Male Urethral Diverticulum with Stones Presenting as Acute Urinary Retention
By Syed Muhammad Nazim, Roshane Shahid Rana, Kaleem Khan MiraniAffiliations
doi: 10.29271/jcpsp.2022.08.S189ABSTRACT
The urethral diverticulum is an outpouching of the urethral wall communicating with its lumen. Acquired male urethral diverticulum is a rare entity and arises secondary to intervention or distal urethral obstruction. Most patients present with lower urinary tract symptoms (LUTS). Development of calculi is seen in 4-10% of cases. We describe a case of a 63-year gentleman who presented with urinary tract infection (UTI) and acute urinary retention (AUR). He denied history of urolithiasis. Per-urethral catheterization failed, so a supra-pubic catheter was placed and UTI was managed with broad-spectrum parenteral antibiotics. On workup, he was found to have a large tubular urethral diverticulum in the anterior urethra with multiple stones and urethral strictures. The case was managed endoscopically with optical urethrotomy and fragmentation and retrieval of stones using a semi-rigid ureteroscope and pneumatic lithoclast.
Key Words: Urethra, Diverticulum, Male, urethral calculus, Lithoclast.
INTRODUCTION
Urethral diverticulum (UD) is an outpouching of the urethral wall continuous with the true urethral lumen and can be of saccular or tubular types.1 Although there are multiple studies in contemporary literature regarding the presentation, diagnosis, and management of UD in females,2 this entity is rare in males and is described in case reports and small case series only. The clinical presentation includes lower urinary tract symptoms (LUTS), particularly post-void dribbling, difficulty in urination, urinary incontinence, and recurrent urinary tract infections (UTIs). Development of calculi is observed in 4-10% of patients.3 Presentation with acute urinary retention (AUR) has only been reported in a few cases. Here, we discuss a case of UD and lithiasis in an adult male which was managed by a minimally invasive surgical approach.
CASE REPORT
A 63-year male with multiple medical co-morbid conditions, i.e., chronic obstructive pulmonary disease (COPD), Hypertension (HTN), and Ischemic heart disease (IHD) presented to the emergency room with one-day history of fever and AUR. He had a prior history of LUTS and uneventful urethral catheterization about 5 years back at the time of coronary artery bypass graft (CABG).
He had history of UTI in past but denied any history of ureteric colic or urolithiasis. On examination, he was tachycardiac and had a temperature of 38.4oC. Urethral meatus, genitalia, and perineum were normal. Digital rectal examination revealed a benign, smooth, non-tender, moderately enlarged prostate; however, the urinary bladder was palpable. Laboratory workup revealed a raised total leukocyte count (TLC) of 17,000/µL with serum creatinine (Cr) of 1.4 mg/dl. Ultrasound showed normal kidneys with a bladder volume of 630 ml and prostatomegaly (33 grams). Per-urethral catheterization failed; so, a supra-pubic catheter was placed. His urine culture grew Klebsiella, which was treated with broad-spectrum antibiotics. He was followed up with antegrade and retrograde urethrogram after 2 weeks which demonstrated calcific densities in the line of the urethra and two small strictures at peno-bulbar and bulbo-membranous junctions. There was a tubular dilatation on the ventral aspect of the bulbar urethra communicating distally with the normal urethra without any contrast extravasation and free flow of contrast to the bladder, raising suspicion of UD (Figure 1).
We performed cysto-uretheroscopy. Intra-operatively, a peno-bulbar stricture was identified and incised; a pit was noticed at the distal bulbar urethra below the main lumen at 7 O’clock position with pouting stones. It was negotiated with 6 Fr semi-rigid ureteroscope and found to be a blind-ending diverticulum with multiple small stones (Figure 2). All stones were fragmented with lithoclast and retrieved. The posterior urethral stricture was dilated and 16 Fr 2-way Foley’s catheter was placed. The patient was started on alpha-blockers.
The post-operative period was uneventful. The patient had a successful trial without a catheter (TWOC) and later had a uro-flowmetry (UFM) after 3 months that showed a good maximum flow (Qmax) of 17.6 ml/sec with minimal post-void residue. He is currently asymptomatic with minimal LUTS.
