The Relationship between Third-generation TSH Receptor Antibody Positivity and Cumulative Methimazole Dose Used until Remission in Graves' Disease
By Serhat Ozçelik1, Mehmet Celik2, Aski Vural3, Bunyamin Aydin4, Hulya Gozu5Affiliations
doi: 10.29271/jcpsp.2021.05.517ABSTRACT
Objective: To determine the relationship between the positivity of third-generation TSH receptor antibody (TRAb) at the time of diagnosis and the cumulative methimazole dose used until remission in patients with Graves’ disease.
Study Design: Cross-sectional, descriptive study.
Place and Duration of Study: Department of Endocrinology and Metabolic Diseases, University of Health Sciences, Kartal Dr. Lütfi Kırdar City Hospital, Turkey from 2016 to 2018.
Methodology: Newly diagnosed Graves' patients were included in the study. The patients were divided into two groups according to whether they entered remission (n: 21) or not (n: 20), in the 18th month of methimazole treatment. In addition, the patients were further divided into two categories, according to TRAb status at the time of diagnosis as negative (n: 17) or positive (n: 24). The TRAb positivity and the cumulative methimazole dose they used until the month of remission were compared in these groups.
Results: The mean time to reach remission in 41 patients was 20.5 ± 3.1 months. TSH receptor antibody positivity rate was 58.5%. When the TRAb positivity of the groups was compared according to the state of having remission in the 18th month of the treatment, the positivity rate in the non-remission group was statistically significantly higher (p = 0.023).The time to go into remission was longer and the cumulative methimazole dose requirement was higher in the TRAb positive group (p <0.001).
Conclusion: Graves’ disease patients with positive third-generation TRAb were found to have a lower rate of remission in the 18-month period compared to negative patients.
Key Words: Graves’ disease, TSH receptor antibody, Cumulative, Methimazole.
INTRODUCTION
Graves’ disease is an autoimmune disease, mediated by thyroid stimulating hormone receptor antibodies (TRAb).1 Achieving and maintaining remission with antithyroid agents is the main goal in the treatment of Graves' disease.2,3 Remission can be achieved with these medicines, but recurrence is observed in up to 50% of patients after discontinuation of antithyroid agents.4
In various studies, conducted with different types and doses of antithyroid drugs, it has been shown that dose titration with methimazole over 12-18 months is the preferred treatment.5,6 At the onset of the disease, it is not easy to determine which patient will go into remission with antithyroid agents.
Thyroid stimulating hormone receptor antibodies are thought to have a prognostic role as well as their diagnostic value in Graves' disease.7 TSH receptor antibodies are composed of stimulating (TSI) or blocking (TBI) immunoglobulins with different biological activity. While TSH receptor stimulating immunoglobulin increases cAMP production, TBI leads to inhibition.8 Furthermore, there are authors who argue that there are non-classical, non-cAMP signaling pathways.9
TSH receptor antibodies were first measured using thyroid cell membranes, which ended up with low spesificity. In second generation measurement methods, analytical specificity has been increased with chemiluminescent and radioisotope marking. With second generation measurement methods, TRAb presence above 1.5 IU / L is generally accepted as positive for Graves' disease. However, human monoclonal TSH receptor stimulants and blocking immunoglobulins are used in third generation measurement methods. Therefore, it has been reported that sensitivity and specificity are very high (up to ~ 95-97% and 100%, respectively) with these methods.10,11
There are many studies involving the relationship between TRAb and antithyroid drugs in Graves' disease.12,13 However, these studies generally discuss the optimal duration of antithyroid drug therapy. It was desired to examine the effect of cumulative methimazole dose and TRAb positivity on remission from a different perspective. To the best of authors’ knowledge, no research has been conducted that examines the relationship between cumulative methimazole dose and TRAb.
The aim of this study was to determine the relationship between the third-generation TRAb levels of patients with Graves' disease at the time of diagnosis and the cumulative methimazole dose used until remission.
