Recurrent Bleeding From a Duodenal Ulcer Halted by Laparoscopic Oversewing Under Endoscopic Guidance
By Feng Chi, Shenkang ZhouAffiliations
doi: 10.29271/jcpsp.2022.08.S121ABSTRACT
Peptic ulcers are the most common causes of upper gastrointestinal bleeding. Although most peptic ulcer bleeding can be controlled by medical and endoscopic treatment, a small number of patients with recurrent bleeding eventually require surgical treatment. In recent years, laparoscopy, a minimally invasive surgical method, has gained popularity and acceptance. We, herein, report a case of recurrent duodenal ulcer bleeding. Laparoscopic oversewing of the bleeding ulcer under endoscopic guidance resulted in satisfactory recovery. We suggest that for recurrent bleeding from peptic ulcers, laparoscopic oversewing under endoscopic guidance should be recommended as a possible early option to halt the bleeding.
Key Words: Upper gastrointestinal bleeding, Peptic ulcer, Laparoscopy, Treatment.
INTRODUCTION
Upper gastrointestinal (GI) bleeding is one of the most common critical illnesses.1 Peptic ulcer (PU) bleeding is the main cause of upper GI bleeding.2 With the popularisation and progress of Helicobacter pylori eradication therapy and anti-ulcer therapy, its incidence has gradually declined in the past 20 years, but overall mortality has remained unchanged.3 Most PU bleeding can be controlled by medical and endoscopic treatment. However, re-bleeding would occur in a small number of patients. In these cases, although surgery is the most reliable method for hemostasis, repeated endoscopic treatment is preferred over surgery because of its less invasiveness. In recent years, laparoscopy, a minimally invasive surgical method, has gained great popularity and acceptance. We report a case of recurrent duodenal ulcer bleeding treated by laparoscopic oversewing under endoscopic guidance, and suggest the early utility of this procedure for recurrent bleeding in certain patients with PUs.
CASE REPORT
A 76-year woman presented with complaints of the passage of black stools for two days. The patient had a history of hypertension, type 2 diabetes, and uremia. On physical examination, she was pale (hemoglobin was 7.5 g/dL), but was afebrile.
On examination of vitals, her radial pulse was 89 beats/minute, and blood pressure was 163/93 mmHg. The abdominal examination was normal. She underwent upper GI endoscopy, which revealed a clean-based PU at the anterior wall of the duodenal bulb. Infusion of proton pump inhibitor was used. Two days later, she had melena again. A repeated upper GI endoscopy was done, which revealed oozing of blood from the former duodenal PU (Figure 1). An endoscopic heater probe was used to stop the bleeding. After another 2 days, she had one more episode of melena. She underwent upper GI endoscopy again, which also showed oozing of blood from the duodenal PU. Epinephrine injection and heater probe were used to halt the bleeding under endoscopy. When she had another episode of melena 1 day later, it was decided to attempt laparoscopic oversewing of the bleeding ulcer to minimize invasiveness. An initial 10 mm trocar was inserted below the umbilicus for laparoscopy and two additional trocars were placed in the right epigastric region. As identified by endoscopic observation, the ulcer from the serosal aspect under laparoscopy was oversewed with 2-0 Vicryl suture (Ethicon, Somerville, NJ) (Figure 2). The endoscopic view after this procedure is shown in Figure 3. The entire procedure took 60 min with minimal blood loss. Postoperatively, the patient did not experience bleeding again, and the recovery was uneventful.
DISCUSSION
Upper GI bleeding refers to bleeding caused by diseases of the digestive tract above the ligament of Treitz. Common causes include PUs, varices, malignant lesions, erosive gastritis, and Mallory-Weiss tears.4 Among them, PUs are the most common, and they are more often located in the duodenum. The most common symptoms are hematemesis and melena. If the amount of bleeding is large, it may be accompanied by signs of peripheral circulatory failure such as dizziness, palpitations, paleness, increased heart rate, and decreased blood pressure. Endoscopy is the key to the diagnosis of the cause, and it is recommended to be done within 24 hours after bleeding.5
 Figure 1: Endoscopy showing a bleeding duodenal ulcer (oozing).
Figure 1: Endoscopy showing a bleeding duodenal ulcer (oozing).
 Figure 2: Laparoscopic view after oversewing.
Figure 2: Laparoscopic view after oversewing.
