Whole-body Bone Scan in the Diagnosis and Treatment of SAPHO Syndrome
By Chengzhi Jinag1, Yajie Zhao2, Xinhui Li2, Hui Hu2, Can Li2Affiliations
doi: 10.29271/jcpsp.2022.04.64ABSTRACT
Synovitis, acne, pustulosis, hyperostosis, and osteomyelitis (SAPHO) syndrome is rare disease of unknown pathogenesis. Its diagnosis and treatment are difficult. There is no standardised treatment for SAPHO syndrome, and the results of empirical therapy are unpredictable. The whole-body bone scan may help evaluate the efficacy of SAPHO syndrome treatment. The case of a 52-year Chinese male, affected by SAPHO syndrome, is presented and discussed in this report. After the patient received methotrexate, prednisone and non-steroidal anti-inflammatory drugs (NSAIDs) for six months, his clinical symptoms and whole body bone scan signs improved.
Key Words: SAPHO syndrome, Whole-body bone scintigraphy, Treatment efficacy.
INTRODUCTION
Synovitis, acne, pustulosis, hyperostosis, and osteomyelitis (SAPHO) syndrome is a rare clinical entity involving musculoskeletal and dermatologic systems.1 The main clinical features are chronic inflammatory osteoarthritis and dermatosis. Chest wall pain, more common in the sternoclavicular joints, along with palmoplantar pustulosis and acne can point to this uncommon syndrome.2 Herein, we report a case of a Chinese male, who was diagnosed as SAPHO syndrome and received methotrexate, prednisone and non-steroidal anti-inflammatory drugs (NSAIDs) for more than six months. Subsequently, his clinical symptoms and whole-body bone scan signs improved.
CASE REPORT
In September 2017, a 52-year Chinese male patient was admitted to our hospital with complaints of pain and swelling in the anterior chest wall and lumbago regions for eight months, without skin lesions.
Physical examination revealed pustulosis on the face, palms and soles. The laboratory evaluation revealed red blood cell count of 4.01×1012/L (reference range: 4.3-5.8×1012/L), hemoglobin 113 g/L (reference range: 130-175g/L), platelet count 362×109/L (reference range: 125-350×109/L), erythrocyte sedimentation rate (ESR) 120 mm/h (reference range: 0-20 mm/h), C-reactive protein (CRP) 95.2 mg/L (reference range: 0–7.44 mg/L) and interleukin-6, 39.9 pg/ml (reference range: 0-5.9 pg/ml).
In addition, coagulation function, liver and renal functions, rheumatoid factor, lupus and other autoimmune disease-specific antibodies were all in normal ranges.
