Melena: An Unusual Manifestation of Metastatic Lung Cancer
By Muge Ustaoglu1, Bahiddin Yilmaz2, Sultan Caliskan3, Ceren Canturk4, Ibrahim Goren1, Ahmet Bektas1Affiliations
doi: 10.29271/jcpsp.2022.04.61ABSTRACT
Lung cancer is the most common cancer around the world, and the leading cause of cancer-related deaths. Clinical manifestations of lung cancer may vary from non-specific respiratory symptoms to symptoms due to metastases. The most common sites of metastases are the lymph nodes, liver, adrenals, bone, and brain. Metastasis of lung cancer to stomach is very rare. Here, we present a case of squamous cell lung cancer in a 71-year male metastasing to the stomach, a very uncommon site of metastasis.
Key Words: Lung cancer, Melena, Metastasis, Stomach.
INTRODUCTION
Lung cancer is considered the most common cause of cancer-related deaths around the world.1 Non-small cell lung cancer (NSCLC) accounts for about 85% of lung cancers. The most common presenting signs and symptoms are chest pain, cough, dyspnea, and hemoptysis.2 Sometimes, patients have symptoms due to metastatic disease. Gastric metastasis is infrequent.3 In this case, we describe a case of a 71-year male presenting with melena due to gastric metastasis from a squamous cell carcinoma (SCC) of the lung. As far as we know, this is the 12th case reported in English literature.
CASE REPORT
A 71-year man visited our Emergency Department with complaints of melena. He was smoking for 30 years and had a smoking history of 50 packs/year. The patient was diagnosed with stage T2N3M0 SCC of the lung 15 months ago; and had received both chemotherapy (paclitaxel, carboplatin) and radiotherapy. He had a history of malaise, anorexia, and anemia for six months. PET/CT scan with [18F]-fluorodeoxyglucose (FDG) showed stable disease.
