Solid Renal Mass in a Transplanted Allograft Kidney: Mucinous Tubular and Spindle Cell Renal Cell Carcinoma
By Erdinc Dincer1, Osman Murat Ipek1, Sukran Sarikaya Kayipmaz2, Oktay Akca1Affiliations
doi: 10.29271/jcpsp.2022.08.S192ABSTRACT
Renal transplantation is the main treatment for end-stage kidney disease. Transplantation reduces the mortality rate and increases life quality in this population but cancer in allograft kidney is a major problem. Here, we report a 39-year male who had renal transplantation 10 years ago. On routine follow-up, radiologic imaging revealed a 32 mm mass in the allograft kidney. After partial nephrectomy, histopathologic examination revealed mucinous tubular and spindle cell variant of renal cell carcinoma(MTSCC). To our best knowledge, this is the first case in the literature that underwent partial nephrectomy in the transplanted kidney and was diagnosed with MTSCC.
Key Words: Renal mass, Mucinous tubular and spindle cell tumor, Kidney transplantation.
INTRODUCTION
Renal transplantation is the gold standard in the treatment of end-stage kidney disease (ESRD). The long-term mortality rate in patients who have undergone renal transplantation is 48-82%. This rate is lower than patients on the transplant waiting list.1 However, one of the most important complications affecting mortality and morbidity after renal transplantation is malignancy. Patients may have renal cancer in both native and transplanted kidneys but it is rare in transplanted kidneys.
Mucinous tubular and spindle cell carcinoma (MTSCC) is a rare variant of renal cell carcinoma (RCC). Morphologically, it consists of tubules, spindle cells, and extracellular mucinous/ myxoid stroma.2
We present a case of MTSCC in a renal transplant patient who was treated by partial nephrectomy, which, to the best of our knowledge, is the first case in the literature.
CASE REPORT
A 39-year male patient had renal transplantation 10 years ago. on routine follow-up, urinary ultrasonography revealed a 32×26mm, isoechogenous, regular-border mass in the posterior part of the middle zone of transplanted kidney.
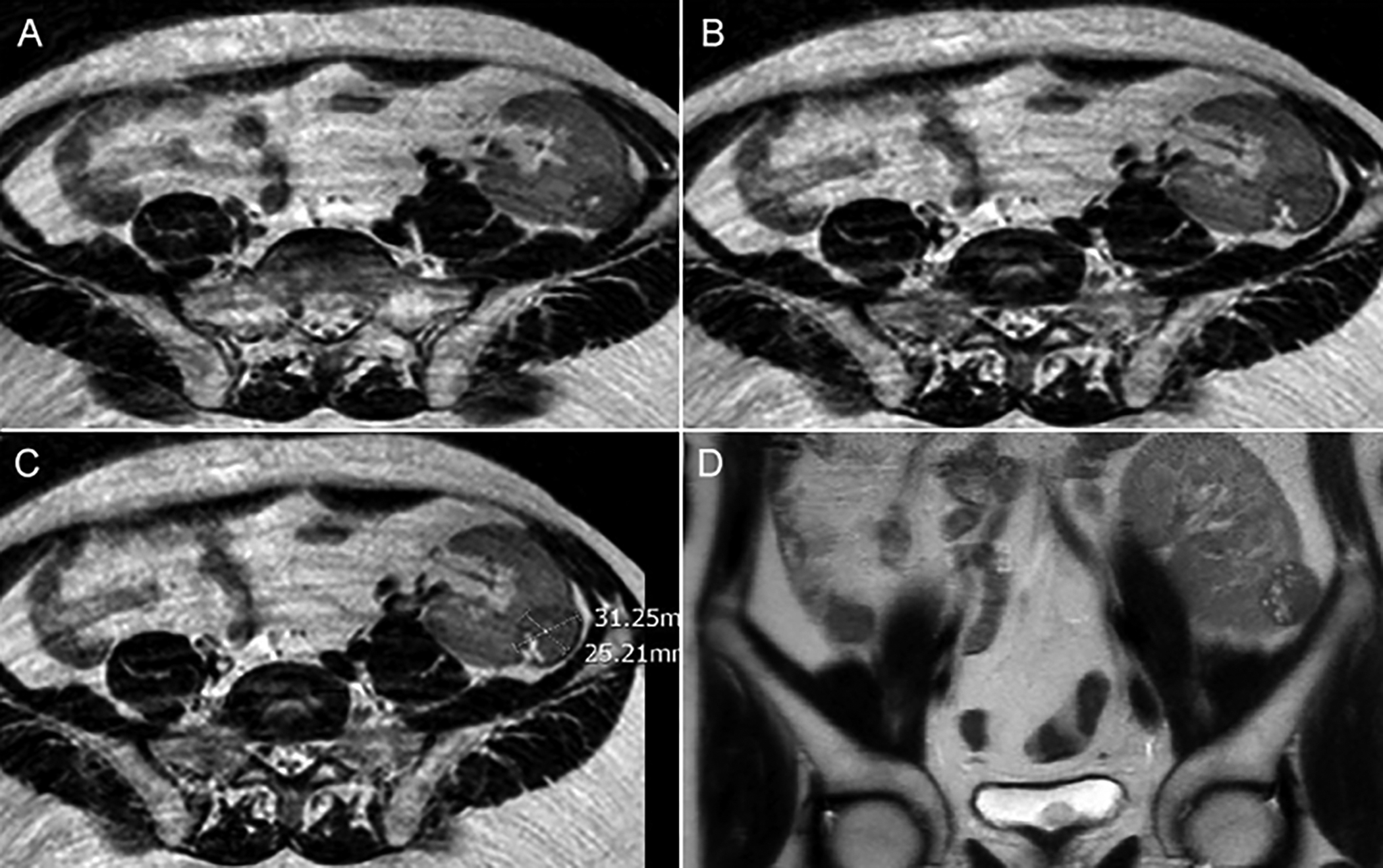 Figure 1: Magnetic resonance imaging of mass in the transplanted kidney.
Figure 1: Magnetic resonance imaging of mass in the transplanted kidney.
