Short-term Outcomes of Elective Abdominal Aortic Aneurysm Repair
By Zia Ur Rehman1, Hafsa Shaikh2, Ziad Sophie1Affiliations
doi: 10.29271/jcpsp.2024.01.105ABSTRACT
Objective: To evaluate the presentations, aetiologies, and outcomes (survival and morbidity) of patients who underwent abdominal aortic aneurysm (AAA) repair at a tertiary care centre in a low middle-income country (LMIC).
Study Design: Case-series study.
Place and Duration of the Study: Section of Vascular Surgery, Department of Surgery, The Aga Khan University Hospital, Karachi, Pakistan, from January 2000 till April 2022.
Methodology: All patients who underwent elective open repair for AAA were identified using ICD coding 10. Patients’ demographics, presentations, treatment options, and outcomes were recorded on a specially designed proforma. Outcomes were measured in terms of 30-day survival and perioperative complications.
Results: Forty-two patients were included in the study. Thirty-nine (92.9%) of them were males. The mean age was 63.8 + 12.6 years. Thirty-four (81%) patients had an infrarenal aortic aneurysm. The average aneurysm diameter was 8.0 + 2.73 cm. The in-hospital survival rate was 95.2% whereas 2 (4.8%) patients had in-hospital mortality. Acute kidney injury (AKI) was the most common complication, seen in 5 (11.9%) patients. Adverse outcomes were seen more in diabetic patients whereas increased incidence of AKI was noted in operations with supra-renal clamping (p<0.05).
Conclusion: Most patients presented with symptoms and large aneurysm size. Open AAA repair was performed safely with 4.8% in-hospital mortality and acceptable morbidity in the LMIC setting.
Key Words: Abdominal aortic aneurysm repair, Low middle-income country.
INTRODUCTION
Abdominal aortic aneurysm (AAA) mostly involve infra-renal aortic segment and are asymptomatic. They can also be incidentally detected for investigations done for unrelated abdominal symptoms. The natural history of aneurysms and risk of rupture are well-understood. A cohort study of patients who refused early operation and who were inoperable had shown that the risk of rupture is significant for >5.5 cm aneurysm.1
Elective repair is advised in patients who have an aneurysm size greater than 5.5 cm.2 In LMICs, they remain undetected due to lack of screening programmes and as a result, most patients present with ruptured or symptomatic aneurysms. Most of these patients are not able to reach the hospital alive.
Rapid expansion >1 cm/year or the development of symptoms such as abdominal pain and tenderness and/or back pain is usually as indication for prompt surgical intervention irrespective of size because of higher rupture rate. Most of the studies about presentations and outcomes of elective AAA repair came from centres of the developed world with higher volumes with very limited evidence from the underdeveloped countries. The objective of this study was to record the presentations, aetiologies, and outcomes (survival and morbidity) of patients who underwent AAA repair at a tertiary care centre at an LMIC.
METHODOLOGY
This was a retrospective, observational study including all patients who underwent surgical repair for AAA from January 2000 till April 2022 at the Section of Vascular Surgery, The Aga Khan University Hospital, Karachi. Consecutive sampling technique was used to collect the data. All adult patients with age >18 years who had undergone elective AAA repair were included in this study. Patients who underwent repair for ruptured aortic aneurysm and those with thoracic aortic aneurysm were excluded from the study.
Patients were identified from ICD coding 10. Patient data were recorded on a specially designed proforma. The proforma consisted of three parts. The first part was regarding patient demographic and preoperative characteristics including age, gender, comorbid, presentation, location size of the aneurysm, and diagnostic modality. Comorbids included smoking, hypertension, diabetes, COPD, coronary artery disease (CAD), and congestive heart failure, documented as per the literature.3-5 The second part was regarding operative characteristics (operative time, surgical approach, type of graft, and need for transfusion). The last part was regarding postoperative complications and patient outcomes. These outcomes were measured in terms of 30-day survival and perioperative complications.
An exemption was obtained from the Ethical Review Com-mittee of The Aga Khan University Hospital (ERC number 2022-7294- 22466). Data were entered and analysed using SPSS version 26. Quantitative variables were reported as means (+) SD and were assessed by independent t-test/Mann-Whitney test. Frequency and percentages were reported for the categorical variables and their correlation was assessed by Chi-square or Fisher’s exact test. A p-value <0.05 was considered significant unless stated otherwise.
