The Fate of Coracoid Graft after Latarjet Procedure: Arthroscopic and Open Findings of Graft Union and Glenoid Remodelling
By Mohd Nizlan1, Raymond Yeak Dieu Kiat1, Ahmad Hisham Rashid2Affiliations
doi: 10.29271/jcpsp.2022.10.1356ABSTRACT
Successful Latarjet procedures depend on many factors including graft union and subsequent restoration of the glenoid surface. Coracoid graft union has been studied; however, remodelling of the glenoid has not been studied extensively. We present two Latarjet cases in which coracoid screws were removed due to hardware issues, at 12 months postoperatively in one patient and at six months in another. We share our observations on the coracoid graft and the restoration of the glenoid shape. Prior to screw removal, done by a mini-open approach, we performed arthroscopic examination of the glenohumeral joint in both patients. Our arthroscopic and open findings with respect to graft union, screw prominence, and glenoid remodelling, are presented. Both cases showed good union of the coracoid graft and restoration of the native glenoid shape.
Key Words: Shoulder dislocation, Surgery, Complications, Coracoid process.
INTRODUCTION
Latarjet surgery is a coracoid grafting procedure commonly performed to overcome significant bone loss on the glenoid surface from recurrent dislocation. This procedure is considered one of the most successful treatment options for recurrent anterior shoulder instability.1 To date, both arthroscopic and open techniques have proved effective, with good and comparable outcomes.2 Graft union in Latarjet procedure has been studied, with more than 90% union rate.3 Question remains whether the united graft will remodel to restore the original shape of the native glenoid. We report two cases in which fixation screws were noted to be prominent posteriorly in one case, and screw-head became prominent postoperatively in the other, causing pain, recurrence of instability, or clicking. Screw removal was done for both cases due to hardware issues.
CASE 1:
A 29-year male medical officer presented with recurrent dislocation in his left shoulder. He had dislocated his shoulder more than 20 times.
