Pompe Disease Complicated with Appendicular Torsion: A Rare Concurrence
By Shujian Zhang1, Xue Luan2, Huiwen Li3, Dongming Piao4, Zhengyong Jin3,5Affiliations
doi: 10.29271/jcpsp.2022.Supp.S134ABSTRACT
Pompe disease, also known as Glycogen Storage Disease Type II, is a rare disorder of glucose metabolism caused by congenital acid alpha-glucosidase (GAA) deficiency. A large amount of glycogen accumulates in the lysosomes, causing these to swell and rupture. Its incidence is about 1 in 40,000 to 1 in 50,000 newborns. The main features are hypotonia and cardiomyopathy. Only a few clinical cases of Pompe disease have been reported, and appendicular torsion has rarely been observed. Herein, we report a case of Pompe disease combined with appendicular torsion, both of which were diagnosed on autopsy pathology. The clinical diagnosis of this disease is difficult in developing countries, and it is mostly misdiagnosed as other types of heart disease. Once the clinical symptoms worsen, most of them die within a short period. Therefore, screening for neonatal genetic metabolic diseases for early diagnosis and treatment should be carried out.
Key Words: Glycogen storage disease type II, Metabolic disease, Enzyme replacement therapy, Neonatal screening.
INTRODUCTION
Pompe disease is a rare disorder of glucose metabolism caused by congenital acid alpha-glucosidase (GAA) deficiency.1,2 Owing to the lack of GAA in children with Pompe disease, glycogen cannot be decomposed. The glycogen is released into the cytoplasm, and the organelles swell, resulting in the deterioration of cell structure and function, causing injury to a variety of tissues such as the myocardium, skeletal muscle, and liver.3 The torsion of the appendix is a relatively rare event and occurs mostly in children. The appendix itself rotates around its longitudinal axis, obstructing its cavity and its mesenteric blood supply.4 Herein, we report a case of Pompe disease combined with appendicular torsion, both of which were diagnosed on autopsy pathology.
CASE REPORT
A 1.5-year girl was admitted to the hospital with fever for five days and blood in the stool for one day. Penicillin was administered at another hospital for five days without improvement.
A day before admission, fever was accompanied by blood in the stool, which was bright red and heavy; therefore, she reported to our hospital. During the illness, she was poorly fed and sleepy, with little urination. On admission, a physical examination revealed body temperature of 37.4°C, respiratory rate, 66 breaths/min, and pulse, 88 beats/min. She had a pale complexion, cyanotic lips, drowsiness, flat and soft abdomen, no tenderness, rebound pain 6 cm below liver ribs, and medium quality grade IV muscle strength, with no obvious abnormality in other physical examinations. Laboratory examination showed white blood cells of 12.6×109/l, neutrophil ratio was 0.48%, lymphocyte ratio was 0.55%, haemoglobin was 105 g/L, and platelets were 178×109/L. Fasting blood glucose was 4.72 mmol/L, aspartate aminotransferase: 449 IU (normal range: 0–40), alanine aminotransferase: 198 IU (normal range: 0–40), creatinine kinase: 1226 IU (normal range: 25–196), CK-MB: 198 IU (normal range: 0–25), lactate dehydrogenase: 405 IU (normal range: 115–220), and hydroxybutyrate dehydrogenase: 1775 IU (normal range: 72–182). Electrocardiogram revealed left ventricular hypertrophy and myocardial injury. Color doppler echocardiography revealed significant enlargement of the left ventricle, interventricular septum, posterior wall of the left ventricle, and thickening of the right anterior wall of the left ventricle. Abdominal B-ultrasound demonstrated an enlarged liver.
After admission, the child’s condition further worsened, and she became unconscious. The clinical death was announced 17 h after admission. The autopsy results revealed that the heart was enlarged and spherical, weighing 136 g (52 g in normal children of the same age). Moreover, the left ventricle wall thickness was 14 mm (normally 6 mm), the ventricular septum was 12 mm (normal infants ≤4 mm), the right ventricle was 4 mm thick, with the liver weighing 372 g (normal for children of the same age), with a smooth surface. The appendix was 7 cm long, and the surface was hyperemic. There was a fava bean-sized hole in the mesentery 1 cm from the root. The appendix was twisted 720° clockwise along this hole. Microscopic examination revealed that the left ventricular wall, papillary muscle, and ventricular septal cardiomyocytes were generally enlarged, and most of the myocardial cytoplasm contained round vacuoles of varying sizes (Figure 1). The sinusoids were dilated and congested, and vacuoles of varying sizes were observed in the cytoplasm of some liver cells (Figure 2). In the appendix, vasodilation and congestion were noted, and the mucosal layer of the appendix was necrotic at the twisting point. The pathological diagnosis confirmed it as Pompe disease and 720° appendicular torsion.