METHODOLOGY
This cross-sectional, descriptive study was carried out between 2016 and 2018 at Adıyaman Education and Research Hospital. The study was approved by İnstitutional Board of Adıyaman University Training and Research Hospital (2-20/2019) and competent authorities of the participating centre, and the trial complied with the Declaration of Helsinki. Inclusion criteria were male and female patients aged 18 years and over, documented Graves’ disease, and newly diagnosed Graves’ disease patients who were treated with methimazole (β-blocker treatment used in case of need) for the first time. Exclusion criteria were low compliance of patients or incomplete medical data, patients treated with propylthiouracil and/or other agents for thyrotoxicosis (e.g. steroid, including pulse steroid for ophthalmopathy; lithium, cholestyramine), patients with side effects of methimazole (e.g. agranulocytosis, cholestatic jaundice, skin rash, pruritus and urticaria), patients who underwent thyroid surgery and/or treated with radioactive iodine, pregnancy and lactation, and patients who do not go into remission within one year after methimazole therapy is discontinued.
Graves' disease was diagnosed with the help of: symptoms of hyperthyroidism, diffuse goiter on physical examination, thyroid-associated ophthalmopathy; high free thyroxine (fT4), free tri-iodothyronine (fT3), anti-Tg, anti-TPO, TSI, TBI; suppressed TSH levels; high uptake in Tc99m scintigraphy (Siemens® E.CAM, Siemens® Medical Systems Inc., Hoffman Estates, IL, USA); the presence of patchy areas with indistinct borders within normal gland echogenicity in thyroid ultrasonography (10 MHz linear probe, LOGIQ® P6; GE Healthcare, Milwaukee, USA) and a prominent increase in vascularity in Doppler ultrasonography.
Serum TSH, free T3, free T4, TBI, TSI, anti-Tg and anti-TPO levels were measured at the time of admission. The term TRAb was used to include: TSI (+) or TBI (+) as well as both TSI (+) and TBI (+). It was taken as ''Positive/Negative'' rather than using actual titre. The authors included patients with TRAb-negative Graves' disease, which was accepted as a subtype, because we only measured TSI and TBI as antibodies. However, it is known that there are neutral antibodies other than TSI and TBI. Since these measurements were not available in the present study, the authors wanted to include the TSI/ TBI negative group in this study. The initial dose of methimazole was determined according to serum thyroid hormone and TSH levels, as 5-10 mg, if serum thyroid hormones were 1-1.5 times the upper limit of normal, 10-20 mg, if serum thyroid hormones were 1.5-2 times the upper limit of normal, 30-40 mg, if serum thyroid hormones were 2-3 times the upper limit of normal, 50 mg, if serum thyroid hormones were 3-4 times the upper limit of normal and, 60 mg, if serum thyroid hormones were 5 times or more the upper limit of normal. Methimazole 60 mg/day was used as the maximum dose. The lowest dose was 2.5 mg, when the methimazole treatment was stopped.
Dosing schedule was applied uniformly in accordance with the titration protocol of this department. The methimazole dose was tapered by checking the thyroid function tests at intervals of 3-6 weeks to find the smallest effective dose. Later, follow-up of thyroid function tests was continued at 1.5-3 month intervals. Remission of Graves’ disease was defined as the lack of detectable TRAb and the state of biochemical euthyroidism (as normal TSH, fT4 and fT3 levels) one year after the withdrawal of methimazole. Thyroid function tests were followed up at 3-month intervals in a year, after methimazole discontinuation. For TRAb negative patients, it was defined as the state of biochemical euthyroidism one year after the withdrawal of methimazole. It was checked whether the patients were in remission in the 18th month of the treatment. For patients who went into remission at 18 months, the cumulative dose of methimazole was calculated at 18 months. For those, who did not go into remission at 18 months, the cumulative dose of methimazole was calculated at their date of remission. In addition, the relationship of baseline TBI and TSI measurements with remission and cumulative methimazole dose was examined.
Fasting blood samples of all patients were taken from the antecubital vein after fasting overnight (at least 8 hours). Thyroid stimulating hormone ( range 0.35–4.95 mIU/L), free T4 (range 0.7–1.48 ng/dL), free T3 (range 1.71–3.71 ng/L), TBI (range 0-14 U/L), TSI (range 0-14 U/L) anti-Tg (0-4,18) and anti-TPO (range 0-5,61) were measured. Analyses of free T3, free T4, TSH, anti-Tg and anti-TPO were performed by immunoassay (chemiluminescence, Beckman Coulter Inc.®, Brea, CA, USA). TSH receptor blocking antibodies ( TSH-REZAK®, Medipan,, Diagnostics, Selchow, Germany) and TSI (IMMULITE® 2000, Siemens, Healthineers, Germany) were performed by radioimmunoassays and chemiluminescent, respectively.