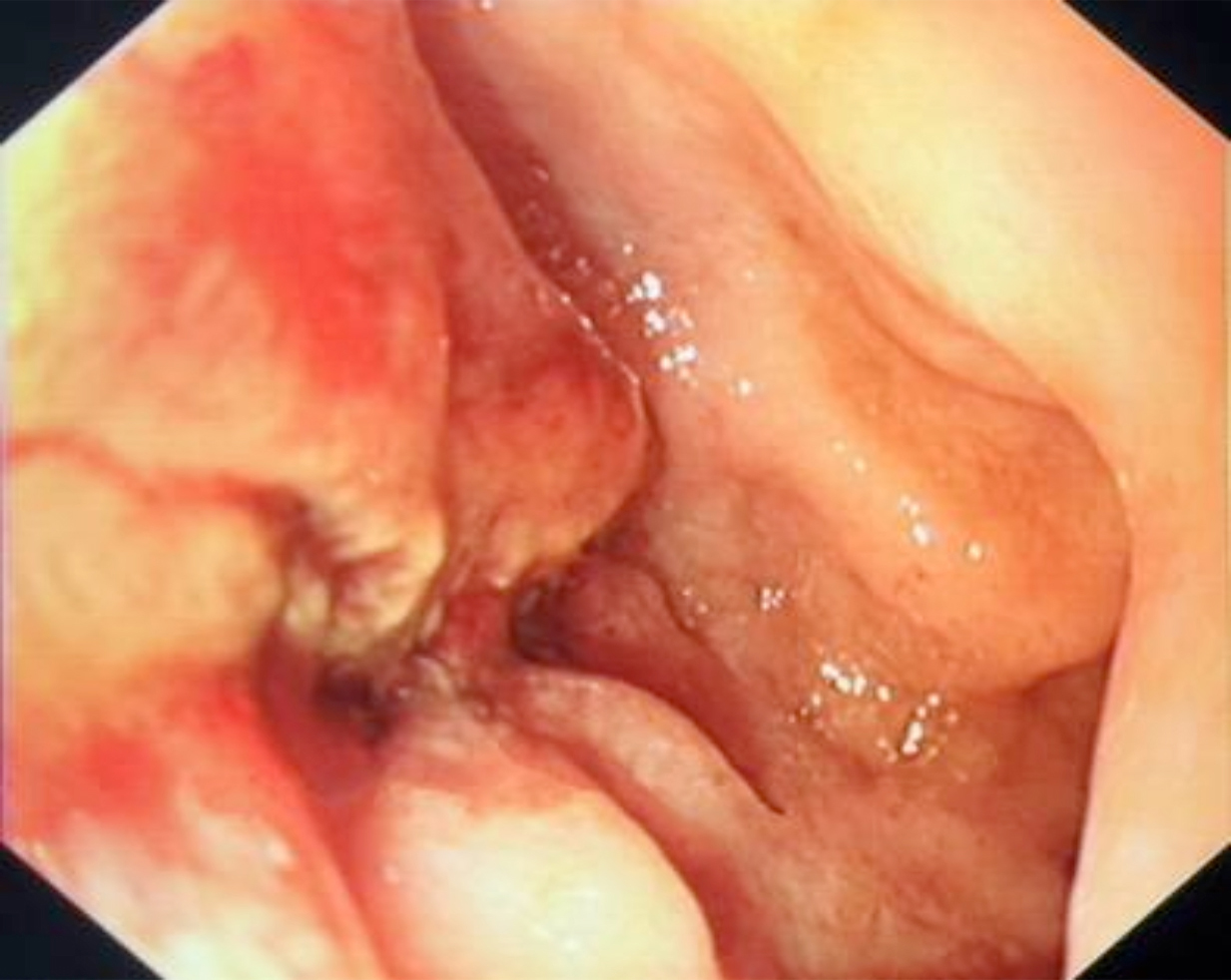 Figure 3: Endoscopic view after oversewing. The bleeding has ceased.
Figure 3: Endoscopic view after oversewing. The bleeding has ceased.
For patients with acute upper GI bleeding, venous access should be established immediately. It is recommended to insert a central venous catheter. For hemodynamically unstable patients, fluid resuscitation has priority over endoscopy. An emergent endoscopic examination should be performed as soon as possible after hemodynamic disturbances are corrected by fluid resuscitation. According to the amount of blood loss, a sufficient amount of fluid should be administered in a short time to correct the shortage of circulating blood volume. Transfusion of red cells should be considered when the hemoglobin level falls below 7 g/dL.
Most PU bleeding can be controlled with acid-suppressing drugs and therapeutic endoscopy. However, a risk of re-bleeding exists. When re-bleeding occurs, it can be treated by repeated therapeutic endoscopy, but eventually, some patients will need surgery.6 Surgery is still the most reliable way to halt bleeding from PUs, despite great progress in endoscopic technologies and drug treatment. The traditional surgical method is open abdominal surgery. However, patients with GIl bleeding who have failed non-surgical treatment, usually are in a critical condition, which increases the risks of surgical complications. Therefore, the use of minimally invasive surgery is preferable. Compared with open abdominal surgery, laparoscopic surgery has the advantages of the smaller incisions, less postoperative pain, and faster recovery. In this case, we performed laparoscopic oversewing of the duodenal ulcer under endoscopic guidance to stop the bleeding. The procedure was done with only three ports, which resulted in little postoperative pain, minimal cost, and fast recovery. We suggest that, for patients with recurrent bleeding from PUs, laparoscopic oversewing under video control with endoscopic guidance is the preferred treatment option, as it is more reliable than simple endoscopic treatment to halt bleeding.
PATIENT’S CONSENT:
Informed consent was obtained from the patient to publish the data concerning this case.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
FC: Surgery, paper writing, and literature review.
SZ: Literature review and manuscript revision.
All the authors approved the final version of the manuscript to be published.
REFERENCES
- Alzoubaidi D, Lovat LB, Haidry R. Management of non-variceal upper gastrointestinal bleeding: Where are we in 2018? Frontline Gastroenterol 2019; 10(1):35-42. doi: 10. 1136/flgastro-2017-100901.
- Van Leerdam ME. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol 2008; 22(2):209-24. doi: 10.1016/j.bpg.2007.10.011
- Patel V1, Nicastro J. Upper gastrointestinal bleeding. Clin Colon Rectal Surg 2020; 33(1):42-4. doi: 10.1055/s-0039- 1695037.
- Fujishiro M, Iguchi M, Kakushima N, Kato M, Sakata Y, Hoteya S, et al. Guidelines for endoscopic management of non-variceal upper gastrointestinal bleeding. Dig Endosc 2016; 28(4): 363-78. doi: 10.1111/den.12639.
- Miilunpohja S, Karkkainen J, Hartikainen J, Jyrkka J, Rantanen T, Paajanen H. Need of emergency surgery in elderly patients with upper gastrointestinal bleeding: Survival analysis during 2009-2015. Dig Surg 2019; 36(1):20-26. doi: 10.1159/000485846.