In abdominal magnetic resonance imaging with intravenous contrast, there was a 31×25mm, low-enhancing mass in the posterolateral aspect of the transplanted kidney. This mass had a heterogeneous structure and smooth contour. Partial nephrectomy was planned for the patient (Figure 1). At first step, an ureteral stent was placed in the transplanted kidney. Abdominal incision was made at the old incision area. Renal pedicle was dissected and the renal artery and vein were exposed. A partial nephrectomy was completed by removing the 30mm mass. The total operation time was 180 minutes including ischemia time (ischemia time: 15 minutes). Estimated blood loss was approximately 135 cc and blood transfusion was not required. The patient was discharged on the postoperative day 1 without complications. Postoperatively, at 3 weeks, serum creatinine was 1.9 mg/dL. Histopathological examination revealed a tumoral lesion of 33×23×20mm in size containing hemorrhagic cystic areas, which were separated from the surrounding tissue by a well-formed capsule. In the immunohistochemical examination, AMACR, CD57, CK7, PAX 2, and PAX 8 were positive and XT-1 was negative (Figure 2). MTSCC with tubular growth pattern and negative surgical margins was diagnosed. There was no recurrence or renal failure at the 3rd postoperative year.
 Figure 2: Histopathology of the solid mass in the transplanted kidney. A: Mucin content in the tumor (Alcien Blue stain,×200). B: Tumor tissue consisting of tubular structures separated from the kidney parenchyma by a well-formed capsule. (HE,×40). C: Tubular structures lined with low-grade cuboidal cells (HE, ×200).
Figure 2: Histopathology of the solid mass in the transplanted kidney. A: Mucin content in the tumor (Alcien Blue stain,×200). B: Tumor tissue consisting of tubular structures separated from the kidney parenchyma by a well-formed capsule. (HE,×40). C: Tubular structures lined with low-grade cuboidal cells (HE, ×200).
DISCUSSION
Although long-term use of immunosuppression plays a role in cancer development in transplanted patients, the reason is multifactorial. These factors include an increased risk of oncoviral-induced malignancy, reduced immune surveillance of neoplastic cells, and the presence of certain agents with pro-oncogenic properties.3 While the incidence of renal cell carcinoma(RCC) in allograft kidneys is low(0.19-0.5%), there is an approximately 10-fold increase in the development of solid malignancy compared to the general population(0.017%).1
Although higher papillary RCC incidence in native kidneys of ESRD patients is well known, it is not known why it is observed in allograft kidneys regardless of kidney function after transplantation.1 The RCC subtype MTSCC, has low malignant features and good prognosis. Most of the reported cases have undergone surgical treatment. It has a good prognosis compared to other RCC variants. In MTSCC, recurrence and metastasis are rarely seen after resection.4 Therefore, it is very important to make the correct diagnosis from papillary RCC on histopathological examination.
