Osteoid Osteoma of Retromolar Trigone: Report of a Rare Case
By Faheem Ahmed1, Hamza Hassan Mirza1, Zahoor Ahmed Rana1, Noaman Ghauri2Affiliations
doi: 10.29271/jcpsp.2022.08.S162ABSTRACT
Osteoid osteoma is a rare benign bone lesion that is often confused with the osteoblastoma. The osteoid osteoma comprises of 3% of all the primary bone tumours usually found in the long bones and vertebrae with the facial skeleton being the most infrequent site. The lesion usually presents with the swelling and pain that resolves with non-steroidal anti-inflammatory drugs (NSAIDs). Here, we report a case of osteoid osteoma of retromolar trigone, the site which has not been reported in the literature, in a 50-year male patient with a complaint of hard swelling on retromolar trigone associated with the mild intermittent localised pain that aggravated at night and on mastication. Excision of the lesion was carried out with chisel and mallet under local anesthesia with uneventful recovery and no recurrence at the 6 months follow-up.
Key Words: Benign, Osteoid osteoma, Retromolar trigone.
INTRODUCTION
Osteoid osteoma is a rare benign bone lesion that is often confused with the osteoblastoma.
Osteoid osteoma comprises of 3% of all primary bone tumours and is usually found in the long bones and vertebrae with the facial skeleton being the most infrequent site with an incidence of less than 1% in the jaw bones.1 It was first described in 1935 by Jaffe as a separate entity.2 The lesion usually presents with the swelling and pain that usually resolves with non-steroidal anti-inflammatory drugs (NSAIDs). The etiology of osteoid osteoma remains debated to date. Jaffe characterised osteoid osteoma as a benign neoplasm,2 while others suggest the lesion to be inflammatory in origin arising as a result of unusual reparative and healing process.3 Some authors suggest the role of trauma in pathogenesis as well.4
No reported case of osteoid osteoma in jaws is the testament of rarity of this disease in this location. We report a case of osteoid osteoma of retromolar trigone, the site which has never been reported.
CASE REPORT
A 50-year male patient presented in the Oral and Maxillofacial Surgery Department with the complaint of swelling and pain at the right posterior side of the lower jaw for 2 years. The patient also had a complaint of interference in mastication because of swelling. Swelling had gradually increased in size and not regressed since. Pain was mild, intermittent, localised, more aggravated at night and on mastication, and relieved by taking ibuprofen. The medical and family history was non-contributory.
 Figure 1: Clinical presentation of the lesion.
Figure 1: Clinical presentation of the lesion.
The extra-oral and neck examination was non-significant. Intra-orally, an irregularly flattened, tender, and bony hard swellings at the right retromolar trigone were noted extending from the distal of the last erupted molar to just reaching the anterior border of the ramus. It measured 1.5 cm in antero-posterior dimension, 1 cm supero-inferiorly, and hindering the upper molars on closing the jaw. Overlying mucosa was attached to it and was of normal color and temperature (Figure 1). An orthopantomogram (OPG) revealed a well-defined crescent shaped radiolucency with corticated radiopaque borders (Figure 2). Excision of the lesion was planned under local anesthesia. After the administration of lingual and inferior alveolar nerve block and buccal infiltration, the bony hard lesion was excised with a chisel and mallet with adequate jaw support, and the specimen was sent for histopathology. Uneventful recovery was noted with no weakness of lingual nerve. The lesion has not recurred uptill the last follow-up at 6 months post-operatively (Figure 3).
The histopathological examination of the lesion revealed irregular anastomosing trabeculae of the mature lamellar bone containing osteocytes and abundant marrow spaces. Fibrocellular stroma with dilated vascular channels was also seen thus, confirming diagnosis of the osteoid osteoma (Figure 4).
 Figure 2: Crescent-shaped radiolucency along right retromolar trigone.
Figure 2: Crescent-shaped radiolucency along right retromolar trigone.