Descriptive statistical methods including percent and mean ± standard deviation (±SD) or n (%), were used to provide the basic features of the data. Categorical independent factors were compared using the Pearson Chi-square test, Fisher's Exact test and Likelihood ratio. Comparison of the quantitative data of the two groups was made using the independent sample t test. All statistical analyses were carried out using SPSS 23.0 version (IBM Corporation, Armonk, NY, USA). A p value <0.05 was considered to indicate statistical significance.
RESULTS
A total of 58 Graves' disease patients treated at Adıyaman Education and Research Hospital, Department of Endocrinology and Metabolism, Adıyaman, Turkey. After the exclusion criteria were met, 41 patients were included in the study (Figure 1). The mean age of our patients was 36.8 ± 11.9 years. While 11 (26.8 %) of the patients were males, 30 (73.2%) were females. The number of smoking patients was 5 (12.2 %). Four patients were excluded due to use of pulse steroid for thyroid-associated ophthalmopathy. The mean time to reach remission was 20.5 ± 3.1 months. TSH receptor antibody positivity rate was 58.5% among all patients. Seven patients got relapse after stopping anti-thyroid medication. TRAb distribution is given in Table I.
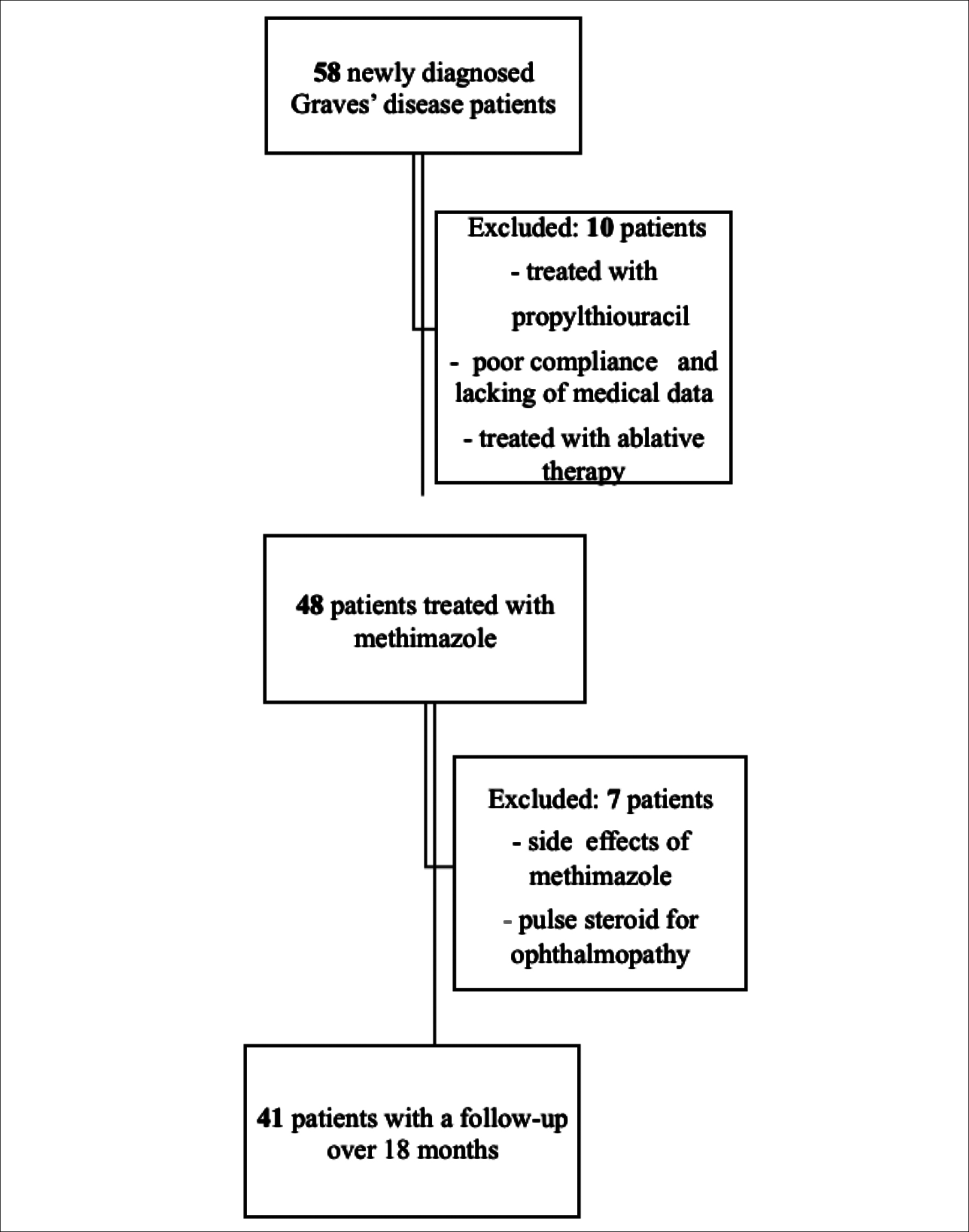 Figure 1: Flow chart of the study.
Figure 1: Flow chart of the study.
Patients were first divided into two groups according to whether they were in remission in the 18th month of continuous methimazole treatment. In the 18th month of the treatment, the number of patients who went into remission was 21, while the number of patients who did not go into remission was 20. The mean time to reach remission for patients who did not go into remission in the 18th month, was 23.1 ± 2.6 months. TSI-only and TBI-only positivity were found to be statistically significantly higher in patients who did not go into remission at 18 months (p=0.023). The calculated cumulative methimazole dose of patients in remission did not differ between the groups (p=0.267, Table II).
