Solitary Plasmacytoma in a Patient Presenting with Taste Disturbance
By Ugur Ergun1, Ayse Uysal2, Hasmet Yazici3Affiliations
doi: 10.29271/jcpsp.2022.08.S165ABSTRACT
Solitary plasmacytoma is a disease included in plasma cell dyscrasias, presenting outside of the bone marrow, and with the potential to turn into multiple myeloma. A 66-year male patient was admitted to the hematology clinic with the complaint of impaired taste. Physical examination revealed edema of the left pharynx. After excisional tissue biopsy, serum/urine protein electrophoresis, and immunofixation tests of the patient diagnosed with plasmacytoma were negative. An increase in atypical plasma cells was noted on bone marrow aspiration and biopsy. There was no systemic involvement outside the pharynx on the PET-CT examination. He was referred to the radiotherapy department for further management. Since the affected area is frequently the nasopharynx, sinuses, and larynx in extramedullary solitary plasmacytoma cases, they generally presented to the clinic with difficulty in swallowing, shortness of breath and pain symptoms. This case presented with a non-specific complaint of taste disturbance along with difficulty in swallowing.
Key Words: Plasmacytoma, Nasopharynx, Multiple myeloma.
INTRODUCTION
Solitary plasmacytoma (SP) is a solitary neoplasm of monoclonal plasma cells. It has two forms: bony or extramedullary. Solitary extramedullary plasmacytoma is mostly localised in the nasopharynx, larynx, or sinuses.1-3 The incidence of solitary bony plasmacytoma is higher than the solitary extramedullary plasmacytoma. Also, the prognosis is different even if both forms respond well to the treatment, overall survival and progression-free survival of solitary bony plasmacytoma are poorer than solitary extramedullary plasmacytoma due to its higher rate of evolution to multiple myeloma (MM).4 Herein, we present a case of solitary extramedullary plasmacytoma which presented with taste disturbance and difficulty in swallowing.
CASE REPORT
A 66-year male presented with the complaints of difficulty in swallowing and taste disturbance for about six months. There was no feature in the patient's medical history except for receiving anti-tuberculosis treatment due to necrotizing granulomatous inflammation of the right eye lacrimal gland for six months.
Clinically, there was irregularity and edema of the left posterior wall of the pharynx. No pathological findings were observed in hemogram or biochemistry tests. The nasopharyngeal magnetic resonance (MR) revealed mucosal irregularities in the posterior wall of the oropharynx and hypopharynx, suggestive of pathologicalpolypoid structures (Figures 1, 2). Excisional biopsy was done. The histopathological study showed neoplastic plasma cells in the soft tissue. The immunohistochemical marker, CD 138, was positive in plasma cells. The other laboratory tests including serum/urine protein electrophoresis, and serum/urine immunofixation electrophoresis revealed normal results; however, serum IgG and kappa levels were slightly high (serum IgG: 16.9 g/L, serum IgA: 1.96 g/L, serum IgM: 0.402 g/L, serum kappa light chain: 4.05 mg/dl, and serum lambda light chain: 2.64 mg/dl). Plasma cells were normal in normocellular bone marrow. Positron emission tomography (PET) imaging performed by intravenous administration of F-18 fluoro-2-deoxy-glucose (FDG), was reported as increased uptake in the lingual tonsils, bilateral palatine tonsils, and oropharyngeal mucosa. The patient received radiotherapy at a dose of 50 Gy, and was followed up by the haemotology and radiation oncology clinic.
DISCUSSION
Solitary bony plasmacytoma and solitary extramedullary plasmacytoma represent a rare subgroup of plasma cell dyscrasias. As such, it has been difficult to accrue large cohorts and perform clinical trials that would change the treatment paradigm of SP. MM is generally located in the bone marrow and associated with a wide spectrum of clinical, laboratory, and radiological findings. Conversely, SP is characterised by a single mass of clonal plasma cells, with no or minimal bone marrow plasmacytosis and with no other symptoms except those derived from the primary lesion. It can present either as extramedullary plasmacytoma, i.e. in soft tissues or as solitary bony plasmacytoma.5 SP generally has a good prognosis, and tissue biopsy is the gold standard for diagnosis. However, systemic changes such as hypocalcemia, hypercalcemia, anemia, leukopenia, thrombocytopenia, and impaired kidney function have not been seen in the plasmacytoma.6 The incidence of SP has been reported to be 0.15 per 100,000 population and it is a rare disease.7 In an analysis of Anderson Cancer Centre data between 1963 and 1996, 1272 (94%) patients had MM, 60 (4%) patients had SP, and 22 (2%) patients had extramedullary plasmacytoma.8
 Figure 1: Axial T2 MRI scan shows hypointense, polypoid lesions (red arrows) throughout the posterolateral parts of the hypopharengeal mucosa.