Computed tomography (CT) showed a bony Bankart lesion with 25% bone loss (Figure 1). He underwent an open Latarjet procedure, accompanied by capsular plication using two SutureTak anchors (Arthrex, Inc) (Figure 2). This combination is the authors’ preferred technique for shoulder stabilisation in patients with more than 20% bone loss. The patient’s immediate postoperative period was uneventful, and he underwent a full range of rehabilitation with good compliance and was asymptomatic for the next eight months.
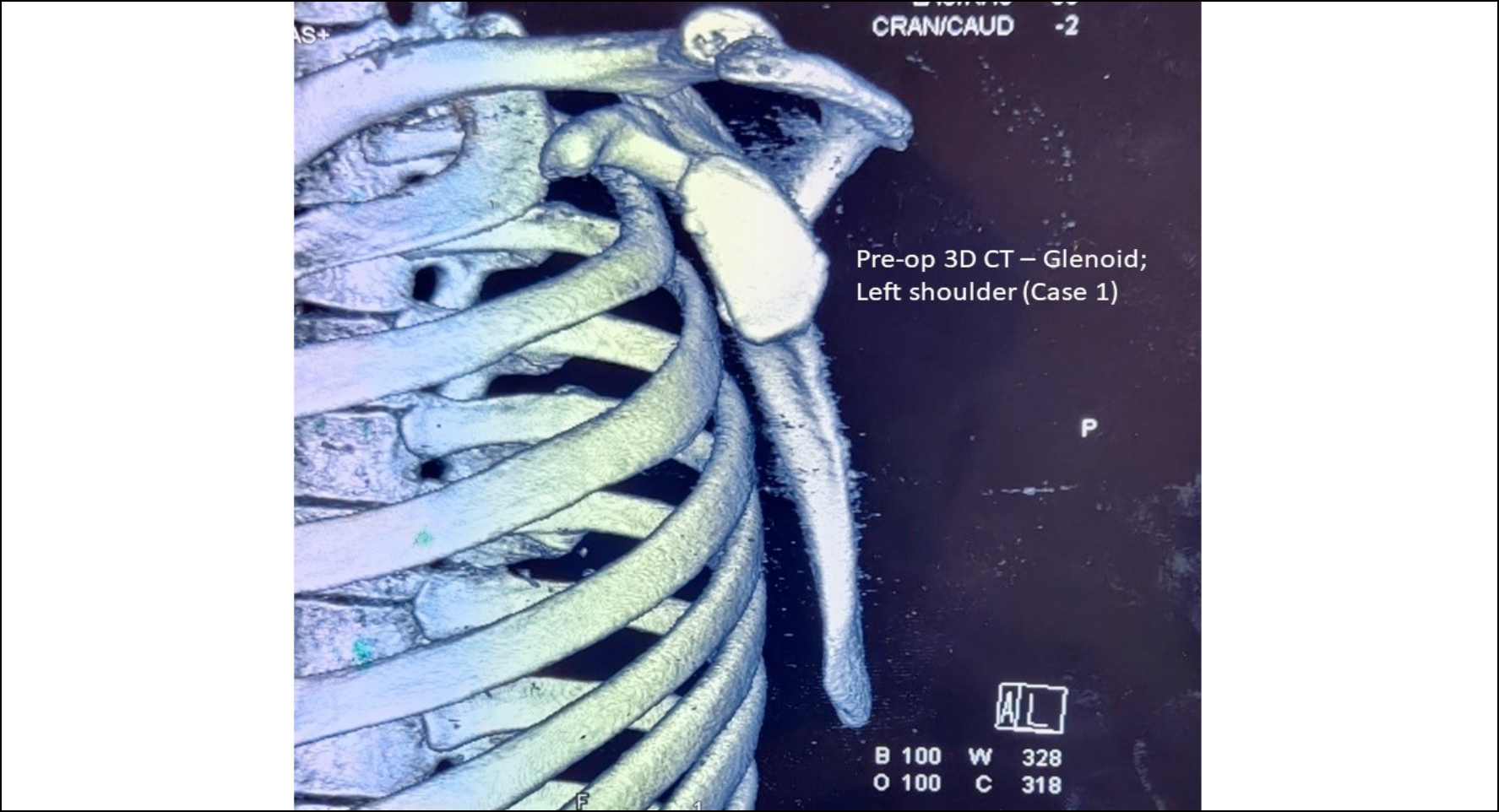 Figure 1: Case 1 – CT (3D) image; Preoperative; left shoulder.
Figure 1: Case 1 – CT (3D) image; Preoperative; left shoulder.
At eighth month, he experienced sudden severe pain and clicking in his left shoulder while performing cardiac compression on one of his patients, and from that incident onward, started to have left shoulder discomfort and clinically showed re-emergence of apprehension on abduction-external rotation position.
