Pleomorphic Adenoma of Minor Salivary Gland
By Sahar Usman, Sufyan Ahmed, Sana Iqbal, Ayesha AslamAffiliations
doi: 10.29271/jcpsp.2022.04.70ABSTRACT
Pleomorphic adenoma is a benign tumor of salivary glands, arising from minor salivary glands, is very rare and presents with a minor female predilection; and the highest occurrence is between the fourth and sixth decades of life. It is of glandular origin, usually presenting as a slowly growing, painless, firm swelling that does not cause ulceration of the overlying mucosa. In this case, a 27-year male presented with swelling on buccal mucosa for three years. The swelling was firm and well circumscribed. Excisional biopsy was done under general anesthesia and the mass was excised. The histopathological evaluation revealed pleomorphic adenoma. This case highlights the need to keep this entity in the differential diagnosis of intra-oral indolent swellings of some duration.
Key Words: Pleomorphic adenoma, Buccal mucosa, Minor salivary glands.
INTRODUCTION
Pleomorphic adenoma (PA) is defined by the World Health Organization as a benign tumor composed of pleomorphic or mixed type of tissues including epithelial tissue intermingled mucoid, myxoid, and chondroid tissues.1 PA is a benign, mixed tumor that typically involves the parotid gland. About 8% of PAs involve minor salivary glands and the palate is the most common region (60–65%). PA occurs in other minor salivary gland sites, including the lip, buccal mucosa, and tongue. PAs of minor salivary glands commonly occur in the fourth and sixth decades of life with a minor predominance in female patients. In children and adults, these are very rare. PAs are commonly present as slowly growing, painless, fixed swellings that do not cause ulceration of the overlying mucosa.1 The treatment of choice for PA is surgical removal with clear margins to prevent a recurrence. The follow-up is mandatory because of the risk of recurrence.2 The purpose of this case presentation is to share our experience of a PA of a buccal minor salivary gland.
CASE REPORT
A 27-year male presented to the Maxillofacial Surgery Section of our hospital with the presenting complaint of swelling in the left cheek for three years, which slowly increased over time. The swelling was firm, well-circumscribed, and not attached to underlying tissue. There was no pain on palpation or any other associated symptoms. Regional lymphadenopathy was also not present. In an extra-oral examination, there was no facial asymmetry. An introverted dome-shaped, oval enlargement with an uneven surface was present on the right cheek region. No abnormality was noticed in the overlying skin. On intra-oral examination, the swelling was of the same color as the buccal mucosa; it was soft to firm in consistency, non-fluctuant, and non-tender (Figure 1). Local temperature over the swelling was not elevated. The patient was advised for hematological investigations and biopsy. The hematological investigations were normal. The excisional biopsy was performed under general anesthesia and the mass was excised. In the gross description, it consisted of a single tan-pink nodular tissue piece that measured 2.5×1.7×1.5 cm and the cut surface showed a grey-white firm lesion that measured 2.4×1.6×1.5 cm (Figure 2). It was less than 0.1 cm away from the outer painted surface. In the microscopic examination, it revealed a well-demarcated biphasic lesion composed of epithelial cells admixed with mesenchymal elements. The epithelial component was forming ducts, lined by a double layer of epithelium; and the mesenchymal component was present in the form of chondromyxoid areas (Figure 3). This confirmed the diagnosis of PA. The swelling was removed completely with an adequate boundary of normal tissue. The patient was counselled for follow-up for observation and detection of early recurrence.
 Figure 1: The intra-oral appearance of swelling with the same color as that of surrounding buccal mucosa.
Figure 1: The intra-oral appearance of swelling with the same color as that of surrounding buccal mucosa.
 Figure 2: Gross appearance of the excised mass showing single tan-pink nodular tissue piece measuring 2.5×1.7×1.5 cm in size.
Figure 2: Gross appearance of the excised mass showing single tan-pink nodular tissue piece measuring 2.5×1.7×1.5 cm in size.