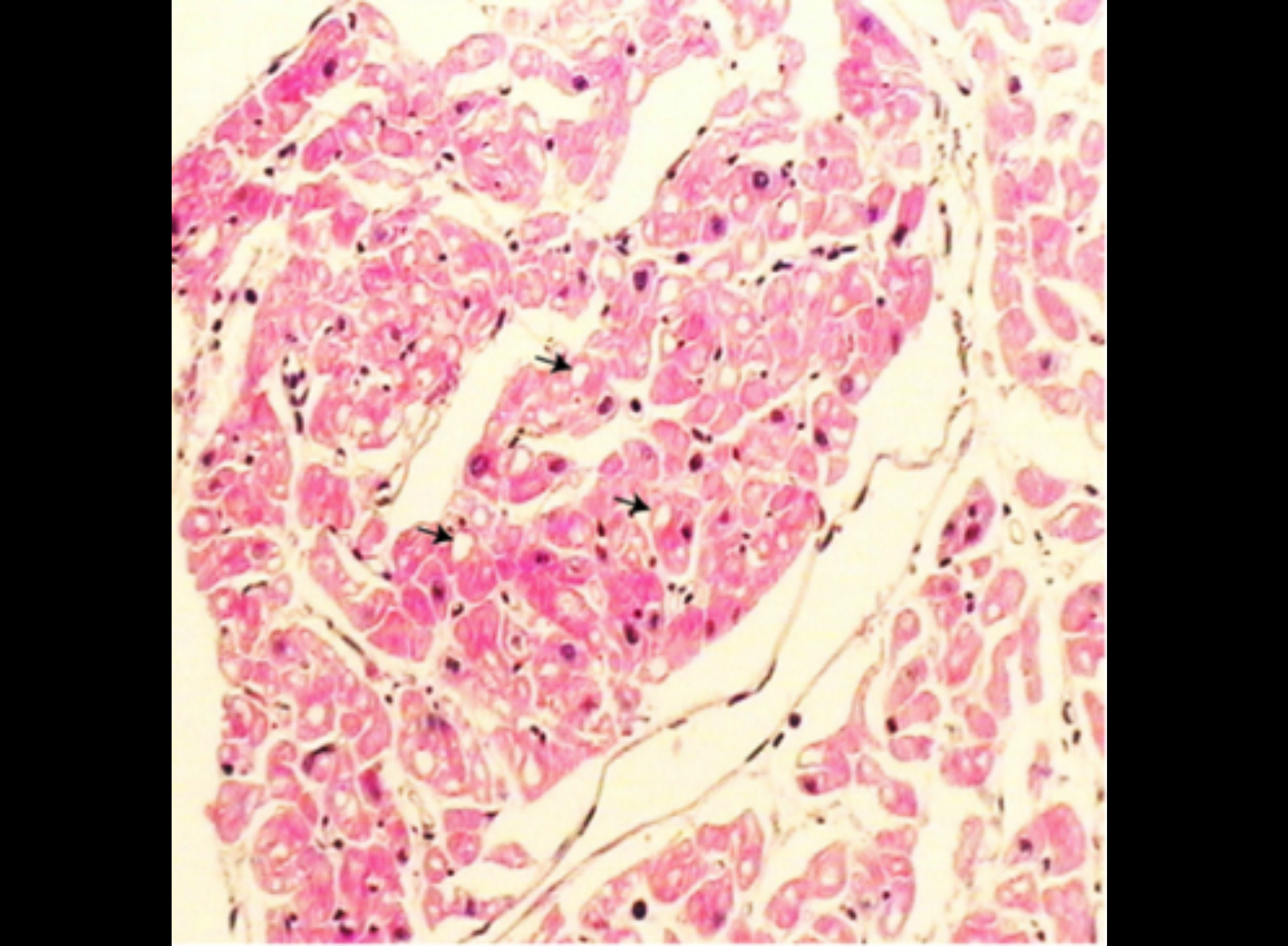 Figure 1: HE staining of cardiomyocytes showing vacuoles of variable sizes in the cytoplasm of cardiomyocytes (arrows). (HE, ×100).
