Pseudoactinomycotic Radiate Granules (PAMRAGs) in the Extensor Tendon of Hand
By Rifat SahinAffiliations
doi: 10.29271/jcpsp.2021.12.1503ABSTRACT
Pseudoactinomycotic radiate granules (PAMRAGs) are most frequently observed in female genitalia. Morphologically, these closely resemble the actual actinomycotic granules. Actinomyces are infectious organisms that require treatment; whereas, PAMRAGs do not require a specific treatment since they are not infectious. Here, we describe a previously unreported case of these granules in the hand. A 56-year woman was admitted with soft mass on the dorsal aspect of her right hand. Peroperatively, lesion was detected in the extensor digitorum communis. Histopathological examination revealed an appearance that resembled actinomyces. Periodic acid-Schiff (PAS) staining was not positive for actinomyces. Hematoxylin-eosin (HE) staining showed radially arranged refractile granules with thick, irregular club-like eosinophilic character without a central core. Thus, actinomycosis was ruled out and a diagnosis of PAMRAGs was made.
Differentiating PAMRAGs from actual actinomycotic infections is crucial for the treatment. Pathologists should be familiar with the presence and appearance of PAMRAGs to avoid misdiagnosis of actinomycosis and prevent unnecessary antibiotic use.
Key Words: Pseudoactinomycotic radiate granules (PAMRAGs), Extensor tendon, Actinomyces, Hand.
INTRODUCTION
Actinomyces, which is a gram-positive, non-spore-forming, anaerobic, rod-like bacterium, is generally observed in the genital area, genitourinary tract and oral cavity.1 It was reported that the presence of actinomyces was closely associated with the use of intrauterine device (IUD).2,3 However, further studies have shown that actinomyces and PAMRAGs could also be observed in patients who did not use IUD.4,5 PAMRAGs was first described in 1981.3 O’Brien et al. found pseudo-sulphur granules and pseudo-colonies in the endometrial curettage materials of patients who had a history of IUD use.1 They named these structures, which differed from actual sulphur granules; and which showed different staining characteristics than actinomyces despite the resemblance, as PAMRAGs.3 In 1908, Splendore described the eosinophilic material that surrounds bacteria; and stated that he accidentally discovered a new sporotrichum species.6 In 1932, Hoeppli described a similar eosinophilic appearance that surrounded schistosoma.7
Thereafter, the Splendore–Hoeppli (SH) phenomenon represented the eosinophilic material (radiate, star-like, asteroid or club-shaped configurations) that surrounds microorganisms or inorganic structures. Some researchers believed that PAMRAGs resembled the SH phenomenon.4,8 In our patient, the appearance was similar to that described by Splendore. There were radiate eosinophilic formations around, what resembled actinomyces.
CASE REPORT
A 56-year female presented to our clinic with localised swelling on the dorsal side of her right hand. Physical examination revealed a soft mass with well-defined borders that measured 2×2 ×2 cm and was sensitive to palpation and localised at the proximal aspect of the third metacarpal bone on the dorsal side of the right hand. There were no signs of infection such as redness, increased temperature or discharge. Her medical history revealed that the swelling had started two years ago and that needle aspiration was performed at another centre one year back. The swelling started to reoccur 10 days after the puncture and the patient also started to have pain. The patient had a history of diabetes and hypertension. Moreover, it was also understood that the patient used an IUD for 15 years and underwent total abdominal hysterectomy and bilateral salpingo-oophorectomy surgery five years ago. Ultrasound imaging showed a lesion of dense cystic nature with a size of 12×11 mm2 on the dorsal side of the right wrist, which was interpreted as a ganglion cyst. Magnetic resonance imaging (MRI) revealed a cystic lesion with disrupted wall continuity with a size of 10×10 mm2 inside the fourth compartment tendon sheath on the extensor surface, at the level of the carpal bones. The loculated fluid collection with 3 cm width that distally extended to the metacarpal base was interpreted as an intra-tendinous ganglion cyst. According to the laboratory tests, white blood cells, erythrocyte sedimentation rate, C-reactive protein, and hemoglobin values were within normal range.
A preliminary diagnosis of ganglion cyst was made, and a surgical excision was scheduled. After marking the skin with a dye; and covering the surgical site with a surgical drape, a longitudinal incision was made to reach the mass on the dorsal side of the right hand under local anaesthesia. The mass of soft consistency, mobile and uniformly cystic structure on the tendon sheath was excised via blunt dissection. The mass was sent for histopathological examination, which confirmed that the mass was a ganglion cyst. However, a relatively stiff, fixed and puffy localised swelling of 1.5 cm size in the extensor digitorum communis (EDC) was detected below the mass (Figure 1). The tendon was accessed by a vertical incision from the dorsal side. Yellowish spots, that accumulated to form lesions that did not appear infected, were observed within the tendon (Figure 2).