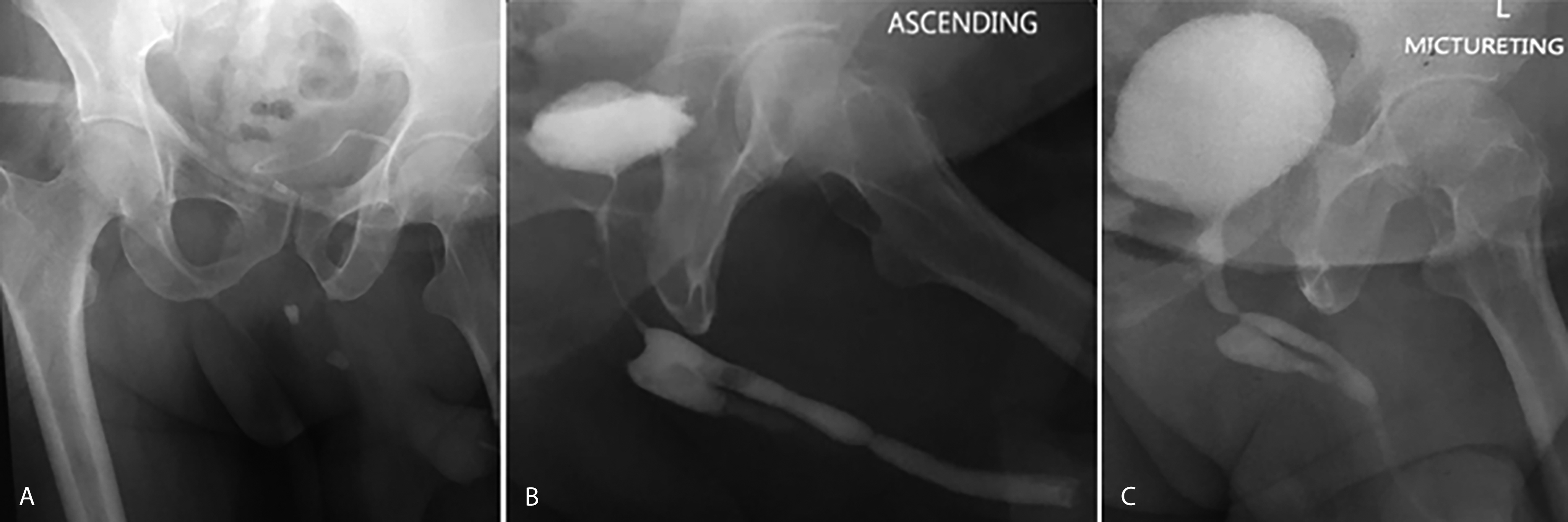 Figure 1: Urethrogram: (A) Plain X-ray film with two radio-opaque shadows in bulbar urethra. (B and C). Ascending and Micturating Urethrogram: Two narrowings at peno-bulbar and the bulbo-membranous junction with diverticulum at bulbar urethra and free flow of contrast into bladder.
Figure 1: Urethrogram: (A) Plain X-ray film with two radio-opaque shadows in bulbar urethra. (B and C). Ascending and Micturating Urethrogram: Two narrowings at peno-bulbar and the bulbo-membranous junction with diverticulum at bulbar urethra and free flow of contrast into bladder.
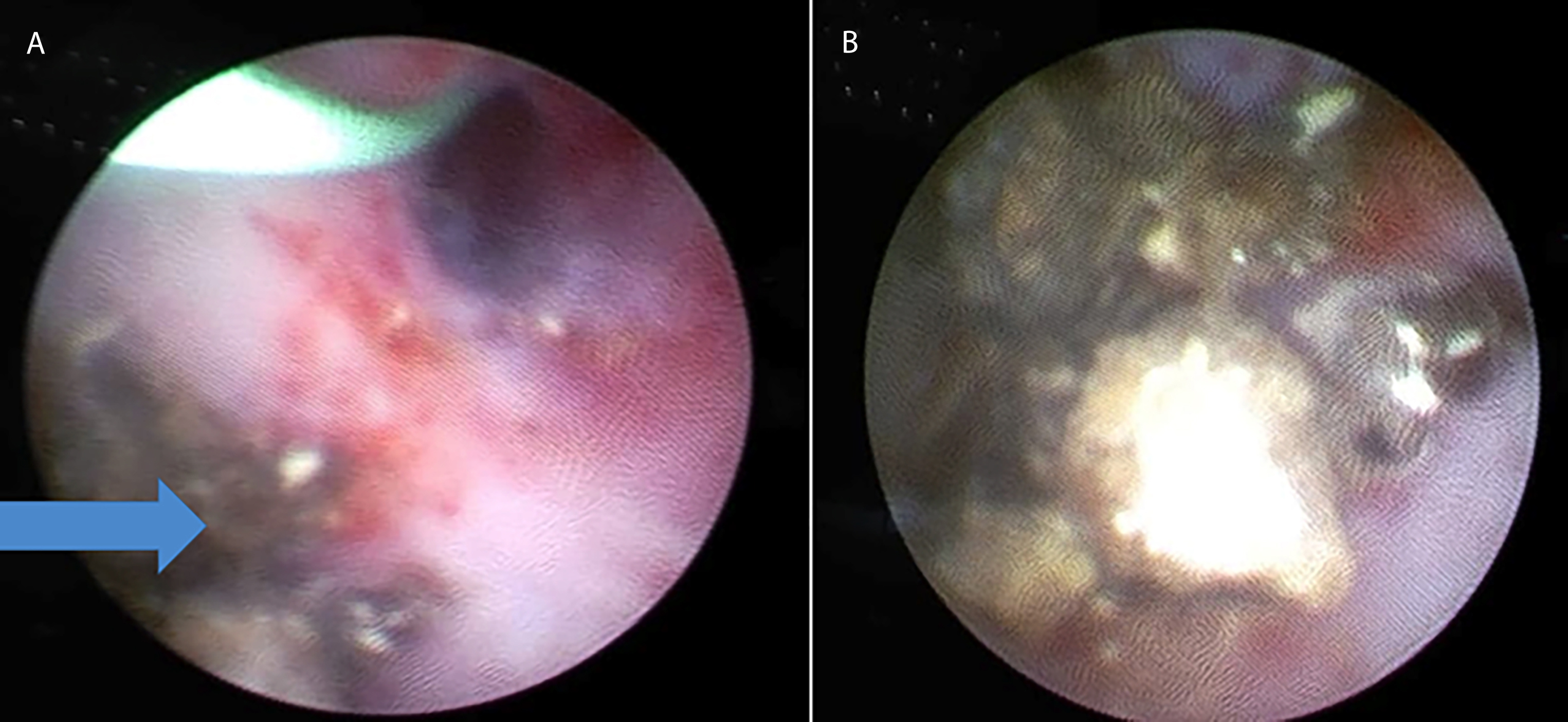 Figure 2: Endoscopic images: (A) Opening of the diverticulum (arrow); stone fragments pouting from a diverticulum. (B) Multiple stones in the urethral diverticulum.
Figure 2: Endoscopic images: (A) Opening of the diverticulum (arrow); stone fragments pouting from a diverticulum. (B) Multiple stones in the urethral diverticulum.
DISCUSSION
UD in males is a rare entity but should not be forgotten while evaluating a male with LUTS and recurrent UTIs. There are 2 types of male UD; congenital (10%) and acquired (90%).1 The former type is due to deficient closure of urethral folds on its ventral aspect leading to a segmental defect in the urethral wall. This type presents earlier in life and is mostly localized in the anterior urethra, particularly at peno-scrotal junction.3