Figure 1: HE staining of cardiomyocytes showing vacuoles of variable sizes in the cytoplasm of cardiomyocytes (arrows). (HE, ×100).
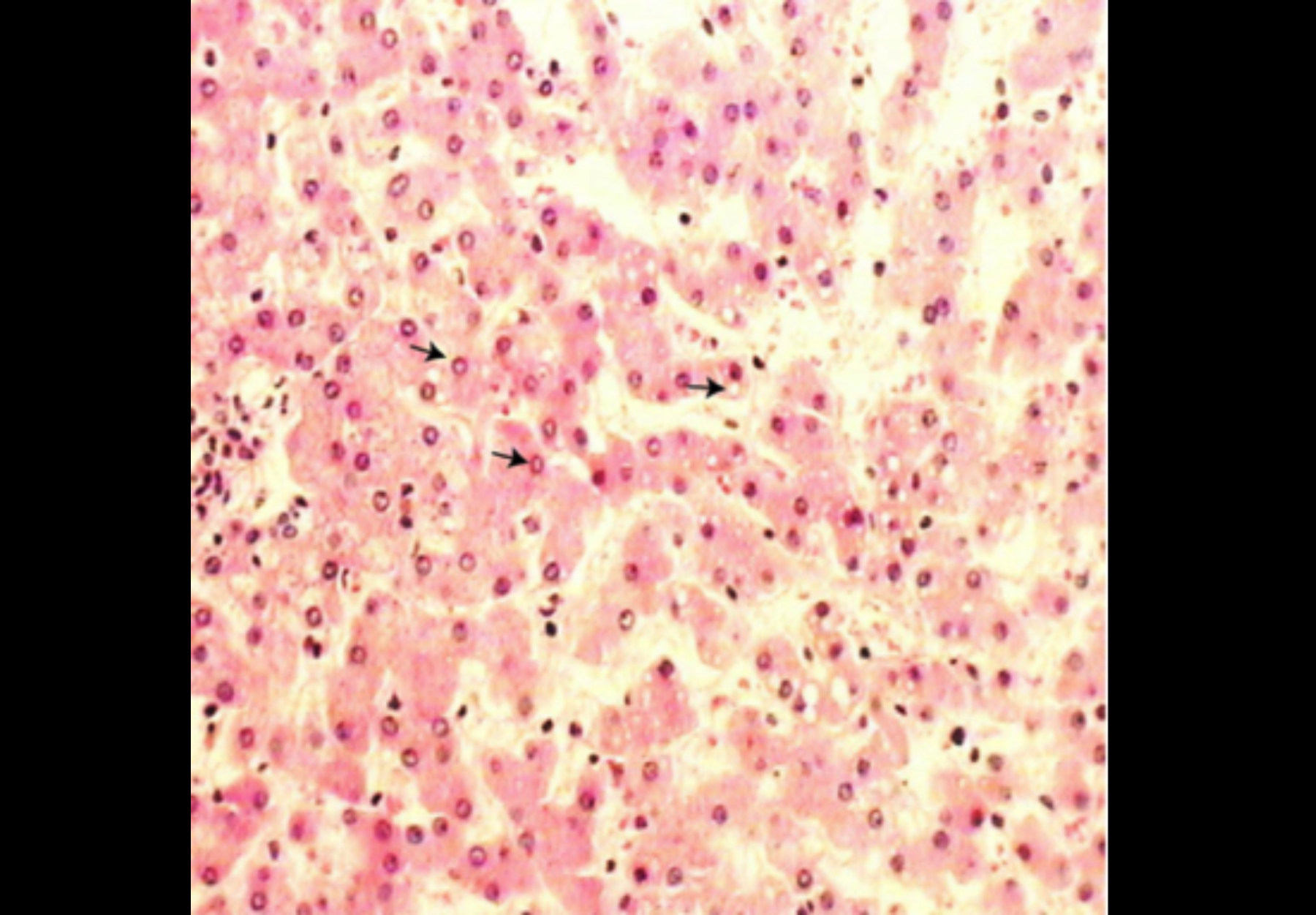 Figure 2: HE staining of liver cells showing vacuoles of variable sizes in the cytoplasm of some hepatocytes (arrows). (HE, ×100).
Figure 2: HE staining of liver cells showing vacuoles of variable sizes in the cytoplasm of some hepatocytes (arrows). (HE, ×100).