Table I: Demographic and biochemical characteristics of the patients.
|
Characteristic |
Value ( n: 41) |
|
Age, years |
36.8±11.9 |
|
Sex (female/male %) |
30(73.2%)/11(26.8%) |
|
Smokers |
5(12.2%) |
|
Time to reach remission (month) |
20.5 ±3.1 |
|
Thyroid function test at diagnosis TSH (mIU/L) Free T3 (ng/dL) Free T4 (ng/dL) |
0.02±0.05 2.25±1.69 8.40±5.64 |
|
TSI (+), (%) |
5 (12.2%) |
|
TBI (+), (%) |
4 (9.8%) |
|
TSI (+) TBI (+), (%) |
15 (36.6%) |
|
TSI(-) TBI(-), (%) |
17 (41.5%) |
|
T3: Triiodothyronine; T4: Thyroxine; TSH: Thyroid-stimulating hormone TSI: Thyroid stimulatory antibody; TBI: Thyrotropin-binding inhibitory immunoglobulin. Data are presented as mean ± SD. |
|
In addition, patients were divided into two groups according to TRAb positivity at the beginning of the treatment. TSH receptor antibody was positive in 24 (58.5%) and negative in 17 (41.5%) patients. All of the patients who were found to be TRAb positive at the start of the treatment became negative, while there was no statistically significant difference between the mean pre-treatment and 18th-month serum TSH levels of the two groups (p> 0.05), there was a difference between the mean serum free T4 and T3 levels (p = 0.047 and p = 0.009 for pre-treatment; p = 0.024 and p = 0.050 for 18th month, respectively). Although not statistically significant, remission rate in the 18th month of the treatment was 64.7% in the TRAb negative group, while this rate remained at 41.7% in the TRAb positive group (p=0.146). The time to reach remission was longer in the group with positive TRAb, which is again not statistically significant. There was a significant difference between the groups regarding the cumulative doses of methimazole used until remission (p <0.001) (Table III).
DISCUSSION
In the present study, third-generation TRAb positivity were found to be associated with a lower rate of remission during the 18-month treatment period compared to TRAb negative patients with Graves' disease and also, the cumulative methimazole dose requirement was higher in antibody positive patients.