Acquired UD generally develops secondary to increased urethral pressure. Causes include urethral stricture, meatal stenosis, urethral instrumentation or trauma, and drainage of a prostatic or peri-urethral abscess.3 In contrast to congenital diverticulum, they are located mostly in the posterior urethra, and are lined by granulation tissue with the wall devoid of the muscle layer. Regarding the pathogenesis, Ganabathi et al.4 proposed that rupture of peri-urethral glands into urethral lumen secondary to obstruction leads to the formation of a peri-urethral cavity and subsequent epithelialization. This later gets further dilated due to straining and backpressure.
The differential diagnosis includes epidermoid inclusion cysts, sequestration cysts, and cystic dilatation of Cowper’s gland.1 Majority of patients with UD are either asymptomatic or present with signs and symptoms of poor flow, intermittency, dysuria, post-void dribbling, painless peno-scrotal/perineal lump, recurrent UTIs, and rarely with pus discharge and formation of a urinary fistula.5
Calculus formation in UD is reported in 4-10% of patients, likely due to urinary stasis, infection, and crystallization with subsequent growth and formation of stone. AUR is rare in UD as the actual urethral lumen is not completely occluded.
Radiological evaluation of UD is important for determining the treatment modality.3 A plain x-ray KUB (Kidney, Ureter, and Bladder) may demonstrate a radio-opaque density in the line of the urethra. Urethrogram can determine many features of UD such as location, size, and neck of diverticulum, and caliber of urethra proximal and distal to it. Ultrasound of the urethra provides information regarding the thickness of wall. The role of magnetic resonance imaging (MRI) is also evolving.
