Post-traumatic Renal Arteriovenous Malformation Discovered after 2 Years of Blunt Trauma: Diagnosis and Management
By Tariq Javed1, Zehra Kazmi2, Amna Butt1, Waqas Rahim1, Mohammad Ayaz Khan1Affiliations
doi: 10.29271/jcpsp.2022.04.82ABSTRACT
Blunt trauma to the kidney is usually minor and self-limiting. In some cases, the patient may present with intractable hematuria or persistent flank pain and discomfort, which necessitates aggressive management. It is very rare and unusual to find a renal arterio-venous malformation following blunt trauma. This unusual presentation should be kept in mind when a patient presents with hematuria and history of blunt abdominal trauma.
We report the case of a young male who suffered blunt abdominal trauma two years back, and continued to have on-and-off hematuria. After extensive work up, a diagnosis of renal arterio-venous malformation was made. His case was managed promptly with renal angio-embolization.
Key Words: Blunt trauma, Arterio-venous malformation (AVM), Angio-embolisation, kidney.
INTRODUCTION
Hematuria is a frequent presenting feature in patients visiting urology clinics. Some common differentials of this presenting complaint include urinary tract infection, trauma, urolithiasis and urologic neoplasms.
Iatrogenic trauma is the underlying cause of approximately 60% of renal vascular injuries, with stab wounds being the most frequent cause.1 Blunt trauma has rarely been implicated. However, post-traumatic renal arterio-venous malformations (AVMs) are abnormal communicating channels between the intra-renal arterial and venous systems.2 Together, these account for some rare causes of gross hematuria.
We describe the case of a 20-year male patient who presented with intractable gross hematuria. Consistent with a remote history of blunt abdominal trauma, he was subsequently diagnosed with renal AVM and managed accordingly. His consent was taken for the publication of this case report.
CASE REPORT
A 20-year, unmarried male patient, secondary school student, was referred to us with complaints of right flank pain and gross hematuria for 12 days. He reported having on-and-off hematuria with clots for the past two years, but these issues were always managed conservatively. His abdomen was soft and flat, with no costovertebral angle tenderness. No vascular bruit was audible on his abdomen.
History was significant for blunt abdominal trauma in 2017 (run over injury by a bull). He was managed in a rural hospital, where the renal injury was recorded as grade I. He recalled an episode of painless hematuria at that time, which resolved with conservative measures and bed rest. No other significant past medical or surgical history, no known allergies or addictions, and no significant family history were elucidated.
When he presented to us, a 3-way Foley’s catheter was inserted and bladder irrigation and intravenous hydration were started. Complete bed rest was advised. All baseline investigations were within normal limits (Table I). Urinalysis showed plenty of red blood cells (>30/high power field). Urine culture was negative.
Doppler ultrasound of the kidneys and urinary bladder was done on the day of admission. It showed minimal calyceal fullness with dilated thick-walled proximal ureter (Figure 1). The upper tract showed raised echogenicity and clots; the urinary bladder was filled with 35 ml of organised clots, demonstrating low internal echoes (Figure 2).
Table I: Baseline laboratory investigations.|
Dates |
Hb/Hct (g/dl) |
TLC (/UL) |
PLT (x103/ml) |
BUN (mg/dl) |
Cr (mg/dl) |
PT/INR (seconds) |
APTT (seconds) |
CRP (mg/L) |
|
31-01-2020 |
11/32.1 |
9,420 |
432 |
10 |
1.0 |
12.4/1.14 |
- |
- |
|
01-02-2020 |
9.0/26.4 |
11,110 |
371 |
- |
- |
13.10/1.21 |
30.40 |
- |
|
03-02-2020 |
9.7/28.3 |
8150 |
421 |
- |
- |
- |
- |
- |
|
04-02-2020 |
- |
- |
- |
- |
1.39 |
11.40/1.05 |
28.10 |
8.71 |
|
05-02-2020 |
8.2/24.9 |
8500 |
342 |
- |
1.45 |
- |
- |
16.35 |
|
06-02-2020 |
8.9/27.1 |
8990 |
400 |
- |
1.3 |
- |
- |
- |
|
Hb: Hemoglobin, Hct: Hematocrit, TLC: Total leucocyte count, Plt: Platelets, BUN: Blood urea nitrogen, Cr: Creatinine, PT: Prothrombin time, INR: International normalised ratio, APTT: Activated partial thromboplastin time, CRP: C-reactive protein. |
||||||||
 Figure 1: Ultrasound demonstrating mild right hydronephrosis and hydroureter.
