Neuroendocrine Tumour of the Gallbladder Diagnosed after Cholecystectomy
By Halil Ibrahim Tasci1, Esra Zeynep Coskunoglu2, Emin Turk1, Erdal Karagulle1Affiliations
doi: 10.29271/jcpsp.2022.08.S127ABSTRACT
Gallbladder cancer is a rare but aggressive malignancy. Neuroendocrine tumour of the gallbladder make up 2-3% of all the gallbladder tumour.
A 67-year female patient underwent laparoscopic cholecystectomy because of symptomatic cholelithiasis and the histopathology revealed a neuroendocrine tumour of the gallbladder, stage pT2a. The patient’s imaging study for metastasis workup were normal. A radical cholecystectomy procedure was planned as the tumour stage was pT2a. Postoperative chemotherapy and/or radiotherapy were recommended. The patient, who had comorbidities, was refused both surgery and other treatment alternatives. The patient’s one-year clinical, laboratory, and radiological follow-up did not reveal any findings of recurrence or metastasis.
There is no standardised staging system for neuroendocrine tumours of the gallbladder since the number of such cases is quite limited. Guidelines are also insufficient. Multi-centred and large studies are needed in order to develop standardisation in treatment, prognosis, and factors affecting survival.
Key Words: Cholecystectomy, Neuroendocrine Tumour, Gallbladder.
INTRODUCTION
Gallbladder cancer is a rare, but aggressive malignancy (most are made up of adenocarcinomas). Neuroendocrine tumours (NETs) of the gallbladder merely constitute 2-3% of all the gallbladder tumours.1 Only 0.5% of NETs originating from the gastroenteropancreatic system arise from the gallbladder.2
The aim of this study was to present a case of the patient who underwent laparoscopic cholecystectomy because of symptomatic cholelithiasis, and was diagnosed with NET of the gallbladder following pathology analysis along with the literature review.
CASE REPORT
A 67-year female patient presented to our clinic with the complaints of colicky pain in the epigastria and right subcostal areas with accompanying nausea and vomiting for the last three years. The patient’s medical history revealed that she had Hashimoto’s thyroiditis, mitral valve replacement, and cardiac arrhythmia.
Further, during the premenopausal period, the patient underwent total abdominal hysterectomy and bilateral salpingo-oophorectomy for dysfunctional uterine bleeding that could not be controlled with the medical treatment. The patient had tenderness in the right subcostal and epigastric areas as revealed by her physical examination. The upper abdominal ultrasonography showed findings consistent with the chronic calculous cholecystitis. Surgery was planned for the patient. After completing her preoperative preparations, laparoscopic cholecystectomy was performed. No tumour findings were found during the surgery. The patient was discharged on the first postoperative day with the recommendations and without any problems.
The macroscopic evaluation of the specimen revealed an 8 mm greyish mural nodule involving the fundus. The specimen was sampled thoroughly for precise evaluation of anatomic extent and focality. The cystic duct margin and a regional lymph node on the neck were also sampled. The microscopy showed a neoplastic lesion infiltrating the gallbladder wall in full thickness and invading into the perimuscular connective tissue on the serosal-side (Figure 1). The tumour was composed of the small cells arranged in nests and sheets. The neoplastic cells had round to oval nuclei and coarsely stippled chromatin (Figure 2). Upto 12 mitotic figures were detected per 10 HPF at 40× magnification and an ocular field diameter of 0.5 mm. No necrosis was detected. On immunohistochemistry, the neoplastic cells were strongly and diffusely positive for Synaptophysin and Chromogranin A (Figure 3). The tumour cells showed focal positivity for Cytokeratin 7, whereas Cytokeratin 20, TTF-1, and CDX2 were negative. The Ki67 index was slightly above 20% (Figure 4). In the view of the histomorphological and immunohistochemical findings, the tumour was signed out as NET, Grade 3. The cystic duct margin and the sampled lymph node were tumour free.