Figure 1: Axial T2 MRI scan shows hypointense, polypoid lesions (red arrows) throughout the posterolateral parts of the hypopharengeal mucosa.
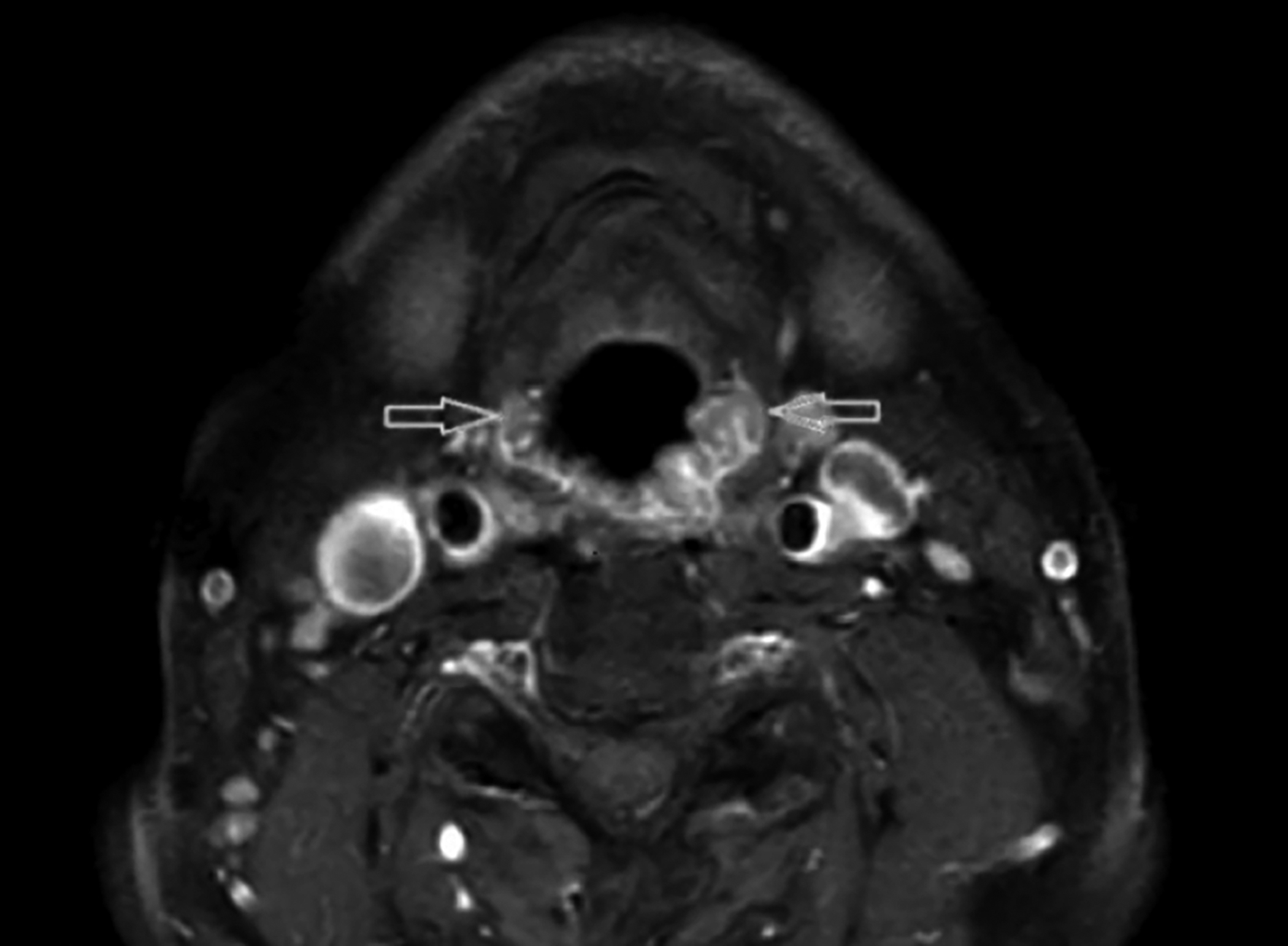 Figure 2: Axial T1 SPIR contrast enhanced scan shows that the lesions (red arrows) have peripheral enhancement.