Further rehabilitation did not help and repeat CT and magnetic resonance (MR) examinations revealed a united coracoid graft albeit with significant prominence of his inferior screw posteriorly over the glenoid. There was minimal graft resorption, and the screw heads were not prominent over the graft (Figure 3). The MR imaging also showed an intact posterior labrum, ruling out the possibility of multidirectional instability.
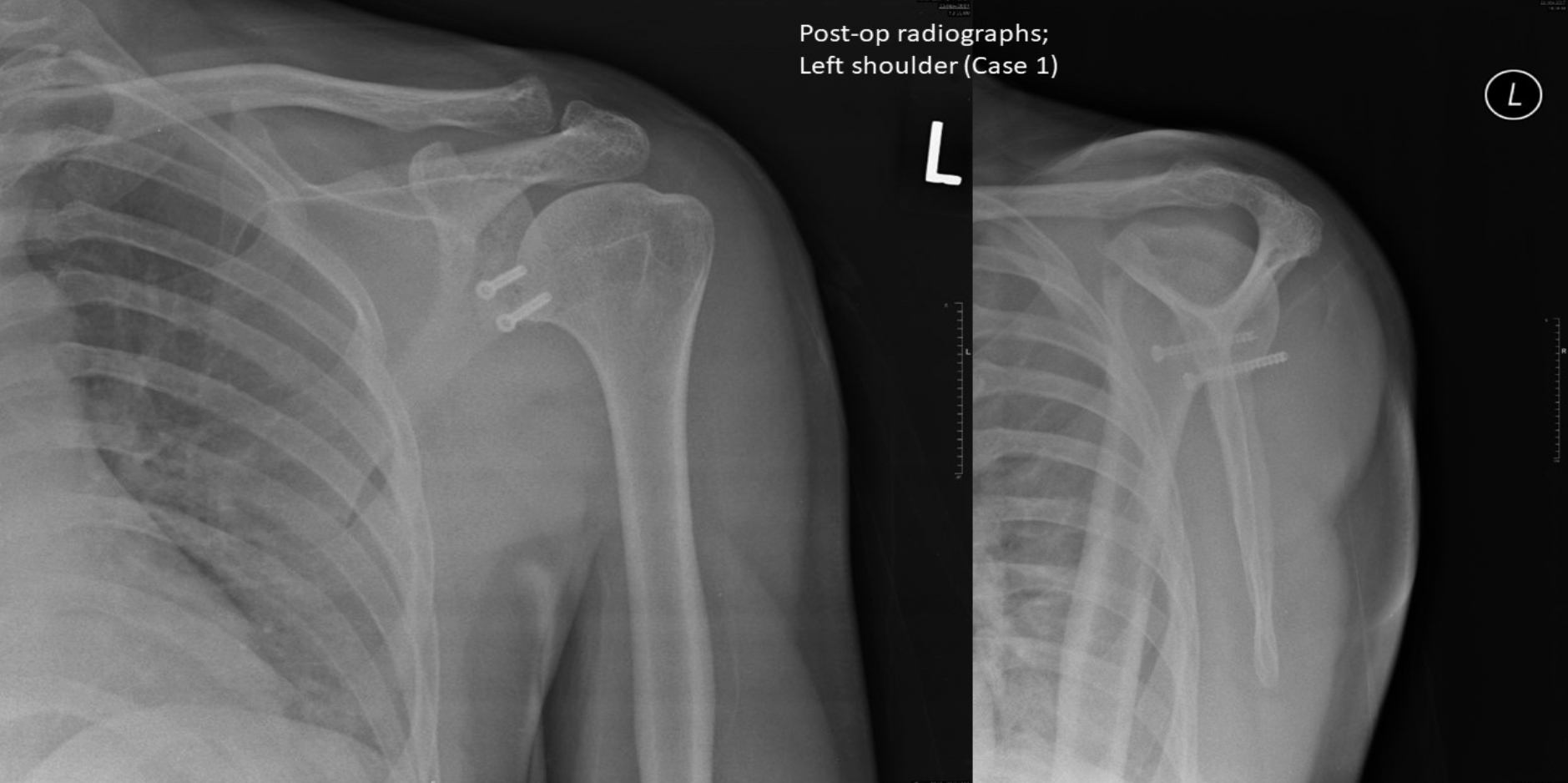 Figure 2: Case 1 – Postoperative radiographs; left shoulder.
Figure 2: Case 1 – Postoperative radiographs; left shoulder.
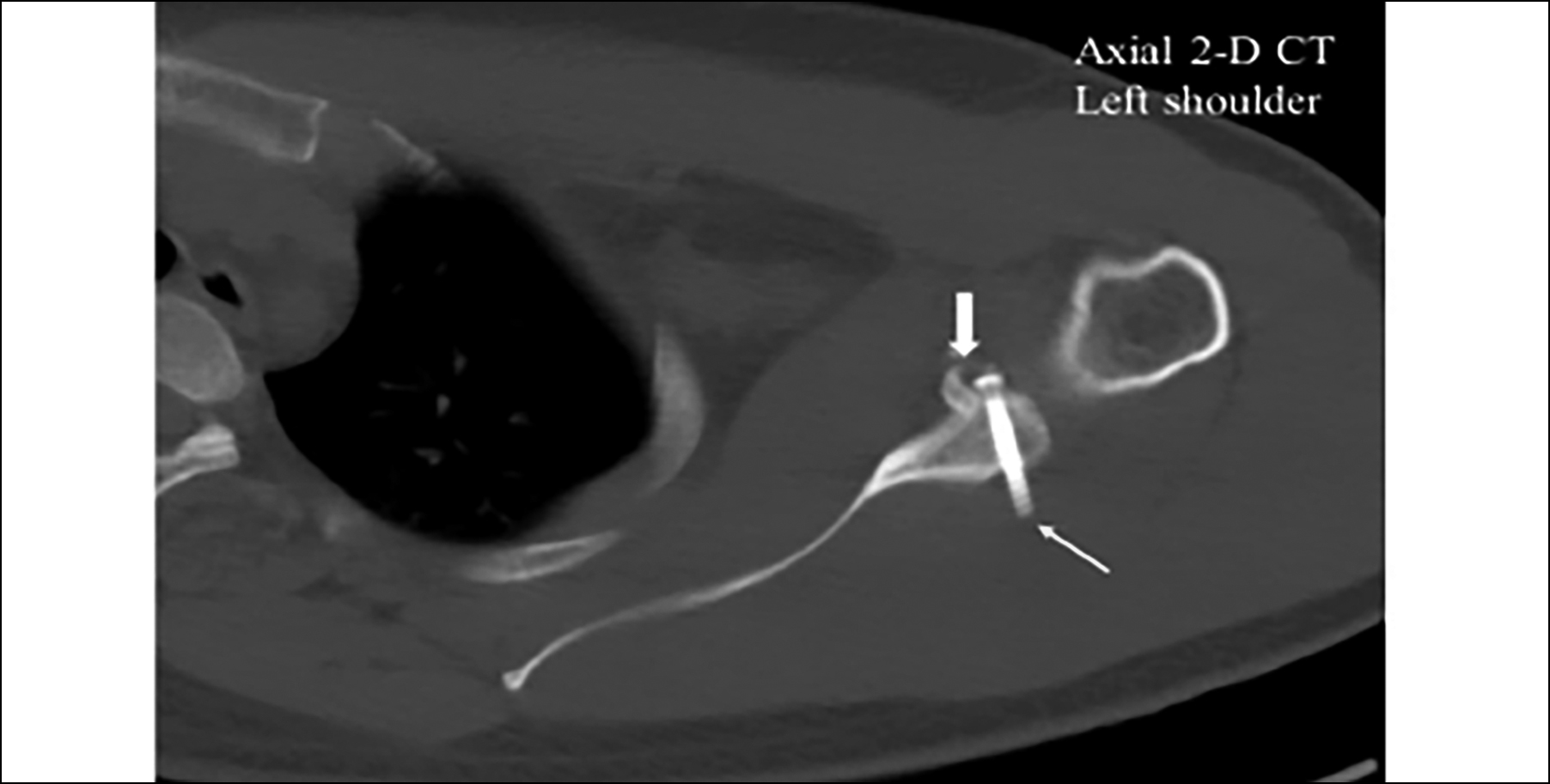 Figure 3: Case 1 – CT (2-D) image; note the united coracoid graft (bold arrow) with posterior prominence of inferior screw (thin arrow); left shoulder.
Figure 3: Case 1 – CT (2-D) image; note the united coracoid graft (bold arrow) with posterior prominence of inferior screw (thin arrow); left shoulder.
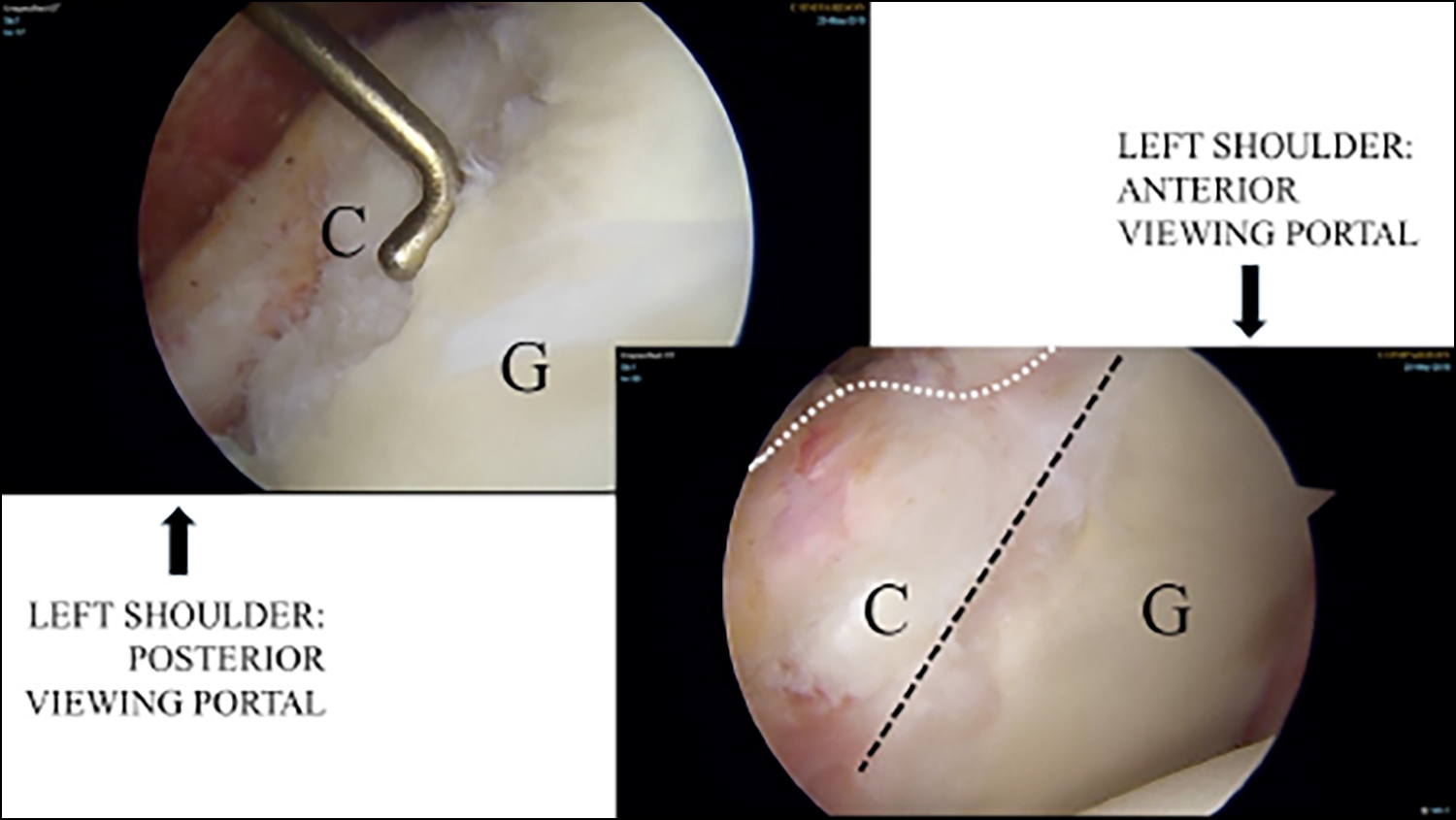 Figure 4: Case1 – Left shoulder arthroscopic image showing the united coracoid graft (C), with glenoid (G) retaining its original shape, as seen from 2 portals – anterior and posterior.