Methimazole is an anti-thyroid drug which inhibits serum free T3 -T4 synthesis by the mechanisms of inhibiting thyroid peroxidase and slowing the oxidation of iodide in the thyroid.14 It is thought to have an impact on inhibiting antibody synthesis from B lymphocytes, lowering the TSH receptor antibody level, and improving the function of suppressor T cells.15 Apart from antithyroid drugs, among the factors affecting the prognosis and remission rates, it was emphasised that age, gender, duration of symptoms before starting treatment, dosage of anti-thyroid drugs, size of goiter, presence of ophthalmopathy and severity of hyperthyroidism are also important.16,17
Table II: Data of patients according to remission status at 18th month.|
|
The group not in remission in the 18th month (n:20) |
The group in remission in the 18th month (n:21) |
P |
|
|
Age, years |
38.7±14.9 |
35±8.0 |
0.333a |
|
|
Sex (female/male %) |
13(65%) / 7(35%) |
17(81%) / 4(19%) |
0.249d |
|
|
Smokers (+) |
1(5%) |
4(19%) |
0.343c |
|
|
Anti-TPO (+) |
19(95%) |
20(95.2%) |
>0.999c |
|
|
Anti-Tg (+) |
13(65%) |
17(81%) |
0.249d |
|
|
TSH Receptor Antibody at the Time of Diagnosis |
TSI (+) |
4(20%) |
1(4.8%) |
0.023b |
|
TBI (+) |
4(20%) |
0(0%) |
||
|
TSI (+), TBI (+) |
6(30%) |
9(42.9%) |
||
|
TSI(-), TBI(-) |
6(30%) |
11(52.4%) |
||
|
Pre-treatment TSH (mIU/L) |
0.030±0.063 |
0.003±0.003 |
0.071a |
|
|
Pre-treatment free T4 (ng/dL) |
2.4±2.1 |
2.1±1.3 |
0.553a |
|
|
Pre-treatment free T3 (ng/dL) |
9.0±6.2 |
7.8±5.1 |
0.508a |
|
|
TSH at 18th month (mIU/L) |
1.72±1.45 |
2.23±1.38 |
0.253a |
|
|
Free T4 at 18th month (ng/dL) |
0.81±0.19 |
0.87±0.17 |
0.264a |
|
|
Free T3 at 18th month (ng/dL) |
3.28±1.09 |
3.32±0.48 |
0.869a |
|
|
Cumulative metimazole dose (mg) at remission date |
2909.8±705.2 |
2639.3±824.5 |
0.267a |
|
|
a: Independent t test, b: Likelihood ratio test, c: Fisher’s Exact test, d: Pearson Chi-square test. Data are presented as mean ± SD. |
||||
Table III: Data of patients according to TSH receptor antibody.
|
|
TSH Receptor Antibody (+) (n:24) |
TSH Receptor Antibody (-) (n:17) |
p
|
|
Age, years |
39.7±13.9 |
32.8±6.8 |
0.042a |
|
Sex (female/male %) |
17(70.8%) / 7(29.2%) |
31(76.5%) / 4(23.5%) |
0.736b |
|
Smokers (+) |
5(20.8%) |
0(0%) |
0.065b |
|
Anti-TPO (+) |
24(100%) |
15(88.2%) |
0.166b |
|
Anti-Tg (+) |
20(83.3%) |
10(58.8) |
0.151b |
|
Pre-treatment TSH (mIU/L) |
0.008±0.022 |
0.027±0.065 |
0.254a |
|
Pre-treatment free T4 (ng/dL) |
2.68±1.76 |
1.63±1.41 |
0.047a |
|
Pre-treatment free T3 (ng/dL) |
10.10±6.61 |
6.00±2.48 |
0.009a |
|
TSH at 18th month (mIU/L) |
1.87±1.48 |
2.13±1.35 |
0.555a |
|
Free T4 at 18th month (ng/dL) |
0.89±0.20 |
0.76±0.12 |
0.024a |
|
Free T3 at 18th month (ng/dL) |
3.51±0.77 |
3.00±0.83 |
0.050a |
|
Remission at 18th month |
10 (41.7%) |
11 (64.7%) |
0.146c |
|
Methimazole cumulative dose until remission (mg) at remission date |
3418.8± 903.5 |
2461.8± 505.4 |
<0.001a |
|
Time to reach remission (month) |
20.8± 3.3 |
20.1± 2.9 |
0.466a |
|
a: Independent t test, b: Fisher’s Exact test, c; Pearson Chi-square test. Data are presented as mean ± SD. |
|||
Furthermore, it is known that the measurement of TRAb is beneficial for predicting remission and relapse.7 By using third generation measurement methods, human monoclonal TSI and TBI are measured separately. Significant decrease in TSI and TBI levels and improvement in terms of remission of the disease and prevention of relapse have been experienced, particularly with methimazole treatment.14,18 On the other hand, there are publications emphasising that measuring TRAb separately as TSI and TBI will not be useful.19 Therefore, although the patients in this study were evaluted as having stimulant and blocker antibody separately, the authors considered them as a single group when commenting on remission in 18 months. It was found that those patients, who were evaluated as a single group of having TRAb, had longer time to go into remission and their cumulative methimazole dose requirement was higher when compared to those without TRAb. Beyond that, institution of uniform titration schedule by physicians who adjusted the treatment dose at the beginning and during the follow-up enabled the cumulative dose calculation to be objective in the current study.