Positron emission tomography-computed tomography (PET-CT) showed bone destruction or increased bone density in bilateral sternoclavicular joints, bilateral clavicles, sternum, right first to third ribs, left first to sixth ribs, and abnormal increase of FDG uptake (SUVmax, 3.4); at the same time, no other malignant solid tumors were found by PET-CT imaging (Figure1). In order to understand the metabolism of the whole body, the whole-body bone imaging was further performed. Whole-body bone scintigraphy (Figure 2a) revealed increased tracer uptake in bilateral sternoclavicular joints, bilateral clavicles, sternum, right first to third ribs, left first to sixth ribs and fourth lumbar vertebrae. The characteristic “bull-head” sign raised suspicion of SAPHO syndrome. According to the diagnostic criteria of Benhamou et al., SAPHO syndrome was finally diagnosed.1
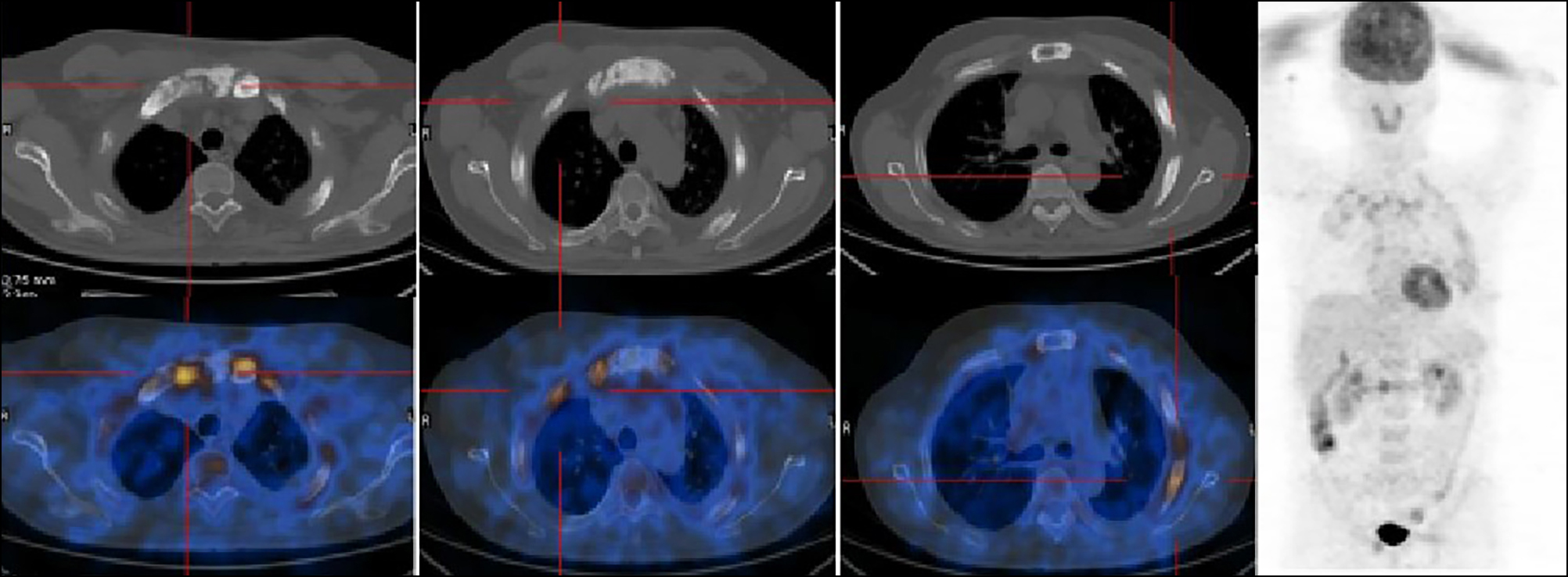 Figure 1: Positron emission tomography-computed tomography (PET-CT) with 18F-FDG showed bone destruction or osteosclerosis and increased tracer uptake in bilateral sternoclavicular joint, bilateral clavicles, sternum and multiple rib joints (SUVmax, 3.4).
Figure 1: Positron emission tomography-computed tomography (PET-CT) with 18F-FDG showed bone destruction or osteosclerosis and increased tracer uptake in bilateral sternoclavicular joint, bilateral clavicles, sternum and multiple rib joints (SUVmax, 3.4).
The patient was treated with methotrexate, 20 mg/week, prednisone, 10 mg/day and calcium tablet, 1 g/day. The NSAID drug, diclofenac, 150 mg/day, was added to the treatment, which improved the anterior chest wall and lumbago pain. After six months, the CRP level and ESR returned to normal. At the same time, the patient stopped taking medicine on his own initiative due to alleviation of the anterior chest wall and lumbago pain. In order to further evaluate the changes of bone metabolism, whole-body bone imaging was performed again. The whole-body bone scan showed decreased uptake of 99mTc-MDP in the right first to third ribs, left first to sixth ribs and fourth lumbar vertebra (Figure 2b). Single photon emission computed tomography–computed tomography (SPECT-CT) scan was performed to further evaluate bone density changes. Fused SPECT-CT coronal and axial images (Figure 3) showed that the destructive, expansile, osteolytic and osteosclerotic lesions of the sternum, and bilateral ribs were improved.