Figure 1: Ultrasound demonstrating mild right hydronephrosis and hydroureter.
 Figure 2: Organised debris with low internal echoes and Foley’s catheter bulb in the urinary bladder.
Figure 2: Organised debris with low internal echoes and Foley’s catheter bulb in the urinary bladder.
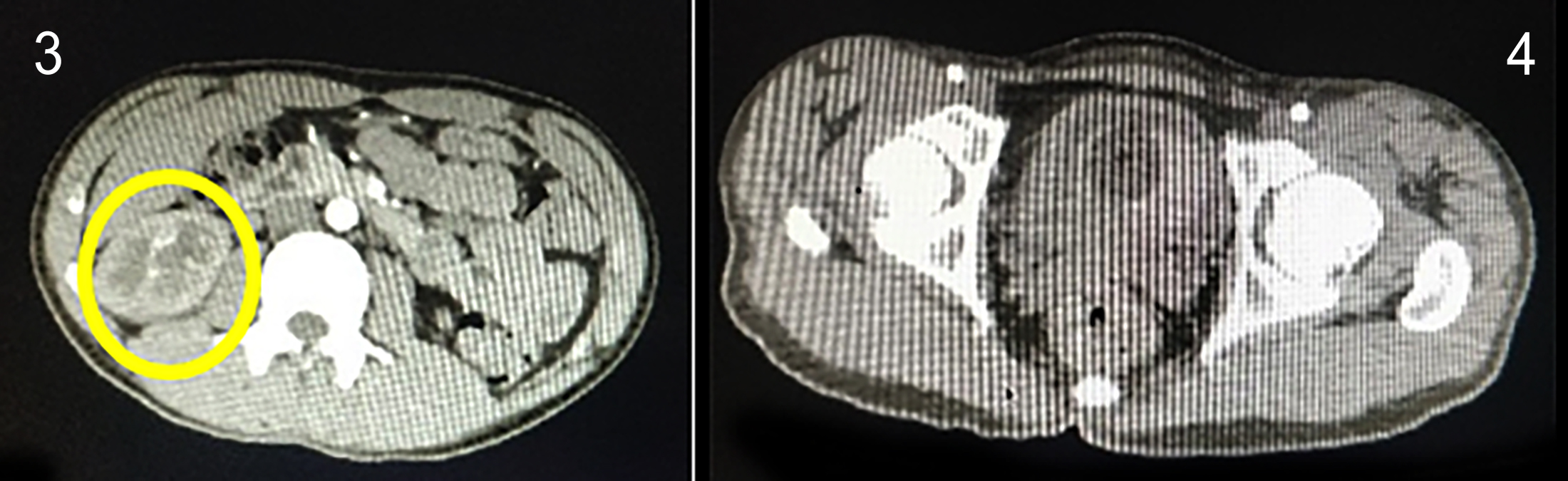 Figures 3 & 4: Contrast CT scan showing an arteriovenous malformation between the intra-renal arterial & venous systems of the right kidney. Organised clots are seen in the urinary bladder.
Figures 3 & 4: Contrast CT scan showing an arteriovenous malformation between the intra-renal arterial & venous systems of the right kidney. Organised clots are seen in the urinary bladder.
CT scan of the abdomen and pelvis with contrast was done. It showed mild right hydronephrosis and hydroureter, and a hyperdense area in the right pelvi-calyceal system up to the right ureterovesical junction, suggestive of blood clot (Figures 3, 4). Subsequently, a CT renal angiogram was done, which showed an AVM between the right inter-polar vessels.