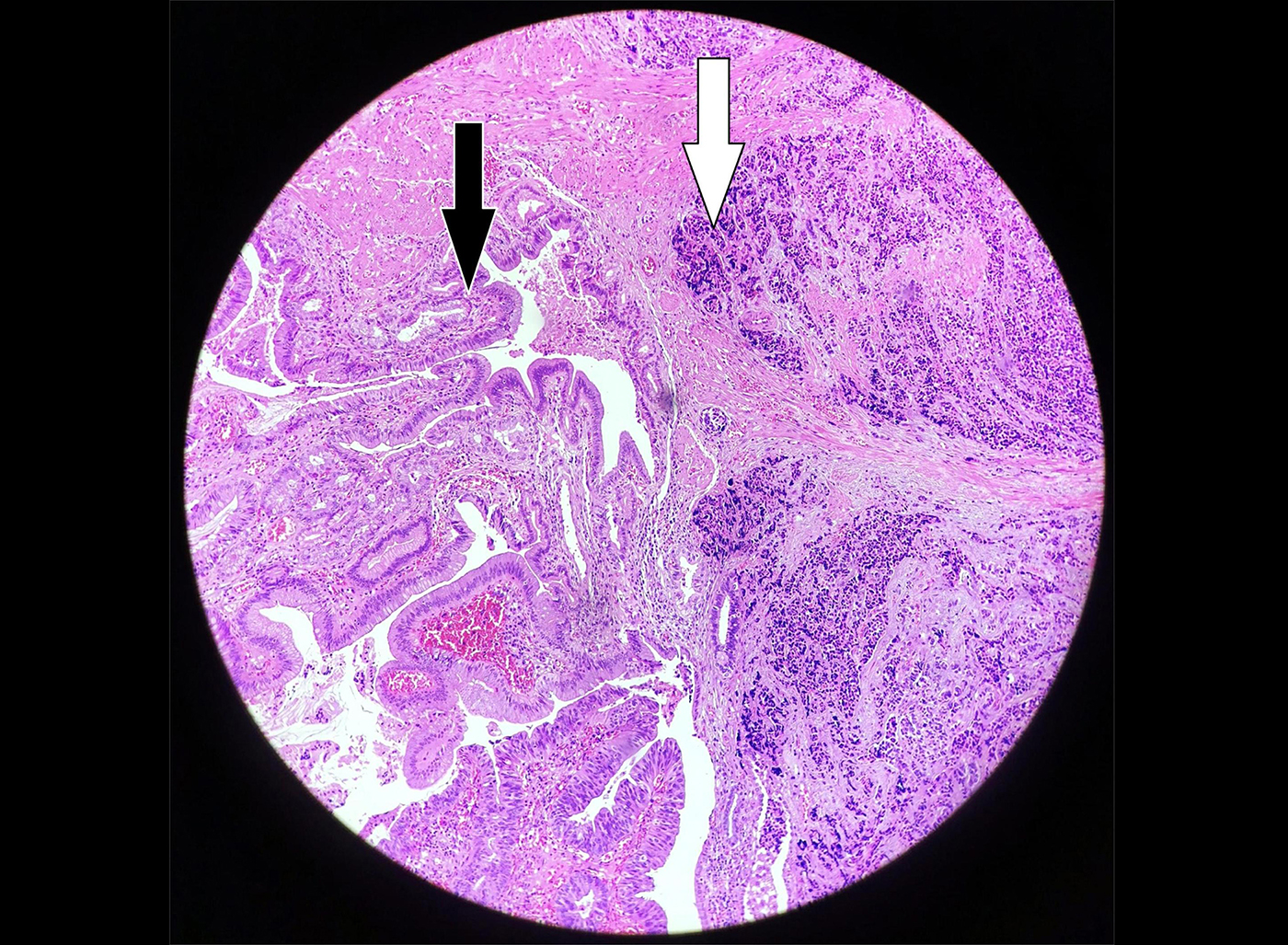 Figure 1: Tumour infiltration in the gallbladder wall, neighboring benign glandular structures (black arrow), showing extensive crush artifact in the form of layers with an infiltration pattern (white arrow) (H&E, ×10).