 Figure 1: The localised swelling in the extensor digitorum communis.
Figure 1: The localised swelling in the extensor digitorum communis.
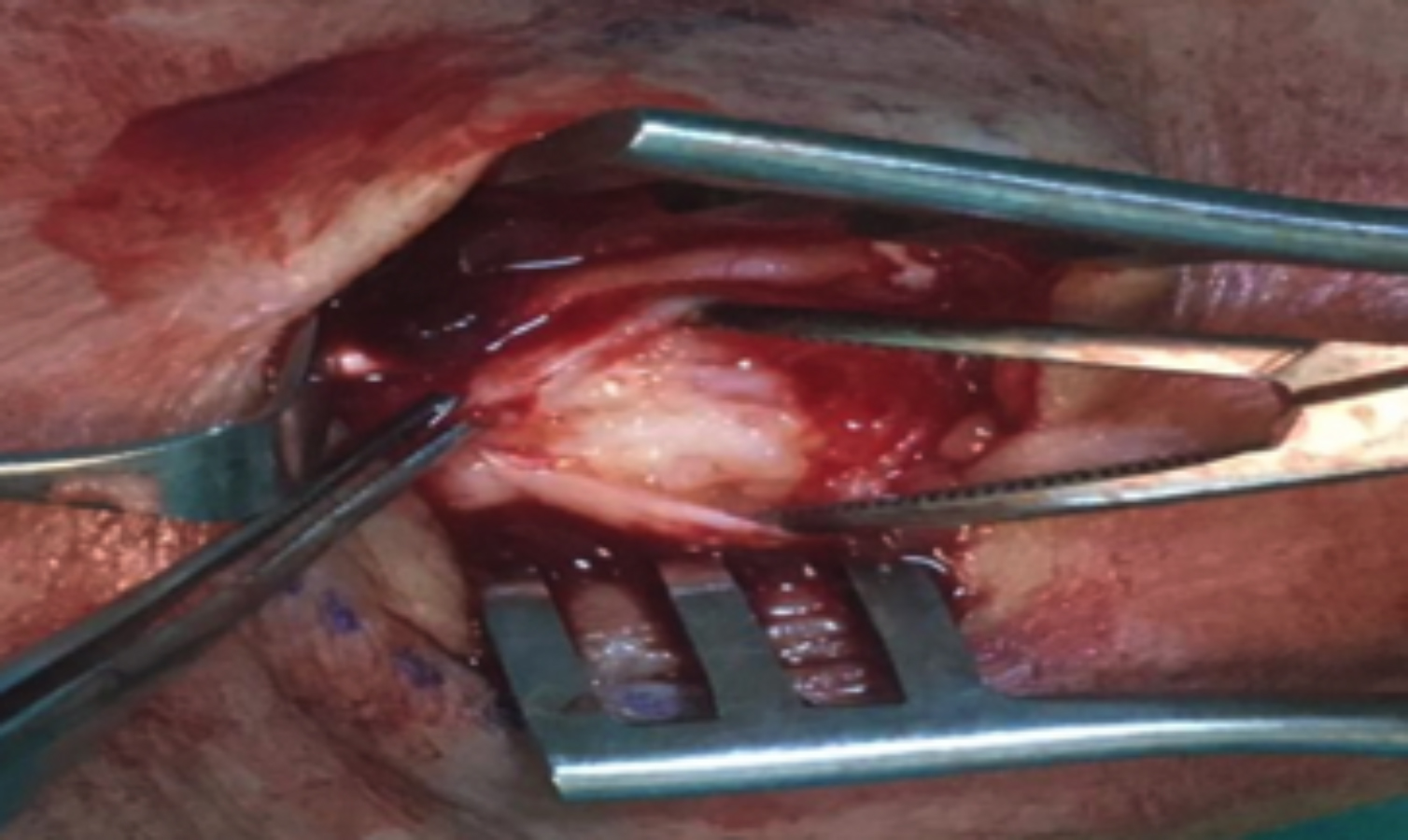 Figure 2: Yellowish spots within the tendon.
Figure 2: Yellowish spots within the tendon.
These lesions were excised and sent for histopathological examination. The tendon was repaired, washed and the layers were sutured. Histopathological examination revealed an appearance that resembled actinomyces. PAS staining was not positive for actinomyces (Figure 3A). Hematoxylin-eosin (HE) staining showed radially arranged refractile granules with thick, irregular club-like eosinophilic character without a central core (Figure 3B, C, D). According to these staining characteristics and appearance, it was determined that the patient had PAMRAGs.