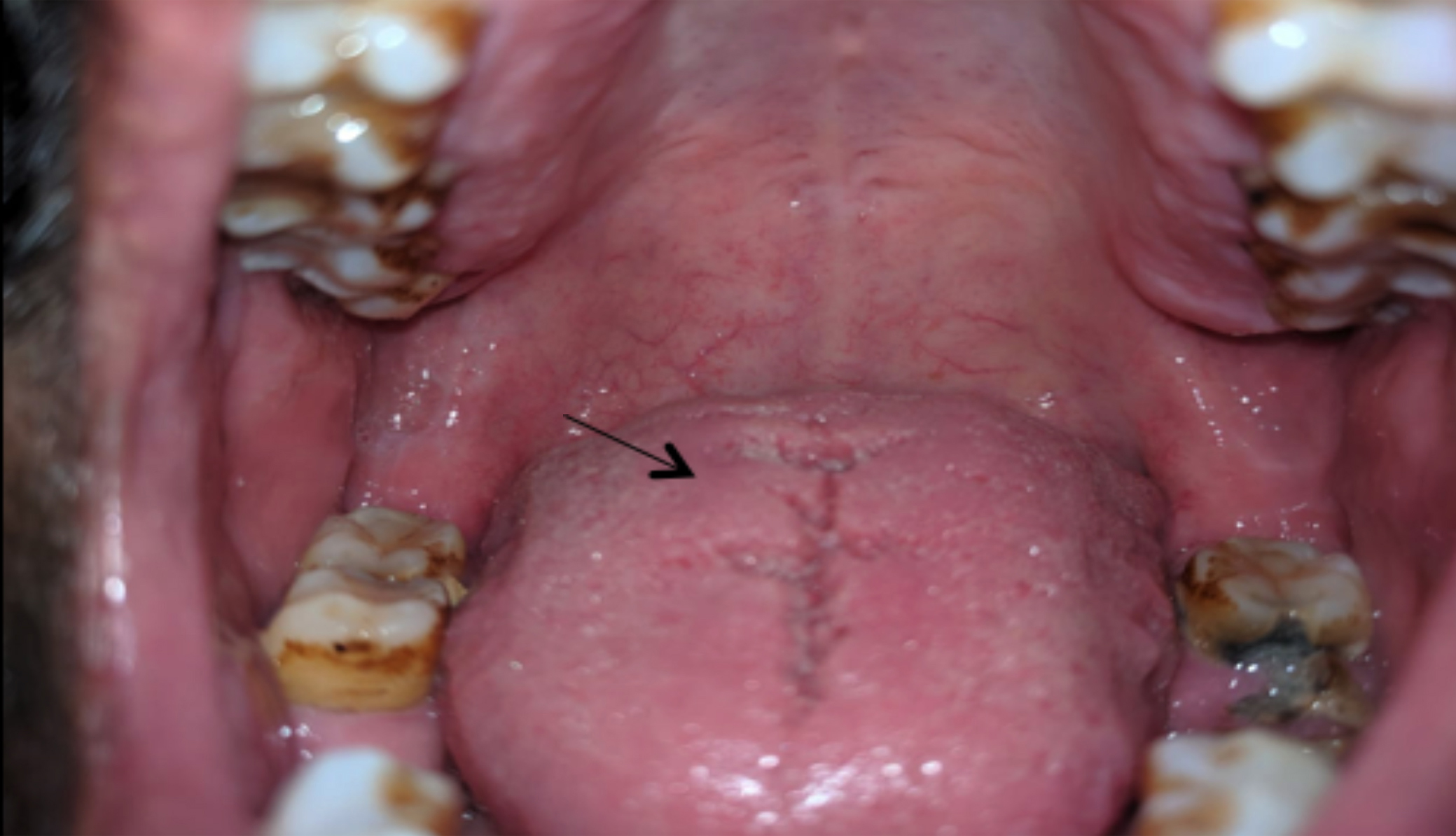 Figure 3: Postoperative view at the 6 months follow-up visit.
Figure 3: Postoperative view at the 6 months follow-up visit.
