Laparoscopic Management of Intestinal Obstruction due to a Tight Muscular Cuff Following Transanal Endorectal Pull-through for Hirschsprung’s Disease
By Vanesa Villamil1, Juana Maria Sanchez Morote2, Maria Josefa Aranda Garcia2, Ramon Ruiz Pruneda2, Maria Fernandez Ibieta2Affiliations
doi: 10.29271/jcpsp.2022.08.S177ABSTRACT
Complications of Hirschsprung’s disease‘s surgery include the general complications of any abdominal surgery, but one of the specific complications is obstruction, which occurs in 10% of children after surgical correction and can be due to a narrowing muscular cuff or a coloanal anastomotic stenosis.
We report a case of a 4-month baby, diagnosed as suffering from Hirschsprung‘s disease, who developed postoperative constipation after transanal endorectal pull-through due to unusual folding of the muscular cuff, which narrowed the colon. A laparoscopic approach was performed. During the surgery, it was observed that the muscular cuff was rolled down, surrounding the neorectum. The anterior rectal cuff was completely divided from the pulled-through colon. After surgery, no intraluminal stenosis was revealed on digital rectal examination.
A long and tight rectal muscular cuff could be the reason for postoperative obstructive side effects. The use of laparoscopy has the advantage of confirming the suspected diagnosis and a clear visualisation of the rectal cuff.
Key Words: Hirschsprung disease, Intestinal obstruction, Laparoscopy.
INTRODUCTION
One of the most recognised complications after final treatment for Hirschsprung's disease (HD) is constipation. Obstructive manifestations occur in 9% - 40% of the patients after what appears to be a technically perfect intervention.1 Muscular cuff narrowing and coloanal anastomotic stenosis are reported as reasons for intestinal obstruction.2,3
We report a case of a 4-month baby who developed postoperative constipation after transanal endorectal pull-through (TEPT) due to unusual folding of the muscular cuff, which narrowed the colon, which was corrected laparoscopically. The use of laparoscopy has the advantage of confirming the suspected diagnosis and a clear visualisation of the rectal cuff.
CASE REPORT
A female neonate was born at 38 weeks of gestation and was referred to our institution due to a suspicious bowel obstruction. She did not have any bowel movements since birth and also presented with vomiting and abdominal distention. The patient started with stooling after rectal stimulation and saline irrigations with a Foley probe, without any spontaneous deposition.
With the prediagnosis of HD, a contrast enema was performed, showing a narrowed recto-sigmoid colon with a dilated descending colon. At one month of age, anorectal manometry was done, identifying absence of the rectoanal inhibitory reflex in response to rectal distension.
When the patient was 2 months old, we did the rectal biopsy, which showed aganglionosis and the presence of hypertrophic nerves, consistent with the diagnosis of HD.
TEPT procedure was performed at the age of 4 months. A submucosal plane was created and extended for six cm, leaving a muscular cuff of that length. The rectal cuff was inverted and withdrawn from the anus. It was split along its entire length in a "V" shape on the posterior rectal wall, reaching almost the level of the anastomosis, and the remaining muscle coat was returned into the anal canal. The entire surgical procedure was done without any inconvenience.
Four weeks after surgery, the patient was admitted again with complaints of bloating, vomiting, and absence of stool. A stenotic distal colon was seen on a barium enema, therefore, an MRI was performed, which showed a tight muscular cuff, causing narrowing of the distal neo-rectum (Figure 1A-D). A ring-like circumferential muscular thickness 5 cm from the anal margin was observed on physical examination. There was no anastomotic stricture. Mechanical dilation was attempted but was not effective in solving the stenosis.