Endoscopic evaluation, i.e., urethro-cystoscopy gives the assessment of the entire lower tract including the condition of urethral mucosa, any associated strictures, valves, neck of the diverticulum, and feasibility of definitive endoscopic management.5
Literature on optimal treatment options is still growing. Fragmentation by laser or pneumatic lithoclast as a treatment of UD stones has been reported in a limited number of cases as an option.5 Small diverticulum can be managed by endoscopic de-roofing of the diverticular sac. Sun et al.6 described a case of an 82-year male with 6 years history of LUTS and swelling in the perineum. His workup revealed a giant stone in bulbar UD which was managed using combined ultrasonic and pneumatic lithotripsy while the diverticulum was left untreated.
Open reconstructive surgery is required for complicated cases such as large stone burden, unhealthy/ infected tissue, or cases of the thick fibrotic diverticular wall. Complicated cases such as fistula require secondary closure with reinforcement with skin/ buccal mucosal grafts.1 Pandey et al.7 reported a 26-year gentleman who had 3 years history of severe voiding dysfunction following injury to the perineum associated with a midline perineal swelling. Urethrogram revealed a large UD compressing the anterior urethra. Open excision of UD was performed.
Alsowayan et al.8 performed robot-assisted laparoscopic diverticulectomy in 2 pediatric cases and found better visualization, meticulous dissection, and resection with this technique. This approach also has the advantage of reduced morbidity, blood loss, pain, and short hospitalization. They recommended this technique to be a feasible alternative to open excision.
Cinman et al.1 reviewed 22 men with acquired UD. The majority had urinary dribbling as presenting symptom; however, none of them presented with urinary retention. Nineteen (86%) patients had a prior history of urological procedures including urethral stricture surgery and hypospadias repair. Only one patient was found to have calculus in UD managed with excision of the diverticulum with primary end-to-end anastomosis.
Our case was unique as the UD was communicating with the anterior urethra, the patient presented with AUR and his diverticular stones and stricture were managed with minimally invasive urethroscopic surgery. It is hard to conclude whether this was an acquired diverticulum secondary to distal stricture or a long-standing asymptomatic diverticulum with stone formation that led to the formation of stricture.
Male UD poses both diagnostic and surgical challenges owing to the rarity of this condition and its atypical presentation. This condition should be kept in mind while evaluating a male patient with LUTS.
PATIENT’S CONSENT:
Informed consent was obtained from the patient to publish the data concerning this case.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
SMN: Contributed to patient related data including patient consent, literature search, writing of the manuscript, and final review.
RSR: Contributed to patient-related clinical data and literature search.
KK: Contributed to patient-related radiology data and literature search.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Cinman NM, McAninch JW, Glass AS, Zaid UB, Breyer BN. Acquired male urethral diverticula: Presentation, diagnosis and management. Urol 2012; 188(4):1204-8. doi: 10.1016/j.juro.2012.06.036.
- Greiman AK, Rolef J, Rovner ES. Urethral diverticulum: A systematic review. Arab J Urol 2019; 17(1):49-57. doi: 10.1080/2090598X.2019.1589748.
- Thakur N, Sabale VP, Mane D, Mullay A. Male urethral diverticulum uncommon entity: Our experience. Urol Ann 2016; 8(4):478-82. doi: 10.4103/0974-7796. 192094.
- Ganabathi K, Leach GE, Zimmern PE, Dmochowski R. Experience with the management of urethral diverticulum in 63 women. J Urol 1994; 152(5 Pt 1):1445‑52. doi: 10.1016/s0022-5347(17)32442-4.
- Mohanty D, Garg P, Jain B, Bhatt S. Male urethral diverticulum having multiple stones. Ann Med Health Sci Res 2014; 4(1):S53-5. doi: 10.4103/2141- 9248.1317.
- Sun M, Xu W, Guo S, Ma W, Xu H, Sun R. Giant urethral calculus in anterior urethral diverticulum: a case report. BMC Urol 2019; 19(1):71. doi: 10.1186/ s12894-019-0498-9.
- Pandey S, Aggarwal A, Sharma D, Goel A. Rare cause of voiding dysfunction in an adult man: Urethral diverticulum compressing the anterior urethra. BMJ Case Rep 2018; 2018: pii: bcr-2018-226446. doi: 10.1136/bcr-2018-226446.
- Alsowayan O, Almodhen F, Alshammari A. Minimally invasive surgical approach to treat posterior urethral diverticulum. Urol Ann 2015; 7(2):273-6. doi: 10.4103/ 0974-7796.152950.