Figure 2: Axial T1 SPIR contrast enhanced scan shows that the lesions (red arrows) have peripheral enhancement.
The clinical presentation of SP mostly depends on the location of the tumor. Since the affected area is frequently the nasopharynx, sinuses, and larynx in solitary extramedullary plasmacytoma cases, they generally present to the clinic with difficulty in swallowing, shortness of breath, epistaxis, nasal congestion, and pain symptoms. Herein, a case of SP presenting with a non-specific complaint of taste disturbance along with difficulty in swallowing is presented. To the existing knowledge, there was no such a case in the literature.
Due to the rarity of the disease, there is no consensus about prognostic factors and treatment. The treatment methods of SP have comprised of local surgery, radiotherapy, systemic chemotherapy, or combination of options. Radiotherapy is the treatment of choice; however, some authors debate about the radiotherapy dose and the relationship with the response rate. Moreover, the role of surgery and chemotherapy is still under debate. Nevertheless, we must consider that the majority of studies include a small number of patients and analyse the efficacy of conventional chemotherapy; few cases are reported concerning the efficacy of novel agents. This patient has received radiotherapy treatment only.
In conclusion, for the diagnosis of SP in the nasopharyngeal area, non-specific clinical findings, such as loss of taste, should also be kept in mind.
PATIENT’S CONSENT:
Written informed consent was obtained from the patient who participated in this case.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
AU: Concept and data collection.
UE: Design, supervision, resources, materials, analysis and interpretation, literature review and writing the manuscript.
HY: Critical review.
All authors approved the final version of the manuscript to bew published.
REFERENCES
- Kilciksiz S, Karakoyun-Celik O, Agaoglu FY, Haydaroglu A. A review for solitary plasmacytoma of bone and extramedullary plasmacytoma. Sci World J 2012; 2012: 895765. doi: 10.1100/2012/895765.
- Witzig TE, Laumann K, Lacy M, Hayman S, Dispenzieri A, Kumar S, et al. A phase III randomized trial of thalidomide plus zoledronic acid versus zoledronic acid alone in patients with asymptomatic multiple myeloma. Leukemia 2013; 27(1):220-5. doi: 10.1038/leu.2012.236.
- Jacob LA, Babu MS, Lakshmaiah K, Babu KG, Lokanatha D, Rajeev L, et al. Multiple myeloma: Experience of an institute in limited resource setting. Indian J Cancer 2017; 54(1):340. doi: 10.4103/ijc.IJC_87_17.
- Bora K. Distribution of multiple myeloma in India: Heterogeneity in incidence across age, sex and geography. Cancer Epidemiol 2019; 59:215-20. doi: 10.1016/j. canep.2019.02.010
- Nahi H, Genell A, Wålinder G, Uttervall K, Juliusson G, Karin F, et al. Incidence, characteristics, and outcome of solitary plasmacytoma and plasma cell leukemia. Population‐based data from the Swedish Myeloma Register. Eur J Haematol 2017; 99(3):216-22. doi: 10.1111/ejh.12907.
- Kilciksiz S, Celik OK, Pak Y, Demiral AN, Pehlivan M, Orhan O, et al. Clinical and prognostic features of plasmacytomas: A multicenter study of Turkish oncology group‐sarcoma working party. Am J Hematol 2008; 83(9):702-7. doi: 10. 1002/ajh.21211.
- Dimopoulos MA, Moulopoulos LA, Maniatis A, Alexanian R. Solitary plasmacytoma of bone and asymptomatic multiple myeloma. Blood J Am Soc Hematol 2000; 96(6): 2037-44.
- Liebross RH, Ha CS, Cox JD, Weber D, Delasalle K, Alexanian R. Clinical course of solitary extramedullary plasmacytoma. Radiother Oncol 1999; 52(3):245-9.