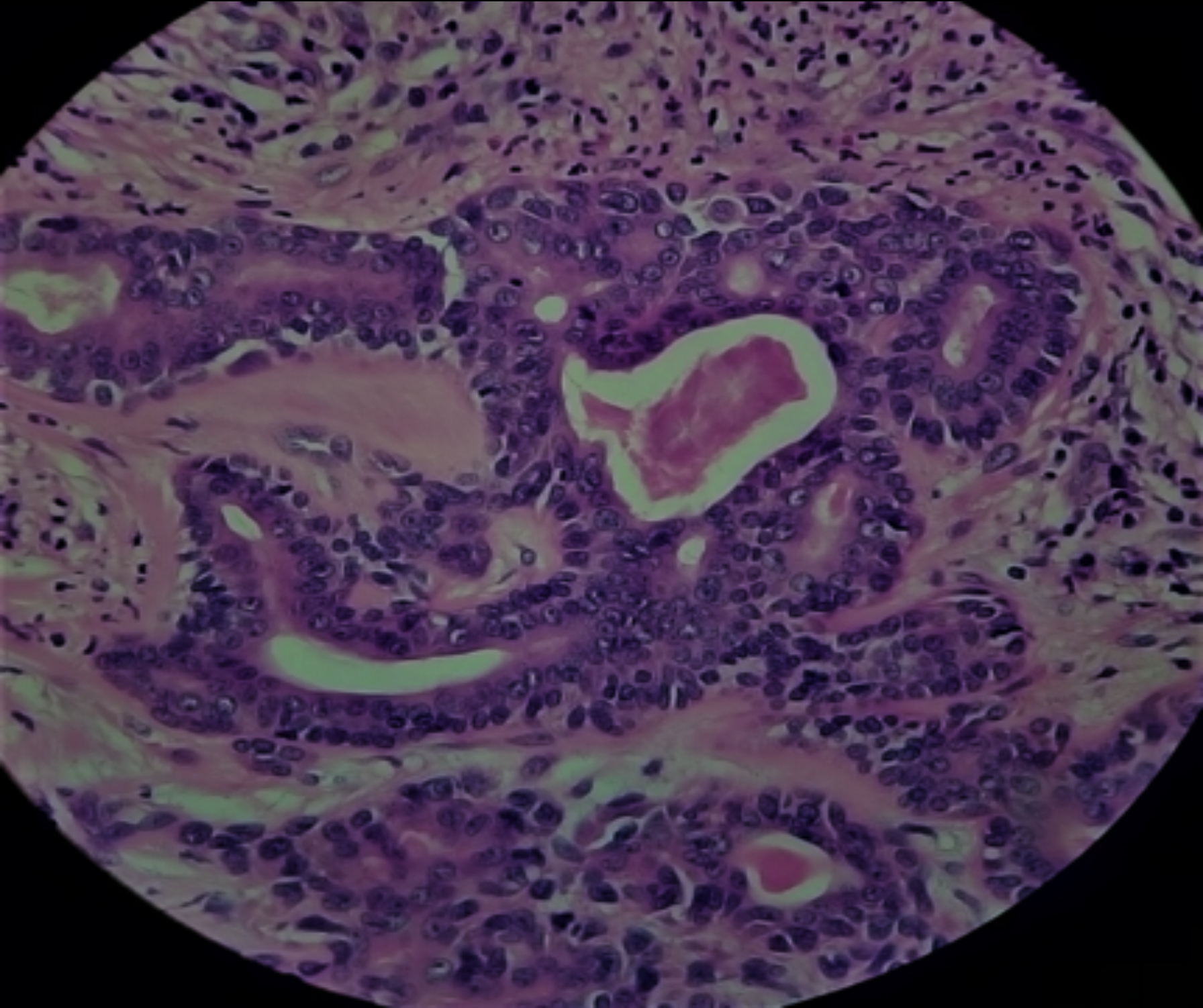 Figure 3: Microscopically, the tumor was composed of epithelial glands with myxoid and chondromyxoid elements tissue stroma.