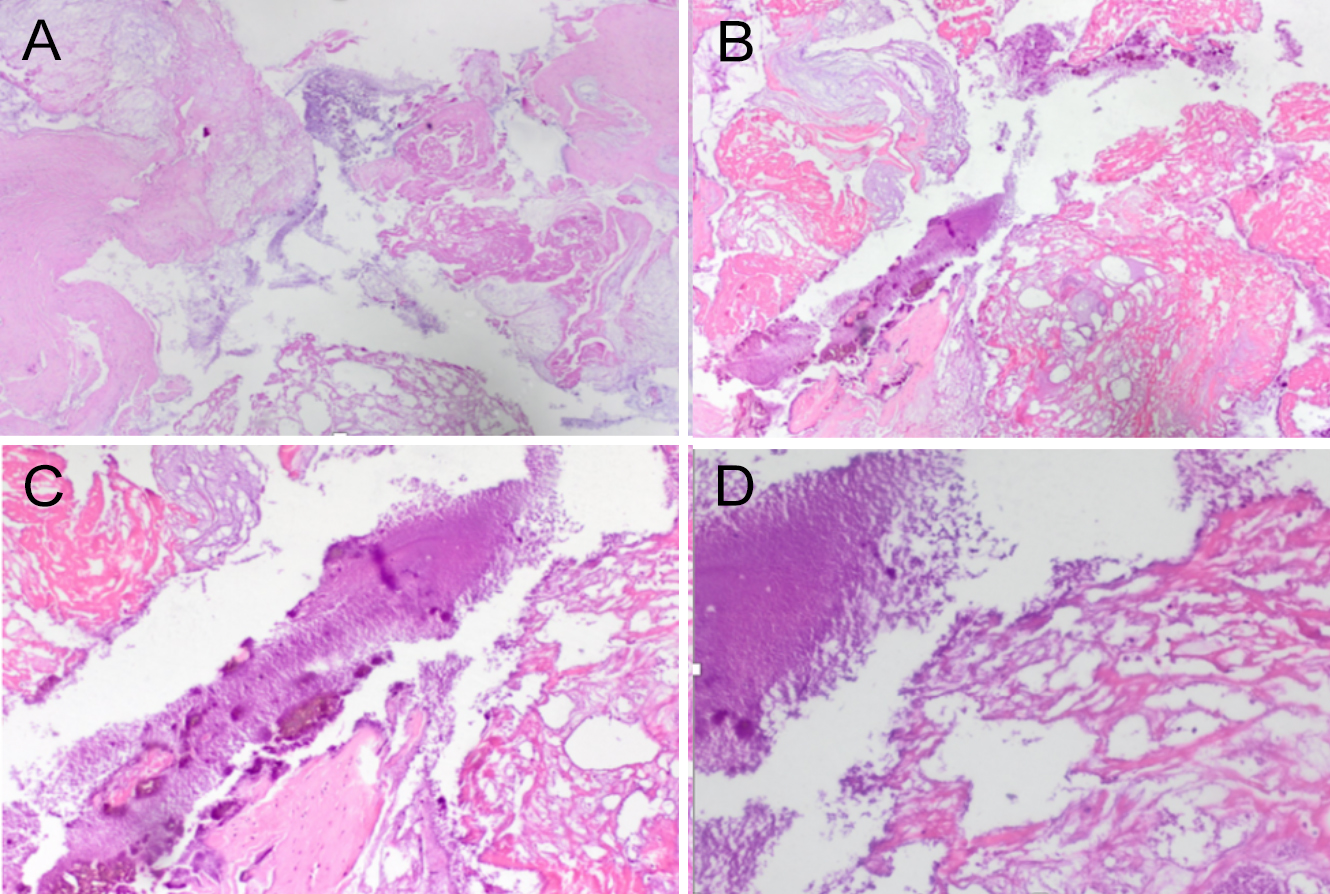 Figure 3: (A) PAS staining was not positive for actinomyces. (B, C, D) H&E x 40,100,200 staining showed radially arranged refractile granules with thick, irregular club-like eosinophilic character without a central core.
Figure 3: (A) PAS staining was not positive for actinomyces. (B, C, D) H&E x 40,100,200 staining showed radially arranged refractile granules with thick, irregular club-like eosinophilic character without a central core.