Figure 1: Tumour infiltration in the gallbladder wall, neighboring benign glandular structures (black arrow), showing extensive crush artifact in the form of layers with an infiltration pattern (white arrow) (H&E, ×10).
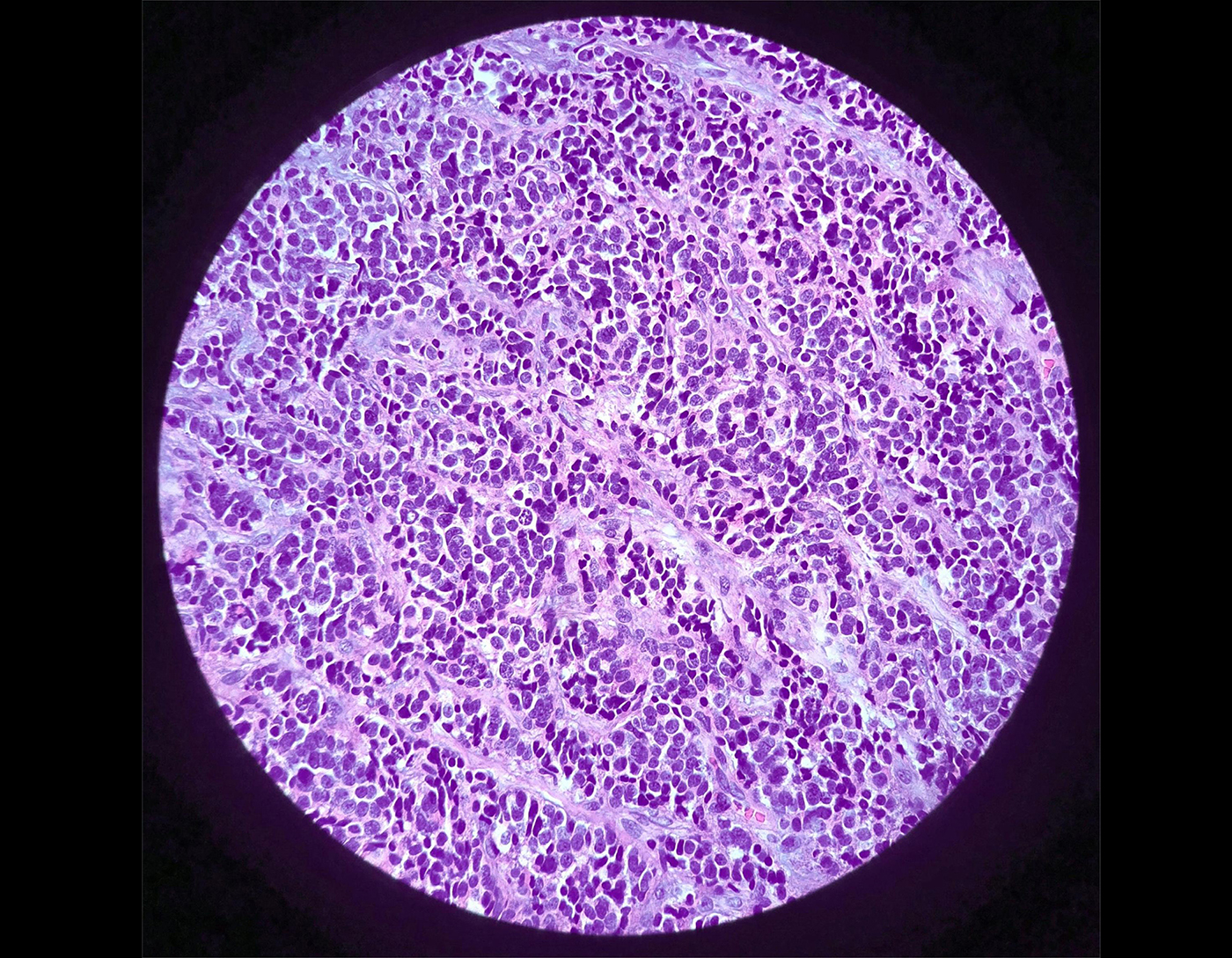 Figure 2: Small round tumour cells with indiscernible borders having hyperchromatic or salt-pepper chromatin containing nuclei (H&E, ×40).
