95% confidence interval 1.427-5.817, Table III).
DISCUSSION
In this case-control study, we found that high-MPV rate and NLR levels were significantly higher in patients with idiopathic SSNHL than healthy individuals. We also calculated the cut-off value of NLR as 2.01. The calculated value was associated with 2.881 times higher risk of idiopathic SSNHL.
Idiopathic SSNHL with an average age of 40 to 54 can be seen in almost all age groups.2 In general, when the studies in the literature are evaluated, no significant finding was found in terms of age distribution.10, 11 Considering the distribution to age groups in this study, no significant distribution difference in patients with idiopathic SSNHL was identified in line with the literature.
It is stated in literature that the gender distribution is generally close to one another and there is no statistically significant difference.10-12 In this study, 23 of the case group consisting of 55 cases were males and 32 were females; 76 of the control group consisting of 145 individuals are males and 69 are females. When the gender distribution is evaluated according to the groups, it is not considered to be statistically significant. This study generally overlaps with the literature in terms of this finding.
Recent studies show that hypertension increases the risk of idiopathic SSNHL.13, 14 Comparing conditions that cause idiopathic SSNHL and endothelial dysfunction, Berjis et al. found the frequency of hypertension to be significantly different in the sudden hearing loss group compared to the control group.14 Hypertension was common in idiopathic SSNHL patients compared to the control group in this study as well. However, there was no statistically significant difference (p = 0.135). In this study, antihypertensive use was not questioned in either groups. If patients using antihypertensive are excluded from the study, the relationship between hypertension and idiopathic SSNHL can be presented more clearly, and the hypothesis that hypertension can disrupt cochlear microcirculation can be tested.
Diabetes mellitus (DM) is observed to increase the frequency of idiopathic SSNHL.15,16 Kitoh et al. found in their study that the severity of hearing loss in idiopathic SSNHL patients showed a significant relationship with DM.17 Durmuş et al. suggested that patients with high blood glucose levels had worse prognosis.10 In this study, DM was more common in the idiopathic SSNHL patient group. However, there was no statistically significant difference (p = 0.495).
Previous studies have reported that individuals with idiopathic SSNHL have higher MPV values.10, 16, 18 Durmuş et al. found that patients with higher MPV values respond less to corticosteroid therapy.10 In accordance with these studies, we found MPV values to be significantly higher in the idiopathic SSNHL group compared to healthy controls. Macrotrombocytes with high thrombotic potential have been previously shown to cause cochlear microcirculation by causing vascular occlusion.5
Studies have found that higher NLR values are higher in idiopathic SSNHL patients.18, 19 Bulğurcu et al. found that the treatment response was lower in patients with higher NLR averages.20 Similarly, in this study, NLR values in the idiopathic SSNHL group were significantly higher than the control group. In the ROC analysis, the NLR cut-off value that we detected with high specificity to predict idiopathic SSNHL was 2.01. Increased NLR is an etiological and prognostic factor for diseases characterised by microcirculation insufficiency and final organ damage.
The main limitation of this study is its retrospective design, which limits the control of confounding factors affecting MPV and NLR and prevents us from reaching a definitive conclusion on vascular pathologies in idiopathic SSNHL etiology. Larger-scale, randomised, prospective studies are required to clearly define the etiopathology of idiopathic SSNHL.
CONCLUSION
High MPV and NLR values may be associated with idiopathic SSNHL, suggesting the role of vascular pathologies in idiopathic SSNHL etiology. Etiopathogenesis of idiopathic SSNHL can be revealed by performing wider ranged series studies with these hematological parameters obtained from a rapid result and low cost examination. By this means, patients can be treated quickly and easily.
ETHICAL APPROVAL:
The study was approved by the Haydarpaşa Numune Training and Research Hospital Clinical Research Ethics Committee, and conducted in accordance with the ethical principles for medical research involving human subjects, outlined in the Helsinki Declaration (approval number of the ethics committee: 2017/67). Informed consent requirement was waived due to the retrospective design of the study.
PATIENTS’ CONSENT:
Informed consents were obtained from the patients to publish the data concerning this study.
CONFLICT OF INTEREST:
Authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
SY, SZT: Conception and design of work, the analysis and interptretation of data, drafting and revision of work, final approval of the version to be published, aggreement to be accountable for all aspects of the work in ensuring that quetions related to the accuracy or integrity of any part of the work are approprately investigated and resolved.
REFERENCES
- Deklein A. Sudden complete or partial loss of function of the octavus-system in apperantly normal persons. Acta Otolaryngol 1944; 32(issue 5-6):407-29.