In patients with Graves' disease, especially those with severe thyrotoxicosis, the methimazole dose required to maintain a normal free T4-T3 level for a long time is much lower than the initial therapeutic dose required to normalize the free T4-T3 level. That is, the dose of methimazole required to maintain normal free T4-T3 level is lower than the dose required to normalize free T4-T3 level. This method of tapering treatment is a frequently used strategy in steroid and cabergoline treatments. The methimazole dose reduction strategy can be recommended to all patients whose free T3-T4 levels returned to normal. Subsequent methimazole tapering is almost always successful, even when very high initial doses are required. In this study, cumulative dose calculation was made using the tapering strategy. It has been shown that remission was achieved by using methimazole treatment with tapering strategy in a mean of 20.5 ± 3.1 months. Of note, this study once again proved that methimazole can be used effectively to treat hyperthyroidism.
The main limitation of this study is selection bias, resulting from single center and retrospective design of the work. The second is the small sample size and the absence of control group.
CONCLUSION
Clinical evaluation of the duration of remission and cumulative methimazole therapy in patients with Graves' disease revealed that TRAb positivity at the beginning of the treatment is a non-favourable factor in achieving remission.
ETHICAL APPROVAL:
The study was approved by Institutional Board of Adıyaman University Training and Research Hospital (2-20/2019); and competent authorities of the participating centre, and the trial complied with the Declaration of Helsinki.
PATIENTS’ CONSENT:
Because this study was retrospective, the patients’ consent was waived.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
SÖ, MÇ, AV and BA: Conceived the study design, involved in data collection, performed the statistical analysis, interpreted data and prepared the manuscript draft.
MÇ and HG: Critically reviewed the final version of the manuscript and approved it for publication.
REFERENCES
- Bahn Chair RS, Burch HB, Cooper DS, Garber JR, Greenlee MC, Klein I, et al. Hyperthyroidism and other causes of thyrotoxicosis: Management guidelines of the american thyroid association and american association of clinical endocrinologists. Thyroid 2011; 21(6):593-646. doi: 10.1089/thy.2010. 0417.
- Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American thyroid association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid 2016; 26(10): 1343-421. doi: 10.1089/thy. 2016.0229.
- Kahaly G, Bartalena L, Hegedüs L, Leenhardt L, Poppe K, Pearce S. 2018 European thyroid association guideline for the management of Graves’ Hyperthyroidism. European Thyroid J 2018;7(4):167-86. doi: 10.1159/000490384.
- Struja T, Fehlberg H, Kutz A, Guebelin L, Degen C, Mueller B, et al. Can we predict relapse in Graves’ disease? Results from a systematic review and meta-analysis. European J Endocrinol 2017; 176(1): 87-97. doi: 10.1530/EJE-16-0725.
- Sundaresh V, Brito JP, Wang Z, Prokop LJ, Stan MN, Murad MH, et al. Comparative effectiveness of therapies for Graves' Hyperthyroidism: A systematic review and network meta-analysis. J Clinical Endocrinol Metabolism 2013; 98(9):3671-7. doi: 10.1210/jc.2013-1954.