Figure 2: Small round tumour cells with indiscernible borders having hyperchromatic or salt-pepper chromatin containing nuclei (H&E, ×40).
Thoracic-abdominal computed tomography and gadolinium-enhanced PET/CT scan for metastasis workup were performed following pathology results. No other foci or tumours were identified. The patient was evaluated at the board meeting and radical cholecystectomy procedure was planned since the tumour stage was pT2a. Subsequent postoperative chemotherapy and/or radiotherapy were also recommended. The patient, who had co-morbidities, refused both the secondary surgery and chemo-radiotherapy treatments. The patient’s three-month, six-month, and one-year follow-up did not reveal any recurrent disease.
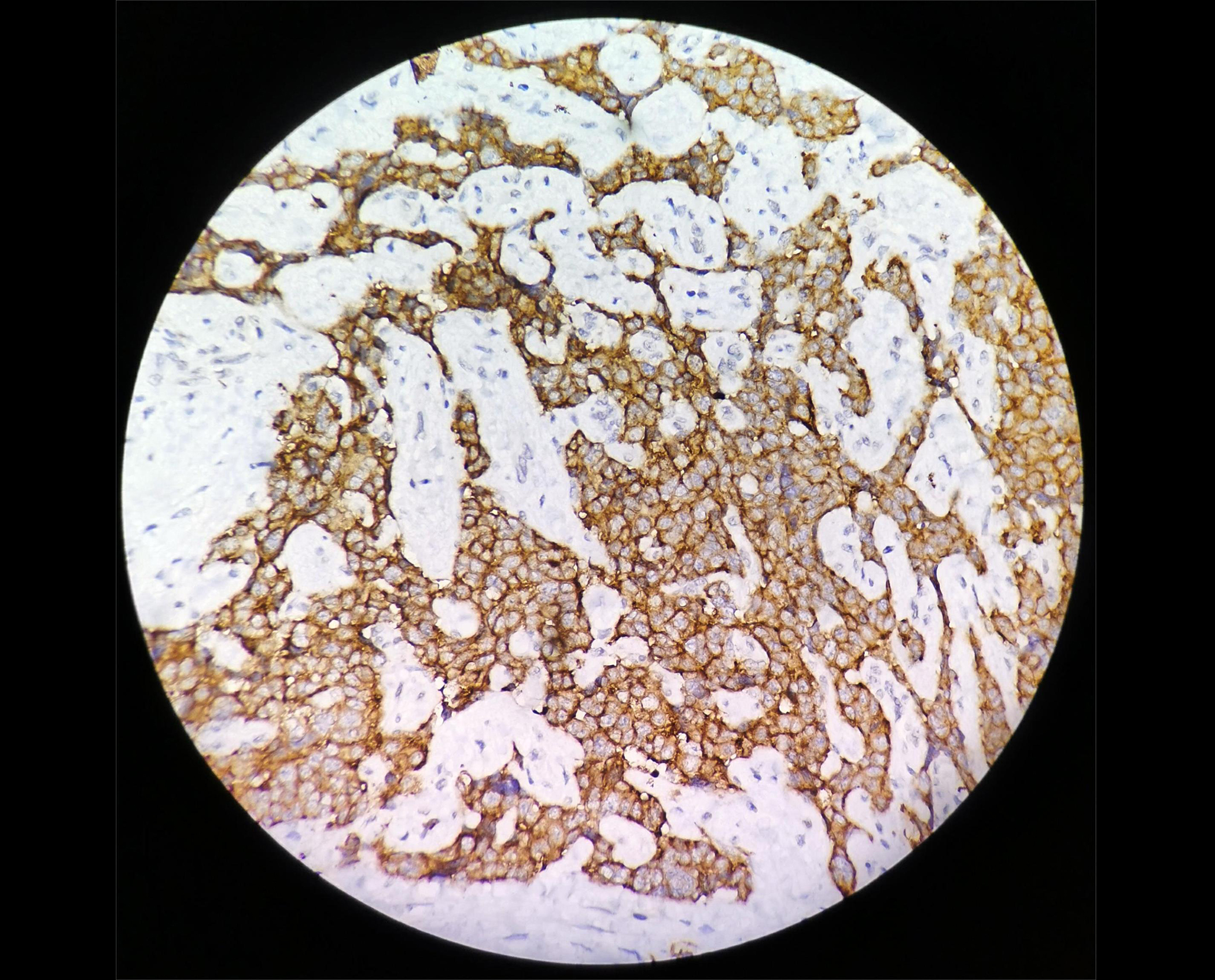 Figure 3: Immunohistochemical staining which shows extensive chromogranin positivity in the tumour.
Figure 3: Immunohistochemical staining which shows extensive chromogranin positivity in the tumour.
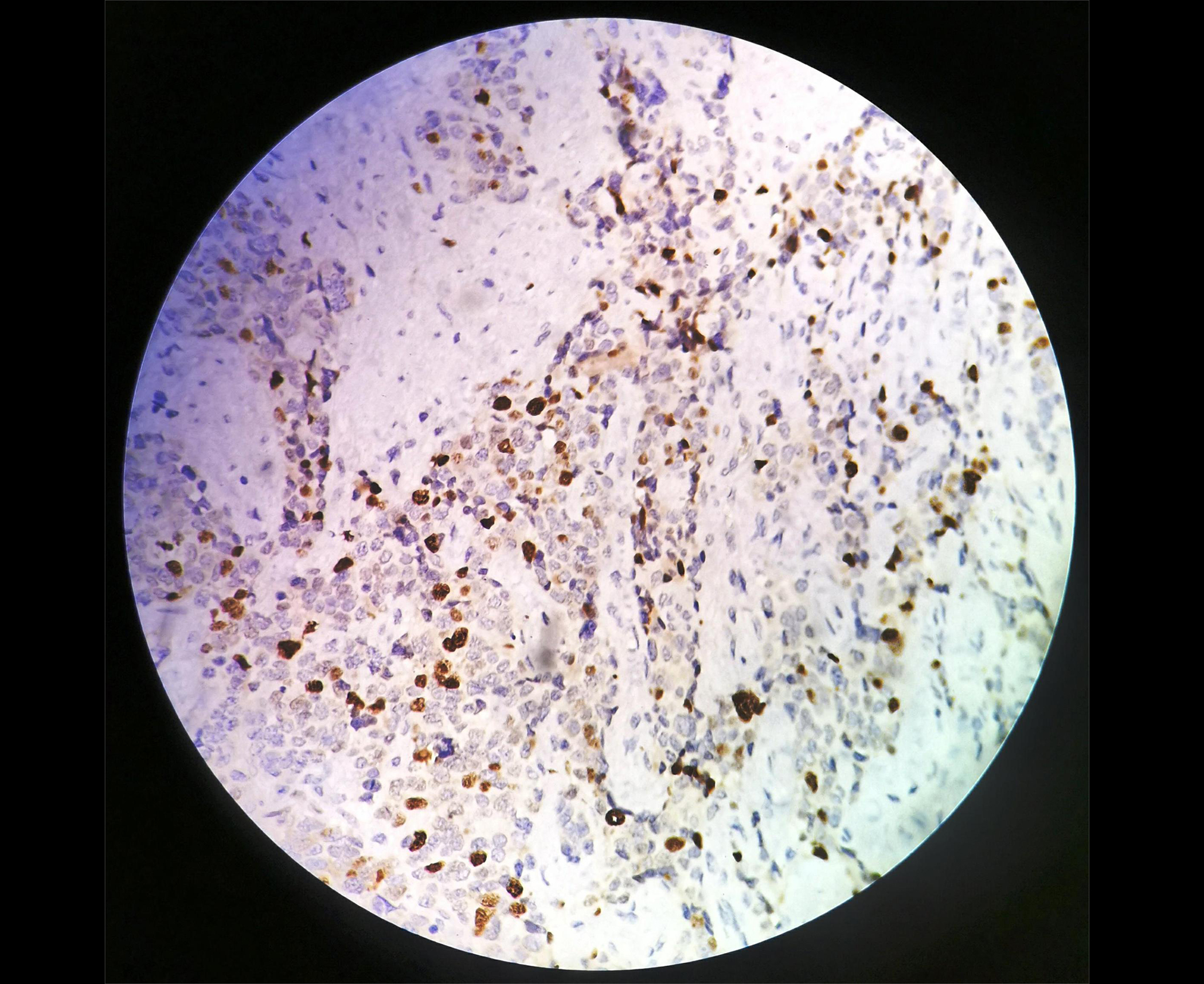 Figure 4: The proliferation index of the tumour revealed by immunohistochemical marker, Ki-67 staining.
Figure 4: The proliferation index of the tumour revealed by immunohistochemical marker, Ki-67 staining.