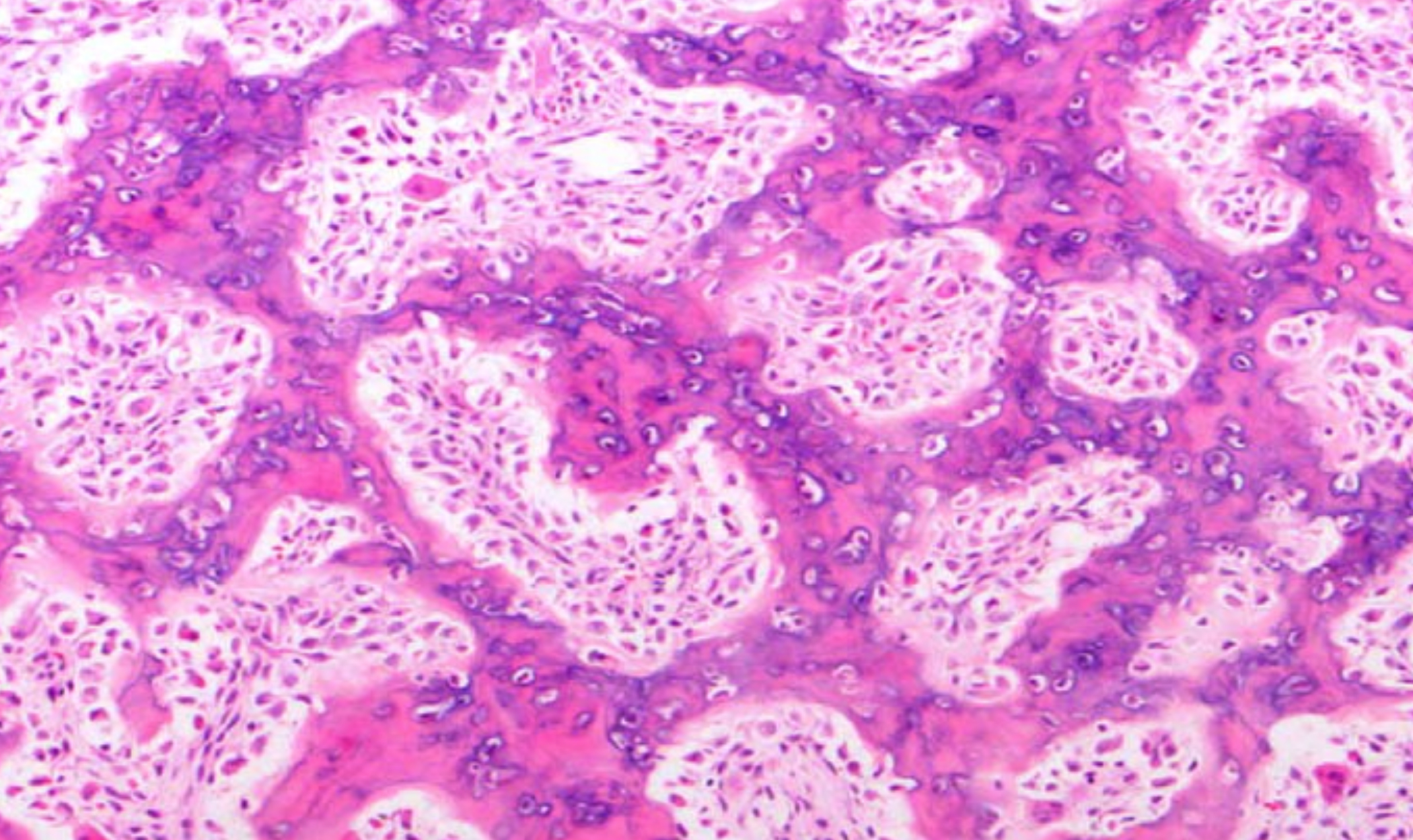 Figure 4: Histology showing irregularly anastomosing trabeculae of mature lamellar bone and marrow spaces.
Figure 4: Histology showing irregularly anastomosing trabeculae of mature lamellar bone and marrow spaces.
DISCUSSION
Osteoid osteoma accounts for 3% of all primary bone tumours and about of 10% all benign tumours.