DISCUSSION
PAMRAGs are most frequently observed in female genitalia, particularly in the endometrium.3,7 They are also observed in paranasal sinuses, although rarely.9 From the pathomorphological aspect, PAMRAGs closely resemble actual actinomyces granules.9,10 Actinomyces are infectious organisms that require treatment; whereas, PAMRAGs do not require a specific treatment, since they are not infectious. However, these two can be present separately or coexist in one patient.5,8 It is difficult to differentiate PAMRAGs from actinomyces in routine histopathology.10 PAMRAGs appear as refractile granules with thick, irregular, club-like peripheral projections without a central core in HE staining. Actual actinomyces contain non-refractile thin basophilic filaments around a dense central eosinophilic core. Filaments of actinomyces are gram-positive in Brown and Brenn (B&B) staining, and they are also stained with Gomori methenamine-Silver (GMS). PAMRAGs exhibit negative or non-specific staining characteristics in B&B, GMS and acid-fast bacilli (AFB) staining.10
Isolation of PAMRAGs from the extensor tendon of the patient, who used IUD for 15 years, could stem from haematogenous dissemination. Moreover, the contamination of the extensor tendon, which is located right below the cyst with PAMRAGs, while aspirating the cyst in the patient’s hand with puncture one year ago, could also have caused this condition. This may explain why the patient’s clinical picture worsened after the puncture, while it was expected to improve.
Most of the reports regarding PAMRAGs involve gynaecologic tissues. The present case is important as it shows that PAMRAGs could also be observed in the extensor tendons. Differentiating PAMRAGs from actual actinomycotic infections is crucial for the treatment. Pathologists should be familiar with the presence and appearance of PAMRAGs to avoid the misdiagnosis of actinomycosis and prevent unnecessary antibiotic use.
PATIENT’S CONSENT:
Informed consent was obtained from the patient.
CONFLICT OF INTEREST:
The author declared no conflict of interest.
AUTHOR’S CONTRIBUTION:
RS: Contributed in all aspects of this manuscript and responsible for all.
REFERENCES
- Koneman EW, Allen SD, Janda WM. The anaerobic bacteria. In: Color atlas and textbook of diagnostic microbiology. Philadelphia, PA: Lippincott- Raven Publishers, 1997:709-84.
- Horn LC, Bilek K. Reaktive und areaktive Aktinomykose-Infektion des weiblichen Genitale und Abgrenzung zur Pseudoaktinomykose [Reactive and areactive actinomycosis infection of the female genitals and differentiation of pseudoactinomycosis]. Zentralbl Gynakol 1995; 117(9):466-71. German. PMID: 7483880.
- O'Brien PK, Roth-Moyo LA, Davis BA. Pseudo-sulfur granules associated with intrauterine contraceptive devices. Am J Clin Pathol 1981; 75(6):822-5. doi: 10.1093/ajcp/75.6.822.
- Bhagavan BS, Ruffier J, Shinn B. Pseudoactinomycotic radiate granules in the lower female genital tract: Relationship to the Splendore-Hoeppli phenomenon. Hum Pathol 1982; 13(10): 898-904. doi: 10.1016/s0046-8177(82)80049-x.
- Boyle DP, McCluggage WG. Combined actinomycotic and pseudoactinomycotic radiate granules in the female genital tract: Description of a series of cases. J Clin Pathol 2009; 62(12):1123-6. doi: 10.1136/jcp.2009.070193.
- Splendore A. Sobre a cultura d’una nova especie de cogumello pathogenico (Sporotrichose de Splendore). Revista de Sociedade de Sao Paulo 1908; 3:62.
- Hoeppli R. Histological observations in experimental schisto-somiasis japonica. Chin Med J (Engl) 1932; 46:1179.
- Padberg BC, Kolb SA, August C, Schröder S. Pseudoaktino-mykotische granula (Splendore-Hoeppli-Phänomen) im korpusabradat bei IUP [IUD-associated pseudoactinomycotic gradiate granules (Spendore-Hoeppli phenomenon) in uterine curettage]. Pathologe 2002; 23(2):135-9. German. doi: 10.1007/ s00292-001-0497-x.
- Starek I, Horacek J, Salzman R. Pseudoactinomycotic radiate granules in the maxillary sinus. A case report. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2020; 164(3):320-3. doi: 10.5507/bp.2019.012.
- Cicy PJ, Tessy PJ, Lekshmidevi P, Letha V, Poothiode U. Pseudoactinomycotic radiate granules (PAMRAGs)- an unusual differential diagnosis for ovarian neoplasm; a diagnostic dilemma. J Clin Diagn Res 2015; 9(3):ED01-2. doi: 10.7860/JCDR/2015/ 11643.5687.