DISCUSSION
NET is a common term used to describe neoplasms that arise from the neural and endocrine structures anywhere in the body.3,4 Neuroendocrine carcinomas of the gallbladder, which were first described by Joel in 1929, are quite rare and a mere 0.04-0.5% of all the NETs originate from the gallbladder.4 Only 2% of gallbladder cancers are NETs.3 Since there are no neuroectodermal cells in the gallbladder, it has been suggested that the NETs of the gallbladder arise from pluripotent stem cells or metaplastic changes on the gallbladder wall are related to the chronic irritation of gallbladder stones.4 This patient, too, had gallbladder stones that might have set the basis for the NET.
While the disease has a higher incidence in the elderly and female patients, it is often seen in the 35-80 years age range.5 Patients usually present with the non-specific complaints. Hepatitis and weight loss are rare presenting features in the advanced stages.6 The studies in the literature have shown that most of the NETs of the gallbladder are non-functional.5 Thus, findings related to carcinoid syndrome are rarely seen in NETs of the gallbladder.7 In the present case, the patient had no specific finding other than chronic calculous cholecystitis.
It is virtually impossible to diagnose a patient through a radiological imaging method like ultrasonography, computed tomography, magnetic resonance imaging, or positron emission tomography in the preoperative period with NET of the gallbladder.4 Most patients are diagnosed by the histopathological analyses of their specimen following cholecystectomy procedures performed for the gallbladder stones.6 This patient, too, was diagnosed following the results of the histopathological analysis conducted following cholecystectomy.
The treatment guidelines offer staging criteria and therapy algorithms for the NETs of many organs like the stomach, ampulla of vater, small bowel, large bowel, appendix, and pancreas. There is no standardised staging system or recommended treatment algorithm for the NETs of the gallbladder because they are rarely seen.1 Most of the studies, therefore, have utilised treatment and staging systems recommended for the adenocarcinomas of the gallbladder and prognosis of NETs of the gallbladder.1 We also used the guidelines for adenocarcinomas of the gallbladder for the treatment of this patient.