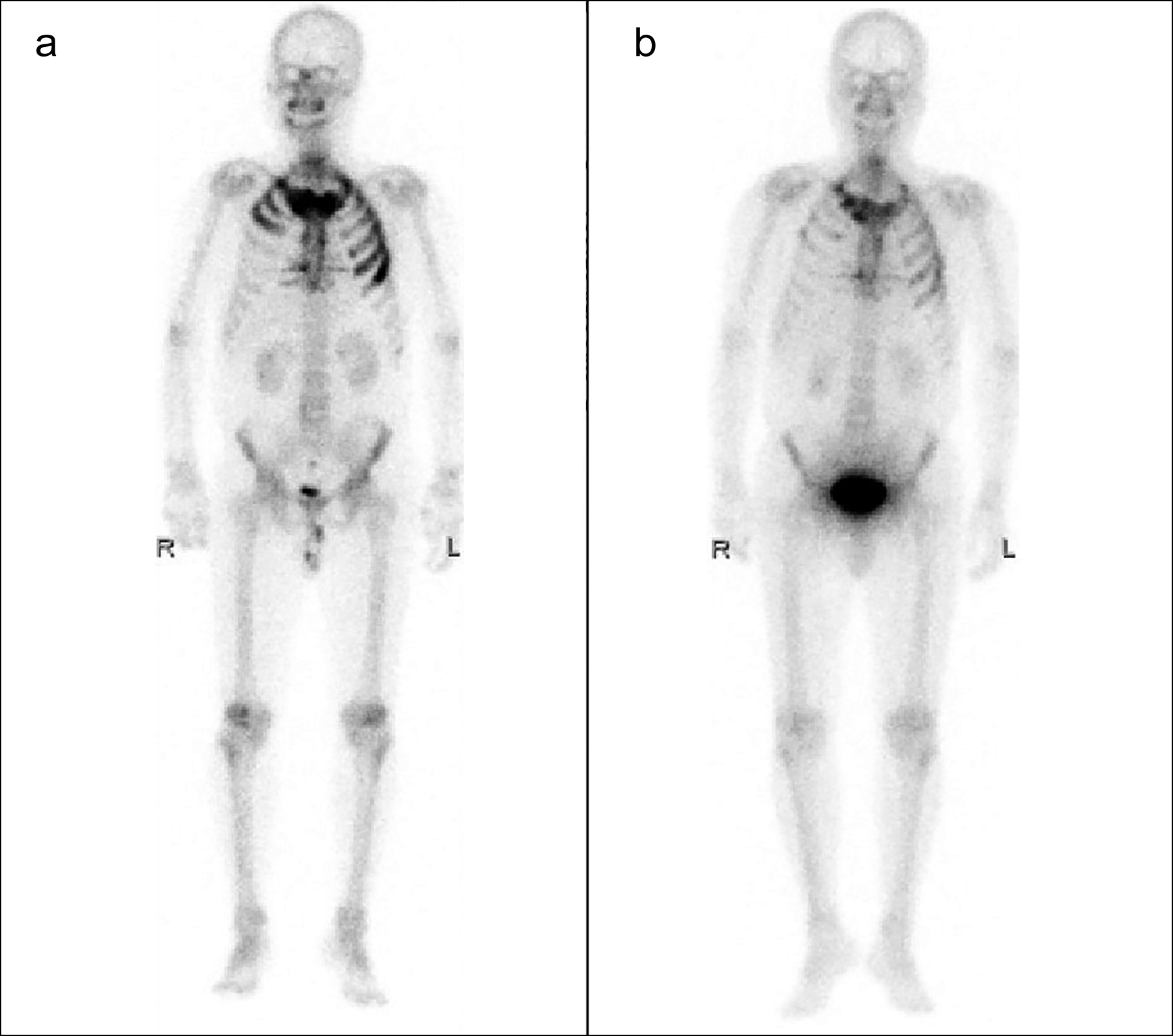 Figure 2: Whole-body bone scan with 99mTc-MDP images before and after treatment. a) Increased tracer uptake in bilateral sternoclavicular joints, bilateral clavicles, sternum, right first to third ribs, left first to sixth ribs and fourth lumbar vertebra. b) decreased tracer uptake of original lesions.
Figure 2: Whole-body bone scan with 99mTc-MDP images before and after treatment. a) Increased tracer uptake in bilateral sternoclavicular joints, bilateral clavicles, sternum, right first to third ribs, left first to sixth ribs and fourth lumbar vertebra. b) decreased tracer uptake of original lesions.
 Figure 3: Fused SPECT-CT coronal and axial images (a-d) show the destructive, expansile, osteolytic and sclerotic lesions of the sternum, and bilateral ribs have improved.
Figure 3: Fused SPECT-CT coronal and axial images (a-d) show the destructive, expansile, osteolytic and sclerotic lesions of the sternum, and bilateral ribs have improved.
DISCUSSION
Chamot et al.,2 were the first group who proposed the name of SAPHO syndrome in 1987. Whole-body bone scan is a highly sensitive examination method for chest wall lesions in patients with SAPHO syndrome. The pattern of increased tracer uptake in the anterior chest wall may resemble a “bull’s head”, which is the characteristic sign of SAPHO syndrome in bone scans.3
18F-FDG PET/CT may be another useful method, which could find more lesions or concealed lesions. The increase of FDG uptake in the anterior chest wall may precede the appearance of skin lesions and the appearance of obvious abnormality on X-rays. In the advanced stages of SAPHO syndrome, PET/CT is helpful to distinguish active from inactive bone lesions. In our case, this patient had PET/CT scan first, which showed that the lesions had low to moderate 18F-FDG uptake, which was not typical enough to diagnose SAPHO syndrome. The reason of different uptake of imaging agent in PET/CT may be the co-existence of osteolysis and osteosclerosis, which is another feature of SAPHO syndrome. Then, the patient underwent a whole-body bone scan, which revealed the “bull’s head” sign and high uptake of multiple rib joints. Leone et al.4 have reported that 60–95% bone destructions, which comprise hyperostosis, osteolysis, osteitis, and osteosclerosis, occurred in the area of anterior chest wall, especially in the costochondral and sternoclavicular joints and spine. In our case, the bone scan revealed intense uptake in bilateral sternoclavicular joints, bilateral clavicles, sternum, right first to third ribs, left first to sixth ribs and fourth lumbar vertebra, which were consistent with the above results.