RESULTS
Forty-four patients underwent elective AAA repair. Two of them had endovascular repair and were excluded from the study; the remaining 42 cases were analysed. Majority of the patients were male (n = 39; 92.9%). The mean age was 63.8 + 12.6 years. Most of the patients were symptomatic (n = 32; 76.2%) with abdominal pain as the predominating complaint (24; 57.1%) followed by leg and backache (n = 6, 14.2%). Hypertension was the most common comorbid seen in more than half of the patients (n = 26; 61.9%) followed by smoking (n = 23; 56.1%). CT scan was used as the first diagnostic modality in over half of the patients (36; 85.8%) followed by ultrasound (n = 4; 6.3%). Infrarenal was the most common site seen in 34 (81%) patients. The mean aneurysm diameter was 8. 0 + 2.73 cm (Table I).
Anterior transperitoneal approach was used in all patients for repair. Aortic clamp was placed at an infra-renal position in 31 (75.6%) patients. In majority of cases, bifurcated graft was used (n = 36; 87.8%) compared to a tube graft (n = 5; 12.2%). Twenty-eight (70%) patients had aorto-iliac reconstructions (Table II). Twenty-eight (71.8%) patients required a mean packed cell transfusion of 2.2 + 3.2 units. The average operating time was 318+72 minutes (equalling 5.33 + 1.29 hours). The average duration of admission was 11.8 + 5.6 days.
Majority of the patients had no postoperative complications (n = 27; 64.3%). Renal complications such as acute kidney injury (AKI) was seen in 5 patients (11.9%), as shown in Figure 1. Patients who had supra-renal clamping developed more postoperative AKI (p = 0.03). Patients with aorto- aortic tube graft also developed more AKI postoperatively (p<0.0001). Two patients had in-hospital mortality (4.8%). The cause of death was cardiac arrest in both patients.
Bivariate analysis showed adverse outcomes in patients with diabetes (p<0.05). No significant correlation was found between the outcome and the shape or size of aneurysm (p >0.05).
Table I: Demographic data and preoperative characteristics.
|
|
|
n (%) |
|
Gender |
Male |
39 (92.9%) |
|
|
Female |
3 (7.1%) |
|
Site |
Infrarenal |
34 (81%) |
|
|
Juxta renal |
7 (16.7%) |
|
|
Supra-celiac |
1 (2.4%) |
|
Shape |
Fusiform |
35 (83.3%) |
|
|
Saccular |
7 (16.7%) |
|
Aetiology |
Degenerative |
36 (85.7%) |
|
|
Inflammatory |
4 (9.5%) |
|
|
Suspected mycotic |
2 (4.4%) |
|
Presentation |
Symptomatic |
32 (76.2%) |
|
|
Asymptomatic |
10 (23.8%) |
|
Symptoms |
Abdominal pain |
24 (57.1%) |
|
|
Leg/back ache |
6 (14.2%) |
|
|
Pulsatile swelling |
2 (4.7%) |
|
Comorbids |
Hypertension |
26 (61.9%) |
|
|
Smoking |
23 (56.1%) |
|
|
CAD* |
15 (35.7%) |
|
|
Diabetes |
8 (19%) |
|
|
COPD** |
8 (19%) |
|
|
Creatinine >1.5 |
7 (17.5%) |
|
|
CHF*** |
0 |
| *CAD: Coronary artery disease; **COPD: Chronic obstructive pulmonary disease; ***CHF: Chronic heart failure. |
||
Table II: Intraoperative characteristics.
|
|
|
n (%) |
|
Graft type |
Bifurcated |
36 (87.8%) |
|
|
Tube |
5 (12.2%) |
|
Type of reconstruction |