- Byl FM Jr. Sudden hearing loss: Eight years’ experience and suggested prognostic table. Laryngoscope 1984; 94(5 pt 1):647-61.
- Penido NO, Cruz OL, Zanoni A, Inoue DP. Classification and hearing evolution of patients with sudden sensorineural hearing loss. Braz J Med Biol Res 2009; 42(8):712-6.
- Yoon TH, Paparella MM, Schachern PA. Histopathology of sudden hearing loss. Laryngoscope 1990; 100(7):707-15.
- Varol E, Aksoy F, Ozaydin M, Erdogan D, Dogan A. Relation-ship between mean platelet volume and mitral annular calcification. Blood Coagul Fibrinolysis 2013; 24(2):189-93.
- Buch A, Kaur S, Nair R, Jain A. Platelet volume indices as predictive biomarkers for diabetic complications in Type 2 diabetic patients.J Lab Physicians 2017; 9(2):84-8.
- Kirtane AJ, Bui A, Murphy SA, Barron HV, Gibson CM. Association of peripheral neutrophilia with adverse angiographic outcomes in ST-elevation myocardial infarction. Am J Cardiol 2004; 93(5):532-6.
- Sharma K, Patel AK, Shah KH, Konat A. Is neutrophil-to-lymphocyte ratio a predictor of coronary artery disease in Western Indians? Int J Inflam 2017; 2017:4136126.
- Bancroft AJ, Abel EW, Mclaren M, Belch JJ. Mean platelet volume is a useful parameter: A reproducible routine method using a modified Coulter thrombocytometer. Platelets 2000; 11(7):379-87.
- Durmuş K, Terzi H, Karataş TD, Doğan M, Uysal İÖ, Şencan M, et al. Assessment of hematological factors ınvolved in development and prognosis of ıdiopathic sudden senso-rineural hearing loss. J Craniofac Surg 2016; 27(1):85-91.
- Koçak HE, Elbistanlı MS, Acıpayam H, Alakras WME, Kıral MN, Kayhan FT. Are neutrophil/ lymphocyte and platelet/lymphocyte ratios relatedwith formation of sudden hearing loss and its prognosis? Eur Ann Otorhinolaryngol Head and Neck Dis 2017; 134(6):383-6.
- Hwang GH, Joo JW, Song IS, Rah YC, Choi J. Questionnaires in patients with unilateral sudden sensorineural hearing loss. J Int Adv Otol 2017; 13(2):211-6.
- Chien CY, Tai SY, Wang LF, Hsi E, Chang NC, Wu MT, et al. Metabolic syndrome ıncreases the risk of sudden sensorineural hearing loss in taiwan: A case-control study. Otolaryngol Head Neck Surg2015; 153(1):105-11.
- Berjis N, Moeinimehr M, Hashemi SM, Hashemi SM, Bakhtiari EK, Nasiri S. Endothelial dysfunction in patients with sudden sensorineural hearing loss. Adv Biomed Res 2016; 5:5.
- Mohammed AAM. Lipid profile among patients with sudden sensorineural hearingloss. Indian J Otolaryngol Head Neck Surg 2014; 66(4): 425-8.
- Sağıt M, Kavuğudurmaz M, Güler S, Somdaş MA. Impact of mean platelet volume on theoccurrence and severity of sudden sensorineural hearing loss. J Laryngol Otol 2013; 127(10):972-6.
- Kitoh R, Nishio S, Ogawa K, Kanzaki S, Hato N, Sone M, et al. Nationwide epidemiological survey of idiopathic sudden sensorineural hearing loss in Japan. Acta Otolaryngol 2017; 137:8-16.
- Lee JS, Hong SK, Kim DH, Lee JH, Lee HJ, Park B, et al. The neutrophil-to-lymphocyte ratio in children with sudden sensorineural hearing loss: A retrospective study. Acta Otolaryngol 2017; 137(1):35-8.
- Kum RO, Özcan M, Baklacı D, Yurtsever Kum NY, Yılmaz YF, Ünal A, et al. Investigation of neutrophil-to-lymphocyte ratio andmean platelet volume in sudden hearing loss.Braz J Otorhinolaryngol 2015; 81(6):636-41.
- Bulğurcu S, Dikilitaş B, Arslan İB, Çukurova İ. Neutrophil-to-lymphocyte and platelet-to- lymphocyte ratios in pediatric patients with ıdiopathic sudden hearing loss. J Int Adv Otol 2017;13(2):217-20.