About 80% of the cases are reported in the long bones.5 Less than 1% are reported in the jaws. There is a slight mandibular and male predilection in jaws. It is usually reported in the second and third decade of life, but the cases have also been reported in the older age.6,7
The most common presenting complaint is swelling along with nocturnal pain. The pain is usually intermittent and responsive to NSAIDs.8
Osteoid osteoma has two appearances on radiology, the osteoid osteoma proper (nidus) that may appear as radiolucent and mixed radiolucent-radiopaque, or radiopaque lesion depending upon the extent of ossification and reaction in its surrounding extended for a variable distance from the nidus.9 The patient, in this case, had intermittent pain relieved with NSAIDs and his OPG revealed a crescent-shaped radiolucency with corticated borders in the right retromolar trigone area. The differential diagnosis of the osteoid osteoma includes osteoblastoma, complex odontoma, osteosarcoma, and Garre’s osteomyelitis. Definitive diagnosis is always by the histopathological examination.
The two treatment options are surgical and non-surgical. The non-surgical option includes symptomatic treatment with NSAIDs which is reserved for smaller lesions that do not interfere with the function. Complete excision is the treatment of choice. Surgical options for gnathic lesions are usually local excision or curettage.10 The osteoid osteoma presented in this case report was causing pain and interference with the mastication; therefore, it was deemed suitable for the surgical excision.
In conclusion, osteoid osteoma is a rare benign bone lesion presenting as less than 1% of all the jaw tumour, etiology of which is still controversial. Pain is the characteristic feature that responds to NSAIDs. The mainstay of the treatment is surgical excision.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
FA: Contribution to the conception, design of work, and drafting of the case report.
HHM: Revising and collecting the data for important intellectual content.
ZAR: Final approval of the version to be published and conventions were made.
NG: Correction of references and plagiarism check.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Richardson S, Khandeparker RV, Sharma K. A large osteoid osteoma of the mandibular condyle causing conductive hearing loss: A case report and review of literature. J Korean Assoc Oral Maxillofac Surg 2017; 43(2):106-14. doi: 10.5125/jkaoms.2017.43.2.106.
- Matthies L, Rolvien T, Pakusa TJ, Knipfer C, Gosau M, Amling M, et al. Osteoid osteoma of the mandible–clinical and histological findings. Anticancer Res 2019; 39(1): 291-6. doi: 10.21873/anticanres.13110.
- Deferm J, Steens S, Vriens D, Bekers E, Kalaykova S, Borstlap W. Chronic temporomandibular joint pain: Two cases of osteoid osteoma and a review of the literature. Int J Oral Maxillofac Surg 2017; 46(9):1130-7. doi: 10.1016/j. ijom.2017.03.036.
- Issa SA, Abdulnabi HA, Alshewered ASH. Intra-articular osteoid osteoma of tempromandibular joint: A case report. Int J Surg Case Rep 2019; 62:9-13. doi: 10.1016/j.ijscr. 2019.07.070.
- Maehara T, Murakami Y, Kawano S, Mikami Y, Kiyoshima T, Chikui T, et al. Osteoid osteoma of mandibular bone: Case report and review of the literature. J Oral Maxillofac Surg Med Pathol 2019; 31(5):322-6.
- Diaz-Rengifo IA, Diaz-Caballero AJ, Redondo-De Oro K, Hernandez-Arenas YY. Painless osteoid osteoma in the maxilla of an elderly female patient. J Oral Maxillofac Pathol 2019; 23(2):280. doi: 10.4103/jomfp.JOMFP_295_18.
- Khaitan T, Ramaswamy P, Ginjupally U, Kabiraj A. A bizarre presentation of osteoid osteoma of maxilla. Iranian J Pathol 2016; 11(5):431-4.
- Adouly T, Oubahmane T, Adnane C, Rouadi S, Abada R, Roubal M, et al. Bilateral osteoid osteoma of the mandible: An unusual case report. Int J Pediatric Otorhinolaryngol Extra 2015; 10(3):56-8.
- Devathambi TJR, Ambrose WC, Niazi KZTM, Raja S. Osteoid osteoma in anterior border of ramus of mandible: A rare entity. J India Academy Oral Med Radiol 2016; 28(4):449.
- Rathod SV. Subperiosteal osteoid osteoma: A rare entity. J Contemporary Dentistry 2015; 5(2):118-21.