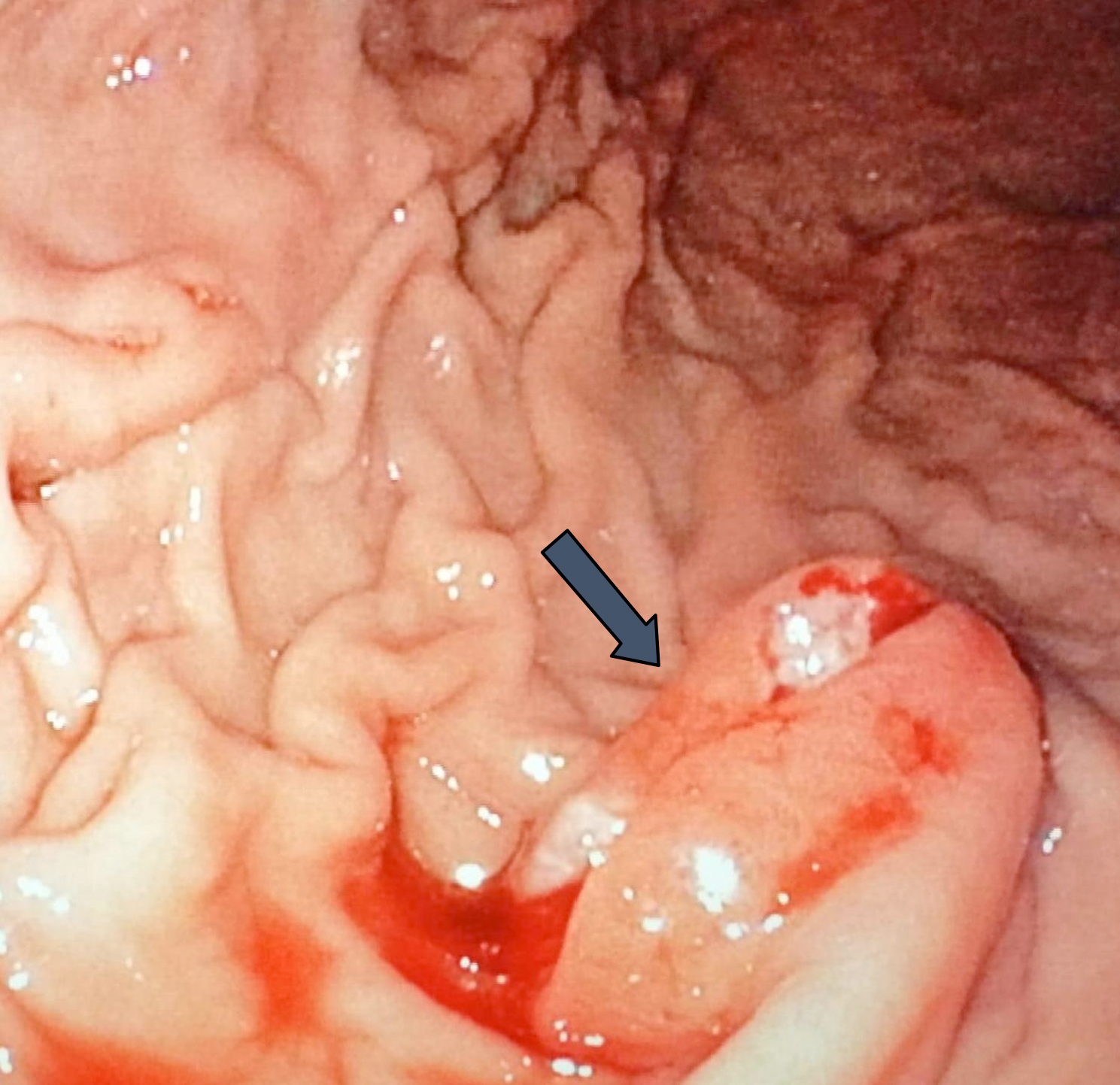 Figure 1: Endoscopic image of an ulcerated, friable mass in the gastric corpus (arrow).
Figure 1: Endoscopic image of an ulcerated, friable mass in the gastric corpus (arrow).
Cranial radiotherapy was planned because of brain metastasis two weeks before admission. He reported a 10-day history of melena. On physical examination, he was fully conscious, with a normal heart rhythm. The abdomen was soft and lax and digital rectal examination showed melena. On laboratory workup, hemoglobin was 10 g/dL, platelet count was 193000/mm,3 and international normalised ratio (INR) was 1.1. Esophagogastroduodenoscopy was performed and an approximately 1.2 cm diameter ulcerated polypoid lesion was seen in the stomach towards the greater curvature; and the biopsies were taken (Figure 1). Histopathological examination of the endoscopic biopsies revealed the infiltration of malignant cells between gastric glands. The malignant cells, arranged in solid nests, were characterised by large vesicular nuclei with irregular shape and size, prominent nucleoli, and abundant eosinophilic cytoplasm. Immunohistochemically, the neoplastic cells were p40 positive, cytokeratin 7, and TTF-1 negative. The pathological findings supported a diagnosis of gastric metastasis of SCC of the lung (Figure 2). A combination of cisplatin and gemcitabine chemotherapy was started due to advanced and metastatic disease. After the first cycle of chemotherapy, no more chemotherapy was administered because of his poor performance status. Supportive treatment was given to improve the quality of life.