The treatment strategies mentioned in the literature vary greatly. Treatment and surgical methods ranging from only cholecystectomy to radical resection accompanied by systemic chemotherapy and radiotherapy combinations have been used.1 It has generally been agreed that cholecystectomy is sufficient in T1 tumours with no requirement for hepatic resection. Liver resection with negative margins is only recommended in the event of tumour invasion into the parenchyma of the liver.8
While there is no standardised systemic chemotherapy regime for the NETs of the gallbladder, drugs used for the adenocarcinomas of the biliary system and other NETs of the gastrointestinal system are used in the treatment.9 In this case, the patient was recommended to have a secondary procedure and subsequent adjuvant chemo-radiotherapy since the tumour was evaluated to be pT2a, but the patient refused any other surgery or treatment.
It has been demonstrated that old age, large cell histology, and positive surgical margins are associated with the poor survival.1 While the survival rates in NETs of the gallbladder are higher than that of adenocarcinomas of the gallbladder, these are lower than those of NETs of the gastrointestinal system arising from other organs.1
NET of the gallbladder is a rare but aggressive malignancy. There is no standardised staging system for the NETs of the gallbladder since the number of such cases is quite limited. Guidelines are also insufficient. Multi-centered larger studies are needed in order to achieve standardisation in treatment, prognosis, and factors affecting survival.
PATIENT’S CONSENT:
Informed consent is obtained from the patient
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
HIT: Concept, data collection and interpretation, literature search, and manuscript writing.
EZC: Concept, data collection and interpretation, and manuscript writing.
ET, EK: Concept, design, definition, and intellectual content.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Ayabe RI, Wach M, Ruff S, Martin S, Diggs L, Wiemken T, et al. Primary gallbladder neuroendocrine tumour: Insights into a rare histology using a large national database. Ann Surg Oncol 2019; 26(11):3577-85. doi: 10.1245/s10434- 019-07440-6.
- Cen D, Liu H, Wan Z, Lin Z, Wang Y, Xu J, Liang Y. Clinicopathological features and survival for gallbladder NEN: A population-based study. Endocr Connect 2019; 8(9):1273-81. doi: 10.1530/EC-19-0124.
- Hirose Y, Sakata J, Endo K, Takahashi M, Saito R, Imano H, et al. A 0.8-cm clear cell neuroendocrine tumour G1 of the gallbladder with lymph node metastasis: A case report. World J Surg Oncol 2018; 16(1):150. doi: 10.1186/s12957- 018-1454-y.
- Kumar K, Tariq H, Ahmed R, Chukwunonso C, Niazi M, Ihimoyan A. Small-cell type, poorly differentiated neuro-endocrine carcinoma of the gallbladder: A case report and review of the literature. Case Rep Oncol Med 2019; 2019:8968034. doi: 10.1155/2019/8968034.
- Hussain I, Sarvepalli D, Zafar H, Jehanzeb S, Ullah W. Neuroendocrine tumour: A rare, aggressive tumour of the gallbladder. Cureus 2019; 11(9):e5571. doi: 10.7759/ cureus.5571.
- Moris D, Tsilimigras DI, Lim J, Camastra D, Nanavati A, Knechtle SJ, et al. Neuroendocrine carcinomas of the gallbladder: Lessons learnt from cases at opposite ends of the spectrum. J BUON 2018; 23(6):1922-6.
- Liu W, Chen W, Chen J, Hong T, Li B, Qu Q, et al. Neuroendocrine carcinoma of gallbladder: A case series and literature review. Eur J Med Res 2019; 24(1):8. doi: 10.1186/s40001-019-0363-z.
- Gundes E, Kucukkartallar T, Cakir M, Gemici K, Esen HH. Incidental neuroendocrine carcinoma of the gallbladder. Eur J Gen Med 2014; 11(4):272-4.
- Kanetkar AV, Patkar S, Khobragade KH, Ostwal V, Ramaswamy A, Goel M. Neuroendocrine carcinoma of gallbladder: A step beyond palliative therapy, experience of 25 cases. J Gastrointest Cancer 2019; 50(2):298-303. doi: 10.1007/s12029-018-0070-y.