Figure 4: Case1 – Left shoulder arthroscopic image showing the united coracoid graft (C), with glenoid (G) retaining its original shape, as seen from 2 portals – anterior and posterior.
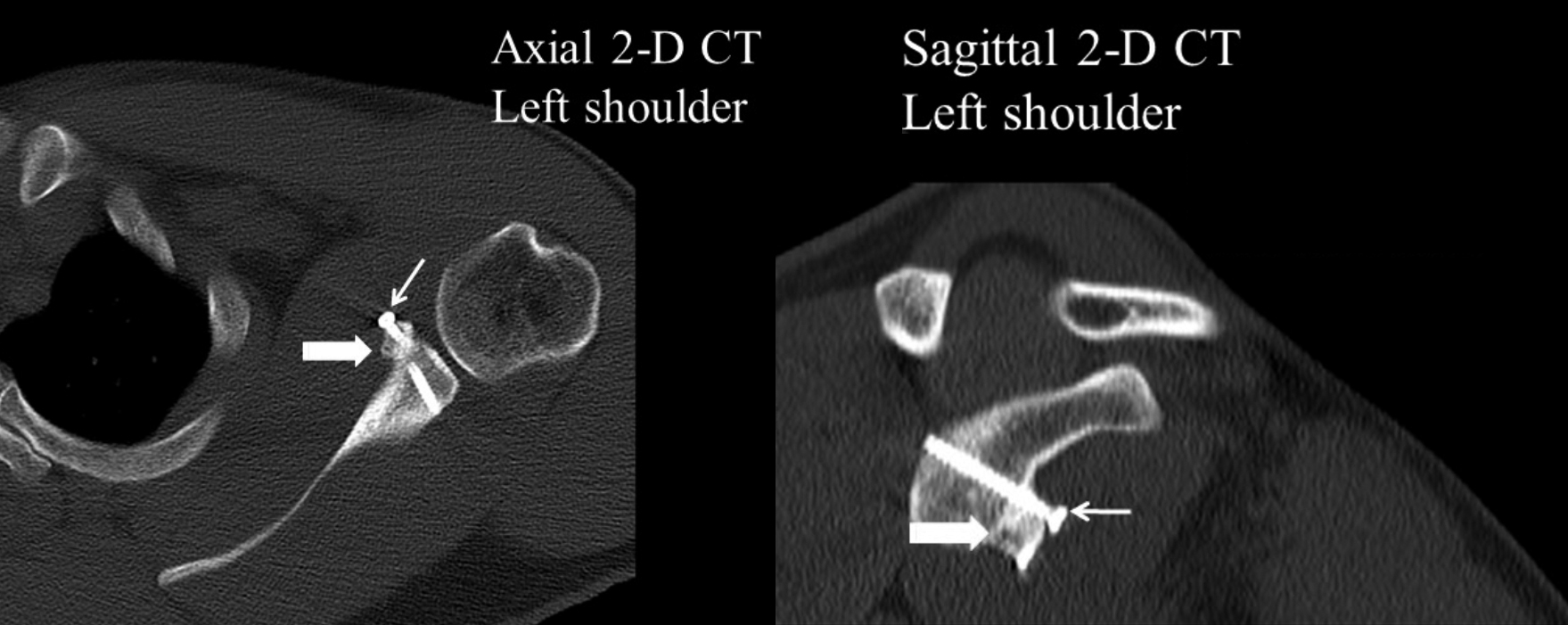 Figure 5: Case 2 – CT (2-D) images; showing united coracoid graft (bold arrow) and prominent proximal screw head (thin arrow); left shoulder.