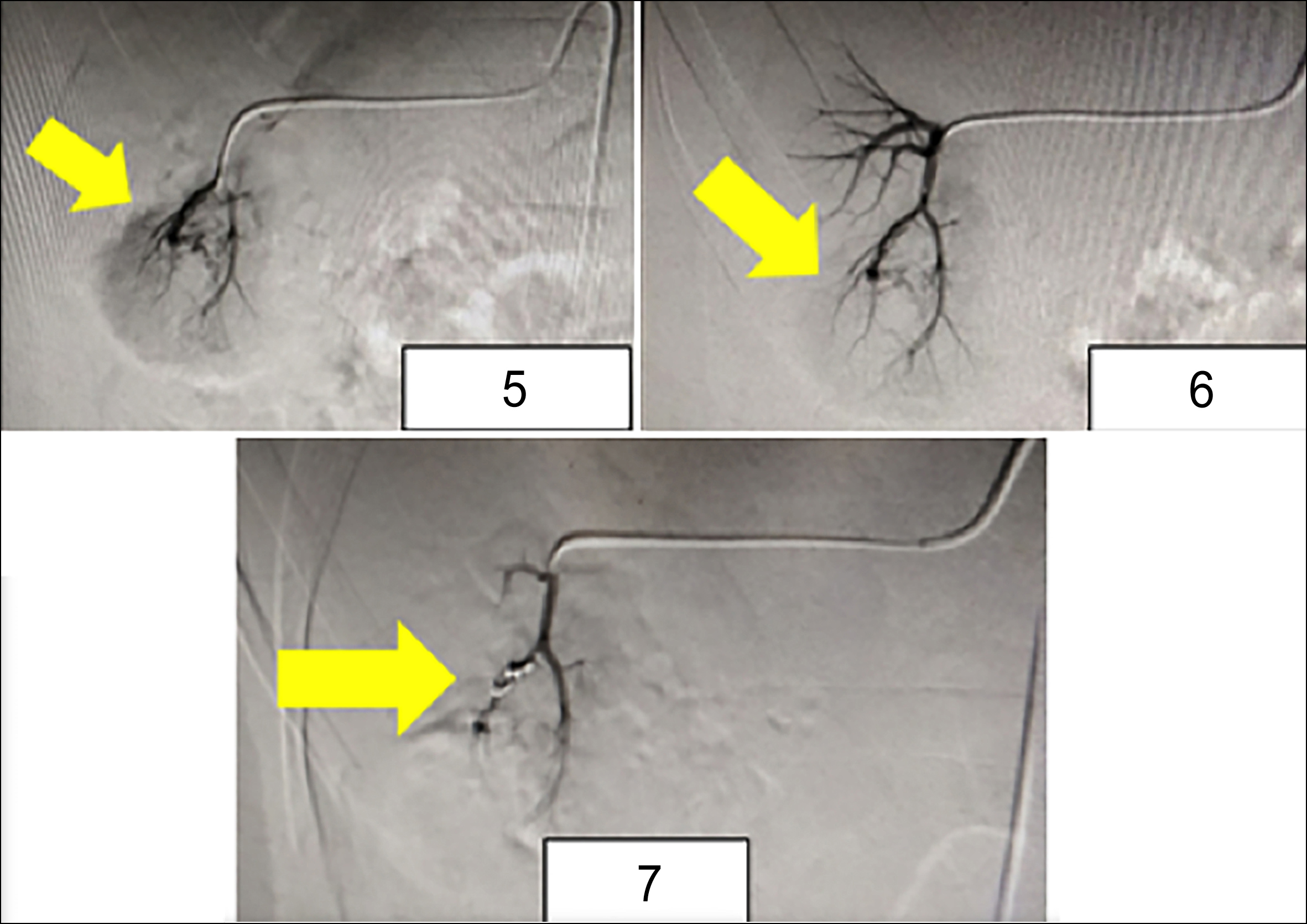 Figures 5, 6 & 7: Demonstrating segmental renal artery angio-embolisation (Figure 5); Complete resolution of the vascular blush (Figure 6); Platinum coil in place (Figure 7).
Figures 5, 6 & 7: Demonstrating segmental renal artery angio-embolisation (Figure 5); Complete resolution of the vascular blush (Figure 6); Platinum coil in place (Figure 7).
After detailed patient counselling, right renal angio-embolisation was performed (Figures 5, 6). A platinum coil was inserted into one of the segmental branches, ensuring minimal parenchymal loss (Figure 7).
Post-procedure, the patient was kept on complete bed rest, intravenous hydration and prophylactic antibiotics. He showed complete resolution of hematuria on serial sampling after 12 hours, and was discharged the same day, uneventfully. The patient has been doing well in all subsequent follow-up visits, and reports no residual pain or lower urinary tract symptoms. He has been advised to continue with long-term follow-up, to watch for recurrence which may happen due to collateral circulation or even re-canalisation of the abnormal communication.