Aorto-iliac |
28 (70%) |
|
|
Aorto-femoral |
7 (17.5%) |
|
|
Aorto-aortic |
5 (12.5%) |
|
Proximal clamp site |
Infrarenal |
31 (75.6%) |
|
|
Suprarenal |
9 (22%) |
|
|
Juxtarenal |
1 (2.4%) |
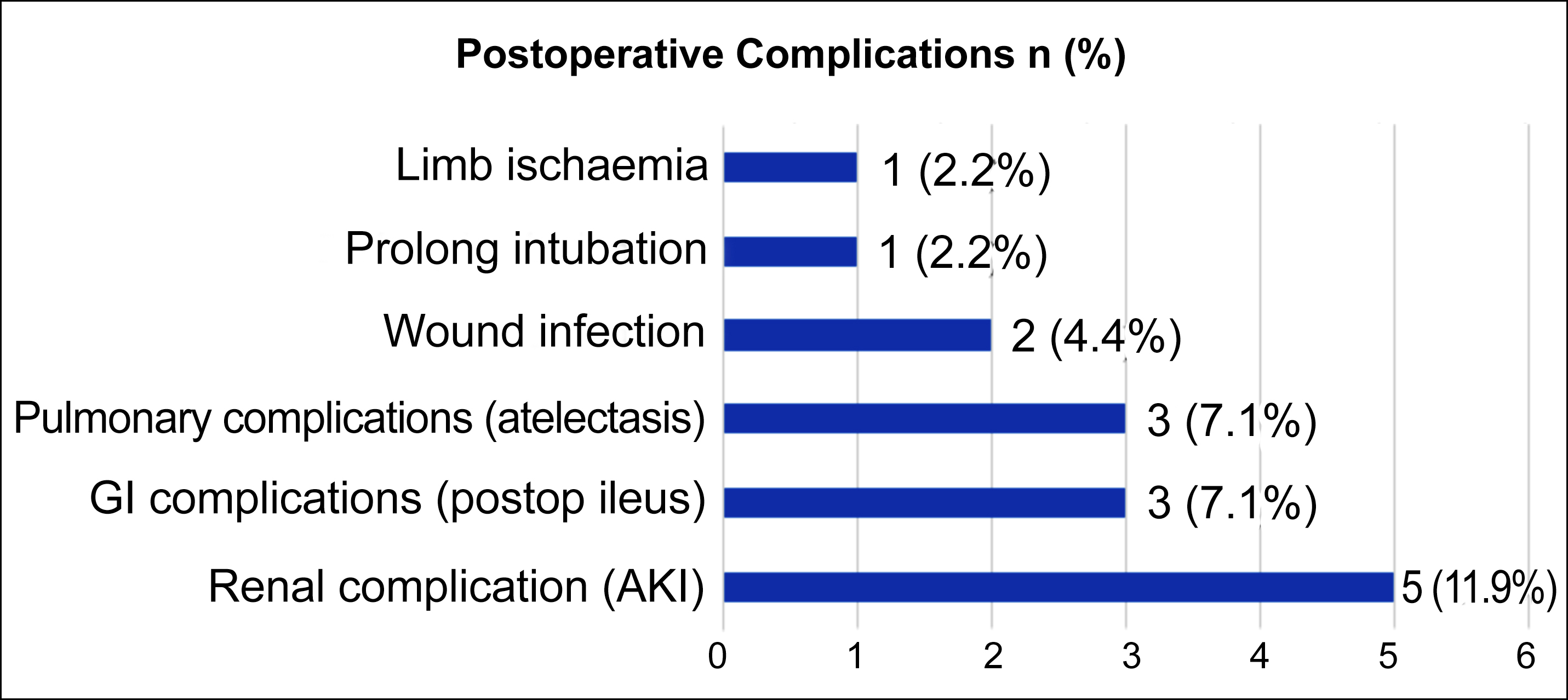 Figure 1 : Postoperative complications.
Figure 1 : Postoperative complications.
DISCUSSION
There are limited studies on the outcomes of AAA repair from LMICs. In the present study, most patients presented with various symptoms which led to the incidental diagnosis of AAA. The mean of aneurysm diameter was found to be 8.0 + 2.7 cm which is higher in comparison to the recent studies.6,7 Most of the patients were male as observed in other studies.
Acute kidney injury (AKI) was the most common complication seen in this study with an incidence of 11.9% followed by gastrointestinal and pulmonary complications (7.1% each). Common complications observed in other studies included cardiopulmonary failure, respiratory infections, myocardial ischaemia, and prolong intubation.8-10 Acute tubular necrosis was the most common cause of AKI post-AAA repair. Multiple factors were responsible for this complication such as aortic clamping and sepsis. Aortic clamping led to increased vascular resistance and reduced renal perfusion leading to AKI. The incidence and severity of complications of aortic clamping can worsen if the clamp is placed more proximally or for longer duration. AKI was more common in patients who had supra-renal aortic clamp placed as a part of their surgery.11 According to a study, the major predictors of AKI in patients undergoing supra-renal clamping for AAA repair were renal ischaemia time, blood loss >1L and operation time of more than 300 minutes.12 Similar results were observed in this study with a significant correlation between renal complications and suprarenal clamping (p = 0.03). Furthermore, suprarenal clamping was also associated with a higher mortality which was reported to be 14% according to a study.13 In this study, mortality rate following an open AAA surgery was 4.8%. This was comparable to the results observed in AAA repair studies over the years (2.5-4.7%).7-11 A similar study done from LMIC (Sri Lanka) showed aneurysm diameter >7 cm, aortic cross-clamp time >60 min, smoking and need for postoperative ventilation to be the predictors of significant morbidity and mortality.14 However, similar correlations were not identified in this study.
Diabetes was found to be associated with poor outcomes in this study. There was inconsistent evidence of correlation of postoperative mortality in diabetic and non-diabetic patients.15
This study had several limitations due to retrospective data from a single centre with a limited number of patients, whose results could not be generalised. A prospective, multicentric study will provide better evidence.
CONCLUSION
Elective open repair of AAA performed in a tertiary care centre of LMICs was a relatively safe operation with results comparable to the international studies.