- Abraham P, Avenell A, McGeoch SC, Clark LF, Bevan JS. Antithyroid drug regimen for treating Graves' hyperthyroidism. Cochrane Database of Systematic Reviews 2010; 20(1): 43-59. doi: 10.1002/14651858.CD003420.pub4.
- Kamath C, Adlan MA, Premawardhana LD. The role of thyrotrophin receptor antibody assays in Graves’ disease. J Thyroid Res 2012; (525936):1-8. doi: 10.1155/2012/ 525936.
- Davies TF, Roti E, Braverman LE, DeGroot LJ. Thyroid controversy- stimulating antibodies. J Clin Endocrinol Metab 1998; 83(11):3777-85. doi: 10.1210/jcem.83.11.5056-1.
- Michalek K, Morshed SA, Latif R, Davies TF. TSH receptor autoantibodies. Autoimmunity Reviews 2009; 9(2):113-6. doi: 10.1016/j.autrev.2009.03.012.
- Massart C, Sapin R, Gibassier J, Agin A, D’Herbomez M. Intermethod variability in TSH-receptor antibody measurement: implication for the diagnosis of Graves disease and for the follow-up of Graves ophthalmopathy. Clin Chem 2009; 55(1):183-6. doi: 10.1373/clinchem.2008.115162.
- Theodoraki A, Jones G, Parker J, Woolman E, Martin N, Perera S, et al. Performance of a third-generation TSH-receptor antibody in a UK clinic. Clin Endocrinol (Oxf) 2011; 75(1): 127-33. doi: 10.1111/j.1365-2265.2011.04022.x.
- Kwon H, Kim WG, Jang EK, Kim M, Park S, Jeon MJ, et al. Usefulness of measuring thyroid stimulating antibody at the time of antithyroid drug withdrawal for predicting relapse of Graves Disease. Endocrinol Metab (Seoul) 2016; 31 (2):300-10. doi: 10.3803/EnM.2016.31.2.300.
- Okamoto Y, Tanigawa SI, Ishikawa K, Hamada N. TSH receptor antibody measurements and prediction of remission in Graves' disease patients treated with minimum maintenance doses of antithyroid drugs. Endocr J 2006; 53 (4): 467-72. doi: 10.1507/endocrj.k05-121.
- Zhao H, Chu N , Han J, Wang F. Effect of methimazole on serum tsab and tbıı levelsin patients with Graves' Hyperthyroidism. Acta Medica Mediterranea 2020; 36(4): 2207-21. doi 10.19193/0393-6384_2020_4_344.
- Kafrouni Gerges AR, Clark SN, Shawa H. Hypothyroidism to hyperthyroidism: An immunological pendulum swing from two extreme poles - a case series. BMJ Case Rep 2019; 12(4):e227445. doi: 10.1136/bcr-2018-227445.
- Ishtiaq O, Waseem S, Haque MN, Islam N, Jabbar A. Remission of Grave's disease after oral anti-thyroid drug treatment. J Coll Physicians Surg Pak 2009; 19(11):690-3.
- Schott M, Morgenthaler NG, Fritzen R, Feldkamp J, Willenberg HS, Scherbaum WA, et al. Levels of autoantibodies against human TSH receptor predict relapse of hyperthyroidism in Graves' disease. Horm Metab Res 2004; 36(2): 92-6. doi: 10.1055/s-2004-814217.
- Mazza E, Carlini M, Flecchia D, Blatto A, Zuccarini O, Gamba S, et al. Long-term follow-up of patients with hyperthyroidism due to Graves’ disease treated with methimazole. Comparison of usual treatment schedule with drug discontinuation vs continuous treatment with low methimazole doses: a retrospective study. J Endocrinol Invest 2008; 31(10):866-72. doi: 10.1007/BF03346433.
- Quadbeck B, Hoermann R, Hahn S, Roggenbuck U, Mann K, Janssen OE. Binding, stimulating and blocking TSH receptor antibodies to the thyrotropin receptor as predictors of relapse of Graves’ disease after withdrawal of antithyroid treatment. Horm Metab Res 2005; 37(12):745-50. doi: 10.1055/s-2005-921102.