Figure 5: Case 2 – CT (2-D) images; showing united coracoid graft (bold arrow) and prominent proximal screw head (thin arrow); left shoulder.
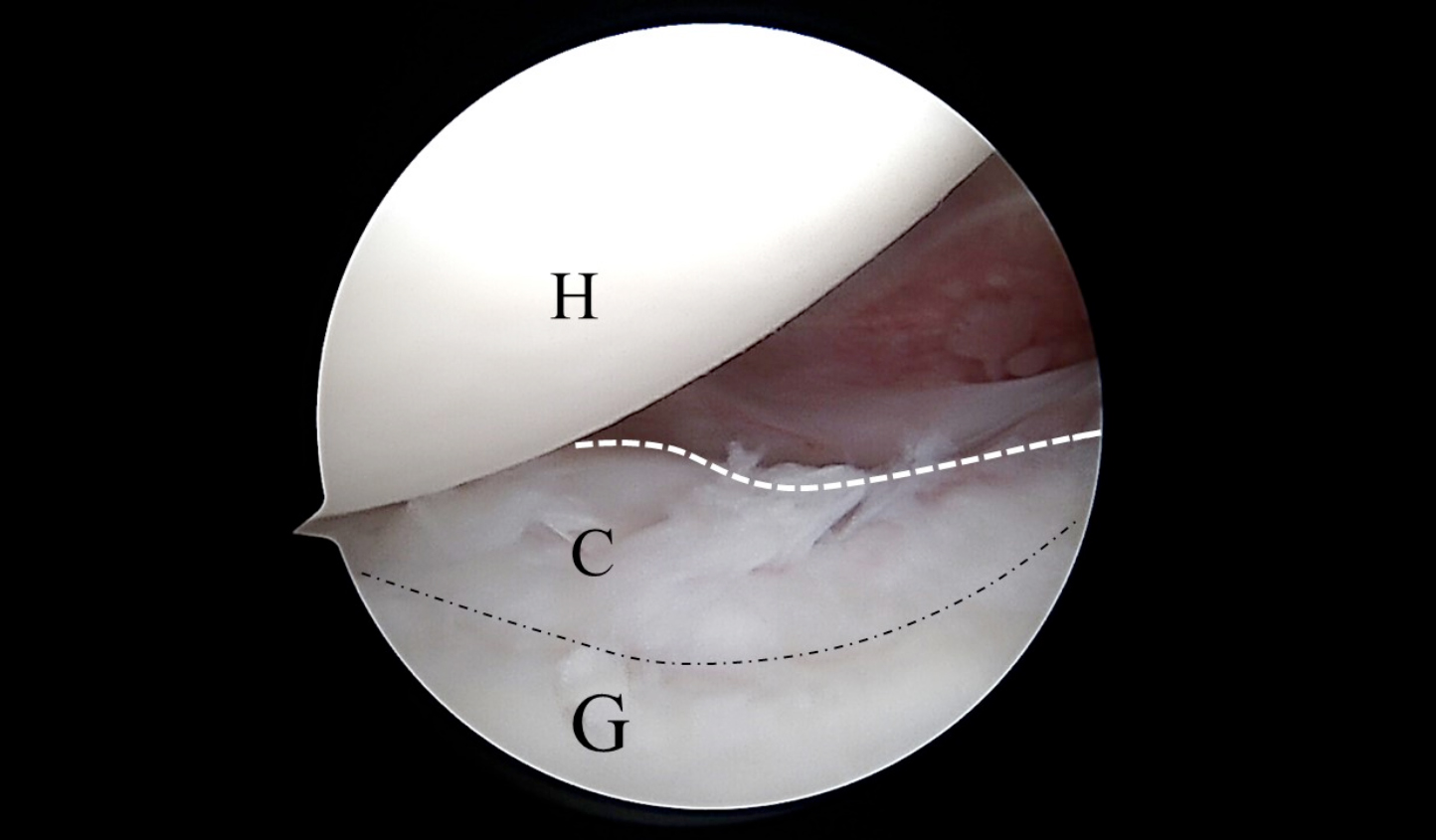 Figure 6: Case 2 – Left shoulder arthroscopic image showing the united coracoid graft (C) to the glenoid (G), and the humeral head (H). The dotted white line indicates curvature representing upper graft resorption, and the dotted black line represents coracoid – the glenoid junction.
Figure 6: Case 2 – Left shoulder arthroscopic image showing the united coracoid graft (C) to the glenoid (G), and the humeral head (H). The dotted white line indicates curvature representing upper graft resorption, and the dotted black line represents coracoid – the glenoid junction.