Figure 3: Microscopically, the tumor was composed of epithelial glands with myxoid and chondromyxoid elements tissue stroma.
DISCUSSION
Tumors of the salivary glands represent fewer than 5% of all head and neck tumors; and two-thirds of these tumors are PAs. PA is a benign salivary gland tumor with a wide cytomorphologic architectural variety. It is a common salivary gland tumor that arises from both major and minor salivary glands. The parotid gland is the most common site of PA. The cause of salivary gland tumors remains unclear, but ionising radiation has been recognised as a risk factor. The patient usually comes with the chief complaint of a small, painless, slowly growing nodule which slowly begins to increase in size, occasionally showing intermittent growth. The skin rarely ulcerates, even though these tumors may reach a very large size.3 Pain is not a common symptom. The size of the tumors ranges from 1 to 7 cm with some PAs of the cheek reaching bigger sizes. PAs of minor salivary glands are noticed and treated earlier than that of major salivary glands. In our case, the tumor was tolerable to grow to a considerable size as it did not restrict the deglutition and speech. Advanced imaging techniques, like computed tomography and ultrasonography, deliver information about location, size, and metastasis of the tumor to adjacent structures. In this case, on clinical examination, a differential diagnosis of fibroma was also considered, given the site, presentation, and extent of this painless swelling. The option of lipoma was also considered because of duration, history of recurring cheek biting, and uniformity of the swelling. The differential diagnoses of PA include buccal abscess, dermoid cyst, sebaceous cyst, neurofibromas, lipomas, and mucoepidermoid carcinomas.4
In our case, the lesion was encapsulated, and located between the cheek mucosa and the buccinator muscle, which was highly suggestive of a benign tumor of minor salivary gland origin. Radiotherapy is not indicated due to the radio-resistant nature of the tumor. Incomplete resection or tumor spillage during excision can lead to local recurrence. In a few cases, the PA of minor salivary glands may undergo malignant transformation into carcinoma. Recurrence after many years of surgical excision as well as malignant transformation, is a real challenge; hence, long-term follow-up of up to 10 years is necessary.5
In conclusion, this case highlights the need to keep this entity in the differential diagnosis of intra-oral indolent swellings of some duration.
PATIENT’S CONSENT:
The patient provided both oral and written consent for the information congregation and publication of his case report.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTIONS:
SU, SA: Conception and design, data acquisition and analysis, interpretation of work.
SU, SA, SI: Drafting the work or revising it critically for important intellectual content.
SI, AA: Final approval of the version to be published.
SU, SA, SI, AA: Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
REFERENCES
- Verma P, Sachdeva SK, Verma KG, Sachdeva K. Pleomorphic adenoma of cheek: A rare case report and review of literature. Indian J Dent Res 2014; 25(1):122-4. doi: 10.4103/0970-9290.131166.
- Mortazavi H, Alirezaei S, Azari-Marhabi S, Baharvand M, Eshghpour M. Upper lip pleomorphic adenoma: Comparison of reported cases between 1990 and 2012. J Dent Mater Tech 2013; 2(4):125-9.
- Bajia SM, Srivastava T, Viswanatha B, Jayaram RT, Vijayashree MS, Srinivasan SB. Pleomorphic adenoma of the palate: Presentations and management. Res Otolaryngol 2016; 5(1):16-9.
- Aggarwal A, Singh R, Sheikh S, Pallagatti S, Singla I. Pleomorphic adenoma of minor salivary gland: A case report. RSBO 2012; 9:97-101.
- Waldron CA, El-Mofty SK, Gnepp DR: Tumors of the intraoral minor salivary glands: A demographic and histologic study of 426 cases. Oral Surg Oral Med Oral Pathol 1988; 66:323-33. doi:10.1016/0030-4220(88)90240-X.