Although there are many researches on the disease, effective treatment is still limited. The current treatment goal for this disease is to relieve symptoms. Skin lesions, such as pustulosis palmaris and plantaris, are difficult to distinguish from psoriasis rash.5 However, for highly active bone and joint damage (erosion, hyperosteogeny and osteoarthritis), long-term use of methotrexate can achieve satisfactory results.6 There are several studies which have proved that the use of steroids and methotrexate may obtain an effective treatment result in inhibiting bone damage.7-9 In our case, after six months of treatment with methotrexate, 20 mg/week, the patient felt much better than before, and two years later, the whole-body bone scintigraphy showed decreased uptake by all lesions. This case, on the one hand, has proved the positive effect of methotrexate on the bone damage of SAPHO syndrome; and on the other hand, it has also effectively proved that bone scanning plays an important role in the evaluation of the therapeutic effect in this disease. However, at present, the treatment of SAPHO syndrome is not standardised and has some challenges, such as optimum dose and duration of treatment and compliance by the patients. Therefore, an appropriate treatment plan and regular follow-up are particularly important. Future research should focus on defining the optimum and effective treatment regimen for this uncommon disease.
ACKNOWLEDGEMENTS:
The authors acknowledge financial support from the Hunan Department of Science and Technology Foundation [Grant No. 2018JJ3827]; China Scholarship Council support [File No. 201906375015].
PATIENT’S CONSENT:
Informed consent was obtained from the patient to publish the data regarding this case.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
CJ: Designed and authored the manuscript.
YZ: Provided concept of the manuscript and proofread the final version before submission and performed the procedure.
XL: Contributed in analysis, acquisition, revision and final proof.
HH: Data collection, and literature review.
CL: Collected the pathological findings and follow-up of the patient.
REFERENCES
- Benhamou CL, Chamot AM, Kahn MF. Synovitis-acne-pustulosis hyperostosis-osteomyelitis syndrome (SAPHO). A new syndrome among the spondyloarthropathies? Clin Exp Rheumatol 1988; 6(2):109-12.
- Chamot AM, Benhamou CL, Kahn MF, Beraneck L, Kaplan G, Prost A. Acne-pustulosis-hyperostosis-osteitis syndrome. Results of a national survey. 85 cases. Rev Rhum Mal Osteoartic 1987; 54(3):187-96.
- İlgen U, Turan S, Emmungil H. Bull's head sign in a patient with SAPHO syndrome. Balkan Med J 2019; 36(2):139-40. doi: 10.4274/balkanmedj.galenos.2018.2018.1630.
- Leone A, Cassar-Pullicino VN, Casale R, Magarelli N, Semprini A, Colosimo C. The SAPHO syndrome revisited with an emphasis on spinal manifestations. Skelet Radiol 2015; 44(1):9-24. doi: 10.1007/s00256-014-2025-0.
- Li C, Wu X, CaoY, ZengY, ZhangW, Zhang S, et al. Paradoxical skin lesions induced by anti-TNF-α agents in SAPHO syndrome. Clin Rheumatol 2019; 38(1):53-61. doi: 10.1007/s10067-018-4083-5.
- Axmann R, Bohm C, Kronke G, Zwerina J, Smolen J, Schett G. Inhibition of interleukin-6 receptor directly blocks osteoclast formation in vitro and in vivo. Arthritis Rheum 2009; 60(9):2747-56. doi: 10.1002/art.24781.
- Zwaenepoel T, Vlam K. SAPHO: Treatment options including bisphosphonates. Semin Arthritis Rheum 2016; 46(2): 168-73. doi: 10.1016/j.semarthrit.2016.04.004.
- Vekic DA, Woods J, Lin P. Cains GD. SAPHO syndrome associated with hidradenitis suppurativa and pyoderma gangrenosum successfully treated with adalimumab and methotrexate: A case report and review of the literature. Int J Dermatol 2018; 57(1):10-8. doi: 10.1111/ijd.13740.
- Akçaboy M, Bakkaloglu-Ezgu SA, Buyukkaragoz B, Isıyel E, Kandur Y, Hasanoglu E, et al. Successful treatment of a childhood synovitis, acne, pustulosis, hyperostosis and osteitis (SAPHO) syndrome with subcutaneous methotrexate: A case report. Turk J Pediatr 2017; 59(2): 184-8. doi: 10.24953/turkjped.2017.02.011.