At one-year, he underwent diagnostic arthroscopy of the left shoulder followed by a mini-open removal of both coracoid screws. Arthroscopy revealed a detached anterior capsule plication with prominent suture remnants within the native glenoid margin. The coracoid graft was noted to be united well, and the glenoid has attained its native shape (Figure 4). There was presence of fibrocartilage-like tissue in between the native cartilage and the remodelled graft. The shoulder did not dislocate at extreme abduction – external rotation position.
Postoperatively, the patient had complete recovery of his pain and the clicking resolved. Instability testing was negative and he was able to get back to work. It was concluded that the pain, clicking, and instability symptoms were due to the prominent inferior screw.
CASE 2:
A 33-year male, an avid bodybuilder, presented with recurrent left shoulder dislocation (>10 times) limiting his gym activities. CT scan revealed significant glenoid bone loss, so he underwent a left shoulder Latarjet, accompanied by capsular plication utilising a single SutureTak anchor. He was well postoperatively and was back at work at postoperative period of six weeks.
At fourth month, he complained of clicking in his left shoulder upon performing alternate abduction – external rotation (ABER) and adduction – internal rotation (ADIR) manoeuvres at the gym. There was no accompanying pain. Even though there was no pain, the clicking was causing him discomfort and he was reluctant to perform rigorous routine during his gym sessions. Clinically, the range of motion was good with no clicks on passive movements; the clicking was only palpable on active ABER and ADIR. The apprehension test was negative. The subscapularis and other cuff tendons were clinically intact.
Postoperative CT scan done at four and six months revealed that the coracoid graft had united with some resorption of the upper part of the coracoid graft, rendering the proximal screw-head a little prominent (Figure 5). The posterior ends of both screws were not protruding. The prominent proximal screw-head was thought to be the cause of the clicking due to attrition on the subscapularis tendon. He consented to undergo diagnostic arthroscopy of the shoulder and removal of the screws.
Diagnostic arthroscopy revealed that the coracoid graft has united, with near-normal glenoid remodelling at six months’ postoperative period (Figure 6). Removal of screws was uneventful, and upon direct palpation, the coracoid graft was confirmed to be solidly united to the glenoid. Postoperatively, he had started back on his gym routines without any discomfort. However, clicking was still present albeit being painless and not causing limitations of his gym and daily activities.
DISCUSSION
Even though the union of the coracoid graft to the native glenoid has been studied well, the degree of glenoid remodelling has only been looked upon by very few studies. Coracoid graft union and restoration of bony glenoid surface, which are essential for successful Latarjet procedures, should ideally be followed by continuous glenoid remodelling.
Moroder et al. found that grafting the glenoid with iliac crest bone grafts would subsequently result in this type of graft undergoing attenuation and remodelling, noted at 12 and 24 months postoperatively.4 Similar findings were noted by DiGiacomo et al., where they found maximum osteolysis and remodelling when there was a significant bone loss on the glenoid before Latarjet was performed.5 They postulated that this osteolysis and remodelling process of the glenoid were influenced by the mechanotransduction effect from the humeral head during movement of the shoulder. Similarly, in our second patient, CT scan revealed graft resorption on the upper part of the coracoid graft at four months postoperatively. Neyton et al. believe that remodelling may occur as early as six weeks post-operatively in determining their maximum cut-off point for CT imaging to be done for their study on graft positioning between open and arthroscopic techniques.6
Postoperative CT scan study done by Kee et al. showed complete remodelling of their coracoid grafts at eight months’ postoperatively, with osteolysis occurring over the outside of the coracoid graft and not on the inside which were fixed facing the native glenoid.7 Furthermore, maximum osteolysis was noted to involve the upper third of the grafts. They also noted that there was no significant difference in the magnitude of osteolysis between 7.7 and 31.7 months postoperatively. This may suggest that remodelling of the glenoid may be complete as early as eight months, postoperatively. Our second case showed significant osteolysis of the upper part of the coracoid at four months, rendering the proximal screw to be prominent, with subsequent clicking during rotational movement of the shoulder. This resorption was more significant when CT was repeated at six months postoperatively.
Xu et al. in a study evaluating their arthroscopic suture button method of coracoid fixation found out that 10 grafts (out of their 50 cases reviewed) that were put too laterally over the glenoid surface, remodelled significantly at six months’ postoperatively.8 Follow-up CT scan performed on these patients at two years postoperatively also did not reveal any glenohumeral degenerative changes, highlighting the protective nature of this remodelling process.