ETHICAL APPROVAL:
An exemption was obtained from the Ethical Review Committee of The Aga Khan University Hospital (ERC number: 2022-7294- 22466).
PATIENTS’ CONSENT:
As this study was based on patient chart review, patients consent was not required.
COMPETING INTEREST:
There was nothing to disclose that could constitute a conflict of interest.
AUTHORS’ CONTRIBUTION:
ZR: Study conception.
HS: Data collection.
ZR, HS: Analysed the data, revised, reviewed the manuscript.
All authors approved the final version of the manuscript for publication.
REFERENCES
- Lederle FA, Johnson GR, Wilson SE, Ballard DJ, Jordan WD, Jr. Blebea J, et al. Rupture rate of large abdominal aortic aneurysms in patients refusing or unfit for elective repair. JAMA 2002;287(22):2968-72. doi: 10.1001/jama. 287.22.2968.
- Ullery BW, Hallett RL, Fleischmann D. Epidemiology and contemporary management of abdominal aortic aneurysms. Abdom Radiol (NY) 2018; 43(5):1032-43. doi: 10.1007/s00261-017-1450-7.
- American Diabetes Association. Classification and diagnosis of diabetes: Standards of medical care in Diabetes—2021. Diabetes Care 2021; 44(Suppl 1): S15- 33. doi: 10.2337/dc21-S002.
- Writing Committee Members; ACC/AHA Joint Committee Members. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure. J Card Fail 2022; 28(5): e1-e167. doi: 10.1016/j.cardfail.2022.02.010.
- Celli B, Fabbri L, Criner G, Martinez FJ, Mannino D, Vogelmeier C, et al. Definition and nomenclature of chronic obstructive pulmonary disease: Time for its revision. Am J Respir Crit Care Med 2022; 206:1317-25. doi: 10.1164/rccm.202204-0671PP.
- Janczak D, Bakowski W, Bakowska K, Marschollek K, Marschollek P, Malinowski M, et al. Early complications in patients undergoing elective open surgery for infrarenal aortic aneurysms. J Coll Physicians Surg Pak 2019; 29(11):1078-82. doi: 10.29271/jcpsp.2019.11.1078.
- Locham S, Shaaban A, Wang L, Bandyk D, Schermerhorn M, Malas MB. Impact of gender on outcomes following abdominal aortic aneurysm repair. Vasc Endovascular Surg 2019;53:636-43. doi: 10.1177/1538574419868040.
- Ferrante AM, Moscato U, Colacchio EC, Snider F. Results after elective open repair of pararenal abdominal aortic aneurysms. J Vasc Surg 2016; 63(6):1443-50. doi: 10. 1016/j.jvs.2015.12.034.
- Locham S, Rizwan M, Dakour-Aridi H, Faateh M, Nejim B, Malas M. Outcomes after elective abdominal aortic aneurysm repair in obese versus nonobese patients. J Vasc Surg 2018; 68(6):1696-705. doi: 10.1016/j.jvs. 2018.03.414.
- Bluro IM, Garagoli F, Fiorini NB, Rabellino JM, Chas JG, Domenech A, et al. Five-year outcomes of elective infrarenal abdominal aortic aneurysm repair at a university hospital in Argentina. Arch Cardiol Mex 2022; 92(2):222-9. doi: 10.24875/ACM.21000077.
- Zabrocki L, Marquardt F, Albrecht K, Herget-Rosenthal S. Acute kidney injury after abdominal aortic aneurysm repair: Current epidemiology and potential prevention. Int Urol Nephrol 2018; 50(2):331-7. doi: 10.1007/s11 255-017-1767-8.
- Yokoyama N, Nonaka T, Kimura N, Sasabuchi Y, Hori D, Matsunaga W, et al. Acute kidney injury following elective open aortic repair with suprarenal clamping. Ann Vasc Dis 2020;13(1):45-51. doi: 10.3400/avd.oa. 19-00095.
- Karthikesalingam A, Holt PJ, Patterson BO, Vidal-Diez A, Sollazzo G, Poloniecki JD, et al. Elective open suprarenal aneurysm repair in England from 2000 to 2010: An observational study of hospital episode statistics. PLoS One 2013; 8(5):e64163. doi: 10.1371/journal.pone. 0064163.
- Gunawansa N, Goonerathne T, Cassim R, Wijeyaratne M. Open repair of infra renal abdominal aortic aneurysms: A single center experience from the developing world. Ann Vasc Dis 2011; 4(4):313-8. doi: 10.3400/avd.oa.11. 00049.
- Pafili K, Gouni-Berthold I, Papanas N, Mikhailidis DP. Abdominal aortic aneurysms and diabetes mellitus. J Diabetes Complications 2015; 29(8):1330-6. doi: 10. 1016/j.jdiacomp.2015.08.011.