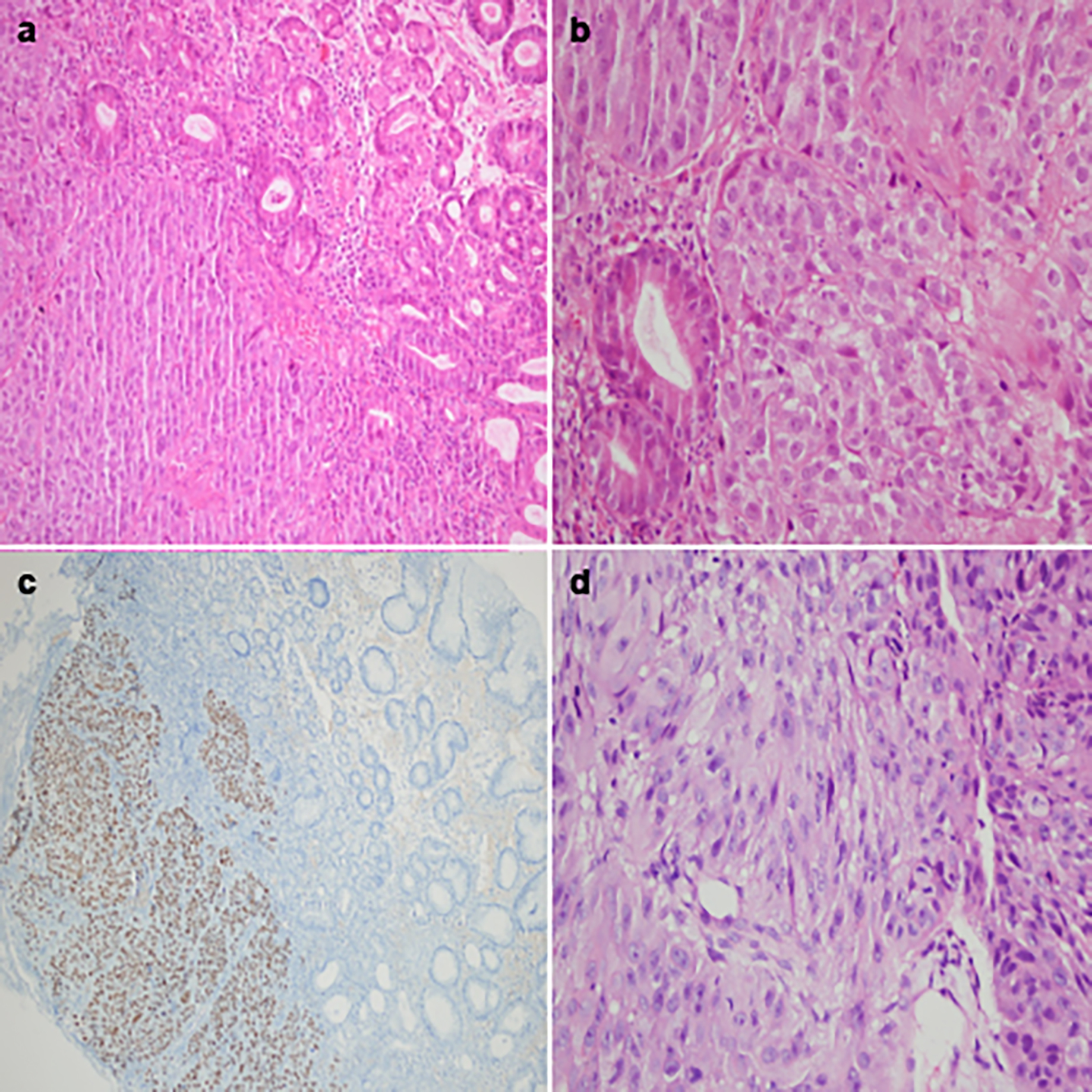 Figure 2: Microscopic findings. (a) Squamous cell carcinoma infiltration in the gastric mucosa (H&E, ×40). (b) Tumor cells are arranged as solid nests next to gastric glands with large nucleoli, vesicular nuclei and abundant eosinophilic cytoplasm (H&E, ×400). (c) Diffuse nuclear staining of tumor cells with p40 immunohistochemistry. (d) Squamous cell carcinoma in the patient’s previous bronchial mucosal biopsy.
Figure 2: Microscopic findings. (a) Squamous cell carcinoma infiltration in the gastric mucosa (H&E, ×40). (b) Tumor cells are arranged as solid nests next to gastric glands with large nucleoli, vesicular nuclei and abundant eosinophilic cytoplasm (H&E, ×400). (c) Diffuse nuclear staining of tumor cells with p40 immunohistochemistry. (d) Squamous cell carcinoma in the patient’s previous bronchial mucosal biopsy.