A study by Zhu et al. noted the rate of osteolysis in their patients as high as 90%. They also noted that the main osteolysis involves the upper part of the graft, attributing this finding to (a) the distance from the conjoint tendon as the source of blood supply to the graft and (b) the fact that more stress was borne by the inferior part of the graft during ABER position; therefore, according to Wolf's law, the superior part of the graft would undergo more significant resorption.9 Boileau et al. suggested suture button fixation as an alternative to screw fixation as there was no hardware-related complications and it avoided screw impingement with no hardware removal reported.10 We also suggest putting an absorbable screw for fixation of the coracoid graft, to avoid future hardware problems related to screw- prominence.
This case report highlights two main issues. Firstly, patients with hardware problems may present with symptoms mimicking recurrence of instability, and these symptoms will abate once screws are removed. Secondly, grafts will subsequently undergo osteolysis for the glenoid to remodel itself, with resultant screw head prominence which would cause clicking in the patient's shoulder. Removal of the screws would likely overcome this clicking issue. Knowledge on graft osteolysis and remodelling is currently limited. A more in-depth look at this aspect of graft healing after a Latarjet procedure is needed to draw more definitive conclusions in the future.
PATIENTS’ CONSENT:
Informed consents have been obtained from the patients to publish the data concerning their case.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
NMN: Conceived the idea and drafted the manuscript.
RYK: Helped with compilation of figures and proofreading of the manuscript.
AHR: Helped with scope picture retrieval and proofreading of the manuscript.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Ernstbrunner L, Gerber C. Editorial commentary: Computed tomography-based analysis of the arthroscopic Latarjet procedure suggests graft positioning is more variable than expected. Arthroscopy 2018; 34(7):2041-4. doi: 10.1016/j. arthro.2018.05.007.
- Hurley ET, Fat DL, Farrington SK, Mullet H. Open versus arthroscopic Latarjet procedure for anterior shoulder instability: A systematic review and meta-analysis. Am J Sports Med 2019; 47(5):1248-53. doi: 10.1177/03635465 18759540.
- Griesser MJ, Harris JD, McCoy BW, Hussain WM, Jones MH, Bishop JY, et al. Complications and reoperations after bristow-latarjet shoulder stabilisation: A systematic review. J Shoulder Elbow Surg 2013; 22(2):286-92. doi: 10.1016/j. jse.2012.09.009.
- Moroder P, Hirzinger C, Lederer S, Matis N, Hitzl W, Tauber M, et al. Restoration of anterior glenoid bone defects in post-traumatic recurrent anterior shoulder instability using the J-bone graft shows anatomic graft remodelling. Am J Sports Med 2012; 40(7):1544-50. doi: 10.1177/0363546 512446681.
- DiGiacomo G, Gasperis N, Costantini A, DeVita A, Rojas Beccaglia MA, Pouliart N. Does the presence of glenoid bone loss influence coracoid bone graft osteolysis after the Latarjet procedure? A computed tomography scan study in 2 groups of patients with and without glenoid bone loss. J Shoulder Elbow Surg 2014; 23(4):514-8. doi: 10.1016/j.jse. 2013.10.005.
- Neyton L, Barth J, Nourissat G, Metais P, Boileau P, Walch G, et al. Arthroscopic Latarjet techniques: Graft and fixation positioning assessed with 2-dimensional computed tomography is not equivalent with standard open technique. Arthroscopy 2018; 34(7):2032-40. doi: 10. 1016/j.arthro.2018.01.054.
- Kee YM, Kim JY, Kim HJ, Sinha S, Rhee YG. Fate of coracoid grafts after the Latarjet procedure: Will be analogous to the original glenoid by remodelling. Knee Surg Sports Traumatol Arthrosc 2018; 26(3):926-32. doi: 10.1007/ s00167-017-4808-z.
- Xu J, Liu H, Lu W, Zhu W, Peng L, Ouyang K, et al. Clinical outcomes and radiologic assessment of a modified suture button arthroscopic Latarjet procedure. BMC Musculoskelet 2019; 20(1):173. doi: 10.1186/s12891-019-2544-x.
- Zhu YM, Jiang CY, Lu Y, Li FL, Wu G. Coracoid bone graft resorption after Latarjet procedure is underestimated: A new classification system and a clinical review with computed tomography evaluation. J Shoulder Elbow Surg 2015; 24(11):1782-8. doi: 10.1016/j.jse.2015.05.039.
- Boileau P, Saliken D, Gendre P, Seeto BL, d'Ollonne T, Gonzalez JF, et al. Arthroscopic latarjet: Suture-button fixation is a safe and reliable alternative to screw fixation. Arthroscopy 2019; 35(4):1050-61. doi: 10.1016/j.arthro. 2018.11.012.