DISCUSSION
According to the age of onset, Pompe’s disease is divided into early and late-onset, which mainly depends on the residual GAA activity in the body. The lower the GAA activity, the earlier the age of onset, and the more severe the clinical symptoms.5 Infant type usually develops within 12 months after birth. The disease progresses rapidly, showing progressive muscle weakness, respiratory insufficiency, and frequent respiratory infections. Heart color doppler ultrasound indicates significant enlargement of the heart and thickening of the ventricles and ventricular septum, often secondary to hypertrophic cardiomyopathy.2,6 Most children die of heart failure and bulbar palsy within two years of age.
Pompe disease develops rapidly and has a low survival rate; therefore, early diagnosis is critical. Currently, the diagnosis is primarily through muscle biopsy and the detection of GAA enzyme activity in fibroblasts. However, the location of the muscle biopsy will affect the test results. Kishnani et al. reported that the combination of urine glycogen-derived glucose 4 (GLc4) and dried blood spot filter paper detection has a diagnostic rate of approximately 100% for Pompe disease.7 This method is suitable for newborn screening.8 However, it has not yet been widely used.
Enzyme replacement therapy (ERT) is considered the most promising treatment method, which can improve the function of the heart and minimise the damage of skeletal muscle. However, the clinical trials of ERT are ongoing; thus, the treatment plan still needs further research.
Torsion of the appendix is also rare and occurs mainly in children. It is related to appendix length, faecal stones, tumours and parasites. Similar to the symptoms of acute appendicitis, torsion of the appendix develops suddenly, and the symptoms and signs aggravate rapidly. This case of appendicular volvulus is mainly related to the length of the appendix and the mesenteric hole. After the volvulus, the degree of obstruction and coma of the child concealed some of the symptoms. Therefore, it was not clinically detected in time.
In conclusion, Pompe’s disease can have an early onset, rapid progression, challenging clinical diagnosis, and high mortality. Therefore, newborn screening is essential for early diagnosis. Treatment initiation before irreversible damage occurs appears useful to maximise the life span.
PATIENT’S CONSENT:
Informed consent was obtained from the patient’s parents to publish the data concerning this case.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’CONTRIBUTION:
SZ: Concept, design, definition and intellectual content, literature search, data acquisition, data analysis, and manuscript preparation and editing.
XL: Design, manuscript preparation, and editing.
HL: Design, manuscript preparation, and editing.
DP: Concept, design, definition and intellectual content.
ZJ: Concept, design, definition and intellectual content.
All the authors have approved the final version of the manuscript.
REFERENCES
- van der Ploeg AT, Reuser AJ. Pompe’s disease. Lancet 2008; 372(9646):1342-53. doi:10.1016/s0140–6736(08)61 555-x.
- Taverna S, Cammarata G, Colomba P, Sciarrino S, Zizzo C, Francofonte D, et al. Pompe disease: pathogenesis, molecular genetics and diagnosis. Aging (Albany NY) 2020; 12(15):15856-74. doi:10.18632/aging.103794.
- Turaça LT, de Faria DO, Kyosen SO, Teixeira VD, Motta FL, Pessoa JG, et al. Novel GAA mutations in patients with Pompe disease. Gene 2015; 561(1):124-31. doi: 10.1016/ j.gene.2015.02.023.
- Kilincaslan H, Gedik AH, Bilici M, Cakir S. Rare case of an abdominal mass presenting as acute abdomen: Torsion of the vermiform appendix. Pediatr Int 2013; 55(2):e14-6. doi:10.1111/j.1442–200X.2012.03746.x.
- Kishnani PS, Hwu WL, Mandel H, Nicolino M, Yong F, Corzo D. A retrospective, multinational, multicenter study on the natural history of infantile-onset Pompe disease. J Pediatr 2006; 148(5):671-6. doi:10.1016/j.jpeds.2005.11.033.
- Dasouki M, Jawdat O, Almadhoun O, Pasnoor M, McVey AL, Abuzinadah A, et al. Pompe disease: Literature review and case series. Neurol Clin 2014; 32(3):751-76. doi:10.1016/j. ncl.2014.04.010.
- Kishnani PS, Steiner RD, Bali D, Berger K, Byrne BJ, Case LE, et al. Pompe disease diagnosis and management guideline. Genet Med 2006; 8(5):267-88. doi:10.1097/01. gim.0000218152.87434.f3.
- Chien YH, Lee NC, Thurberg BL, Chiang SC, Zhang XK, Keutzer J, et al. Pompe disease in infants: Improving the prognosis by newborn screening and early treatment. Pediatrics 2009; 124(6): e1116-25. doi: 10.1542/peds. 2008–3667.