DISCUSSION
Lung cancer is the leading cause of cancer-related deaths among both genders in the world.1 The most common sites of metastasis are lymph nodes, liver, adrenals, bone, and brain. More rarely, metastasis may occur in the gastrointestinal tract, especially the stomach.4
The incidence of gastric metastasis of lung cancer is higher in the autopsy series (0.7-1.2%).5,6 Gastric metastasis especially occurs in male smokers and SCC is the most common histopathological type.3,7 The most common symptoms of gastric metastasis are epigastric pain, anemia, nausea, vomiting, hematemesis, and melena.8 Diagnosis of gastric metastasis is generally made by upper gastrointestinal endoscopy and biopsy, and histopathological and immunohistochemical examination.
Clinical signs, including laboratory tests that raise suspicion of metastatic disease, are suggested in a meta-analysis. According to this meta-analysis, metastasis should be suspected when hematocrit is under 40 in male patients.9 In our patient, at the time of diagnosis of lung cancer, hematocrit was 35%. There were no tumor nodules in the contralateral lobe, no pleural or pericardial nodules/malignant effusion, no extrathoracic tumor metastases at the time of diagnosis, and six months before Emergency Department admission on PET-CT scan'. When the patient was diagnosed with lung cancer, despite hematocrit being 35%, upper gastrointestinal endoscopy was not performed; thus, potentially delaying the diagnosis.
In conclusion, patients with lung cancer, who have non-specific gastrointestinal symptoms, either at the time of diagnosis or during follow-up, should be evaluated carefully. If necessary, upper gastrointestinal endoscopy should be performed. This may obviate the delay in the diagnosis of metastatic disease.
PATIENT’S CONSENT:
The consent of the patient was taken prior to the writing of the manuscript.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
MU: Writing manuscript, design, concept, material, data collection, literature search, analysis and/or interpretation.
BY: Supervision, critical review.
SC: Material, data collection.
CC: Writing manuscript.
IG: Literature research, supervision.
AB: Critical review.
REFERENCES
- Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics. CA Cancer J Clin 2015; 65(2): 87-108. doi: 10.3322/caac.21262.
- Chute CG, Greenberg ER, Baron J, Korson R, Baker J, Yates J. Presenting conditions of 1539 population-based lung cancer patients by cell type and stage in New Hampshire and Vermont. Cancer 1985; 56(8):2107. doi: 10.1002/ 1097-0142(19851015)56:8<2107::aid-cncr2820 560837>3.0.co;2-t.
- Azar I, Koutroumpakis E, Patel R, Mehdi S. Squamous cell lung carcinoma presenting as melena: A case report and review of the literature. Rare Tumors 2017; 9(3):7164. doi: 10.4081/rt.2017.7164.
- Riihimaki M, Hemminki A, Fallah M, Thomsen H, Sundquist K, Sundquist J, et al. Metastatic sites and survival in lung cancer. Lung Cancer 2014; 86(1):78-84. doi: 10.1016/j. lungcan.2014.07.020.
- McNeill PM, Wagman LD, Neifeld JP: Small bowel metastases from primary carcinoma of the lung. Cancer 1987; 59(8):1486‑9. doi: 10.1002/1097-0142(19870415) 59:8<1486::aid-cncr2820590815>3.0.co;2-w.
- Antler AS, Ough Y, Pitchumoni CS, Davidian M, Thelmo W: Gastrointestinal metastases from malignant tumors of the lung. Cancer 1982; 49(1):170‑2. doi: 10.1002/1097-0142 (19820101)49:1<170::aid-cncr2820490134>3.0.co;2-a.
- Maeda J, Miyake M, Tokita K, Iwahashi N, Nakano T, Tamura S, et al. Small cell lung cancer with extensive cutaneous and gastric metastases. Internal Med 1992; 31(11):1325-8. doi: 10.2169/internalmedicine.31.1325.
- Gao S, Hu XD, Wang SZ, Liu N, Zhao W, Yu QX, et al. Gastric metastasis from small cell lung cancer: A case report. World J Gastroenterol 2015; 21(5):1684-8. doi: 10.3748/wjg.v21.i5.1684.
- Silvestri GA, Littenberg B, Colice GL. The clinical evaluation for detecting metastatic lung cancer. A meta-analysis. Am J Respir Crit Care Med 1995; 152(1):225-30. doi: 10.1164/ ajrccm.152.1.7599828.