In the literature, MTSCC was incidentally detected (7 mm focus) in a nephrectomy specimen performed on the transplanted kidney due to multifocal RCC.5 The present case is the first in the literature that underwent partial nephrectomy in the transplanted kidney and was diagnosed with MTSCC.
Patients undergoing radical nephrectomy due to the renal tumor developing in the allograft kidney will become anephric, returning to hemodialysis. The associated complications will decrease life expectancy. Partial nephrectomy is routinely performed nowadays in localised kidney masses. Shortness of the renal pedicle, and narrow confines of the iliac fossa cause difficulty in performing partial nephrectomy for allograft kidneys. Therefore, partial nephrectomy has been performed in the limited number of patients.6 Postoperative follow-up routines can be the same as in other partial nephrectomy cases.
Ultrasonography is a cheap, non-invasive, easily accessible, and sensitive method for imaging.
Most of the renal masses are detected incidentally and the rate of RCC development is higher in transplanted kidney patients than in the general population. Therefore, these patients should be regularly examined. As per the European Association of Urology recommendation, follow-up with abdomen ultrasonography is recommended at intervals of 6-12 months after renal transplantation.7
With an increase in kidney transplantation rates, the frequency of renal cancer will increase in patients. The lesions will be detected in ultrasound when they are small by the close follow-up of patients. We think that partial nephrectomies on the allograft kidney will increase in experienced centres.
COMPETING INTEREST:
The authors declared no competing interest.
PATIENT’S CONSENT:
The consent of the patient was taken prior to writing of the manuscript.
AUTHORS’ CONTRIBUTION:
ED: Concept, design, writing, and literature review.
OMI: Concept, writing, and supervision.
SK: Data collection and material.
OA: Supervision, analysis, and interpretation.
All the authors approved the final version of the manuscript to be published.
REFERENCES
- Griffith JJ, Amin KA, Waingankar N, Lerner SM, Delaney V, Ames SA et al. Solid renal masses in transplanted allograft kidneys: A closerlook at the epidemiology and management. Am J Transplant 2017; 17(11):2775-81. doı: 10.1111/ajt.14366 .
- Zhao M, He XL, Teng XD. Mucinous tubular and spindle cell renal cell carcinoma: A review of clinicopathologic aspects. Diagn Patho 2015; 10:168. doi: 10.1186/s13000-015- 0402-1.
- Karami S, Yanik EL, Moore LE, Pfeiffer RM. Copeland G. Gonsalves L, et al. Risk of renal cell carcinoma among kidney transplant recipients in the United States. Am J Transplant 2016; 16(12):3479-89. doi.10.1111/ajt.13862.
- Du JH, Zhang L, Liang CZ. Huge mucinous tubular and spindle cell carcinoma of kidney: A rare case report and literature review. Medicine (Baltimore) 2018; 97(43): 12933. doi: 10.1097/MD.0000000000012933.
- Ellis RJ, Ng KL, Samaratunga H, Del Vecchio SJ, Wood ST, Gobe GC. Multifocal primary neoplasms in kidney allografts: Evaluation of two cases. J Kidney Cancer VHL. 2016; 3(2):14-22. doi: 10.15586/jkcvhl.2016.53.
- Kaouk JH, Spana G, Hillyer SP, White MA, Haber GB, Goldfarb D. Robotic-assisted laparoscopic partial nephrectomy. For a 7-cm mass in a renal allograft. Am J Transplant 2011; 11(10):2242-6. doi: 0.1111/j.1600-6143. 2011.03655.x.
- Rodríguez Faba O, Boissier R, Budde K, Figueiredo A, Taylor CF, Hevia V, et al. European association of urology guidelines on renal transplantation: Update 2018. Eur Urol Focus 2018; 4(2):208-15. doı: 10.1016/j.euf.2018. 07.014.