DISCUSSION
We presented a case of renal AVM after blunt trauma. The patient came to us two years later with persistent gross hematuria. Renal AVM is a very rare phenomenon with less than 200 cases reported in the literature, and 75% of those present with hematuria. Congenital AVMs are known to occur with Osler-Weber-Rendu disease (OWRD).3 Blunt trauma to the abdomen is a known, albeit rare risk factor for visceral AVMs.4 Some of these patients present with hematuria, as was the case with this patient. Other presentations may be systolic or diastolic hypertension in 46–50% of cases, and 5% may present as high output cardiac failure.2
The unique aspect of this case was the delayed presentation. Most renal AVMs are not so quiescent. However, this patient presented two years after the initial inciting event, and that is not a very common presentation for this already rare condition. Appropriate radiologic imaging is valuable in the detection of these rare malformations; and understanding of the intricate vascular anatomy helps in appropriate and prompt management.5 Acquired renal AVMs are also known as arteriovenous fistulas. Acquired ones account for 70 to 75% of all cases. Most common etiologic factors are from iatrogenic trauma during renal biopsy or surgery.4 These may also occur due to blunt or penetrating trauma, pyelonephritis or as a complication of renal-cell carcinoma; all of which have been reported as rare causes of this anomaly. Idiopathic renal AVM makes up only 5% of all cases. It is thought to be caused by spontaneous erosion or rupture of a renal artery into a neighbouring renal vein.7
The historical treatment is a partial nephrectomy. Interventional radiology has revolutionised their management, and many options of endovascular therapy now exist. Management of intra-renal vascular injury via therapeutic embolisation was first described by Bookstein and Goldstein in 1973 and has been considered an effective form of treatment ever since.6 Coor P et al. reported certain complications of renal AVM embolisation; renal branch intimal dissection in three cases, contrast extravasation in three and ectopic coil placement in two. Post-embolisation pyrexia occurred in one case.7 Earlier reports on endovascular treatment of renal AVMs describe embolisation techniques using gel foam, ethanol, or histoacryl.1
Current indications for trans-catheter renal artery embolisation include hemorrhage resulting from trauma or renal tumor, renal AVMs, end-stage renal disease, severe hypertension refractory to other methods of treatment, and recurrent infected hydronephrosis in a patient with hemophilia.6 The most serious complication after embolisation is the risk of renal infarction. With the advent of the super-selective technique, this risk has now been reduced to 9%.8
In conclusion, renal AVMs are very rare and should be kept in mind when evaluating a patient with hematuria. The treatment of post-traumatic renal AVMs is challenging. The option of endovascular management is a safe and feasible modality, and ensures adequate organ preservation. Long-term follow-up is recommended to monitor the patient for recurrences.
PATIENT’S CONSENT:
Informed consent was obtained from the patient to publish the data concerning this case.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
TJ: Developed the concept of the study.
ZK: Designed and written the manuscript.
AB: Literature review.
WR: Data acquisition.
MAK: Primary surgeon, case supervision.
All contributed to the manuscript review.
REFERENCES
- Inui T, Frankel D. Renal arteriovenous malformations: A rare vascular cause of back pain. Ann Vasc Surg 2017; 42:62. e9-62.e11. doi: 10.1016/j.avsg.2017.03.001. doi: 10.1016/j. avsg.2017.03.001.
- Gandhi SP, Patel K, Pandya V, Raval M. Renal arteriovenous malformation presenting with massive hematuria. Radiol Case Rep 2015; 10(1):1068. doi: 10.2484/rcr.v10i1.1068.
- Cura M, Elmerhi F, Suri R, Bugnone A, Dalsaso T. Vascular malformations and arteriovenous fistulas of the kidney. Acta Radiologica 2010; 51(2):144-9. doi: 10.3109/0284185 0903463646.
- Murata S, Onozawa S, Nakazawa K, Akiba A, Mine T, Ueda T, et al. Endovascular embolisation strategy for renal arteriovenous malformations. Acta Radiol 2014; 55(1):71-7. doi: 10.1177/0284185113493085.
- Eom HJ, Shin JH, Cho YJ, Nam DH, Ko GY, Yoon HK, et al. Transarterial embolisation of renal arteriovenous malformation: Safety and efficacy in 24 patients with follow-up. Clin Radiol 2015; 70(11):1177-84. doi:10.1016/j.crad.2015.06. 079.
- Lee SY, Do YS, Kim CW, Park KB, Hwan Kim Y, Cho YJ, et al. Efficacy and safety of transvenous embolization of type II renal arteriovenous malformations with coils. J Vasc Interv Radiol 2019; 30(6):807-12. doi:10.1016/j.jvir.2018.09.019.
- Corr P, Hacking G. Embolisation in traumatic intrarenal vascular injuries. Clin Radiol 1991; 43(4):262-4. doi: 10.1016/ s0009-9260(05)80252-1.
- Wakefield MR. Julie MR, Carrie EY, Renal arteriovenous malformation. http://emedicine.medscape.com/article/4628 85-treatment#a1128 Updated: Feb 27, 2014.