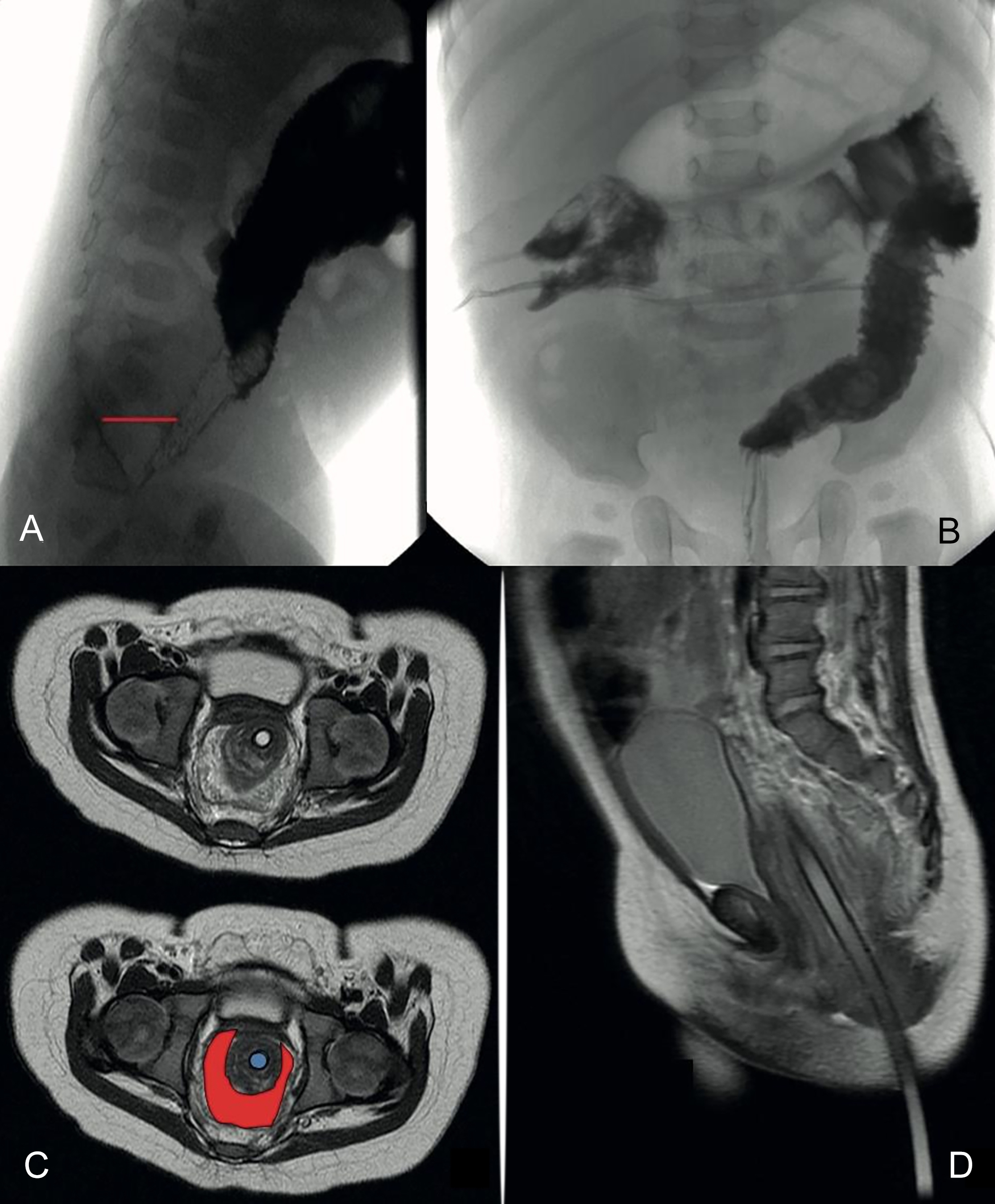 Figure 1: (A) Contrast enema 4 weeks after the pull-through. The line indicates the increased distance between the neo-rectum and the sacrum. (B) Note the stenotic distal neo-rectum. (C) MRI after transanal endorectal pull-through (TEPT). The circle in the middle is the probe surrounded by the folded and obstructing muscular cuff. (D) Lateral view. Note the distance between the probe and the sacrum.
Figure 1: (A) Contrast enema 4 weeks after the pull-through. The line indicates the increased distance between the neo-rectum and the sacrum. (B) Note the stenotic distal neo-rectum. (C) MRI after transanal endorectal pull-through (TEPT). The circle in the middle is the probe surrounded by the folded and obstructing muscular cuff. (D) Lateral view. Note the distance between the probe and the sacrum.
When the patient was under general anesthesia, a rectal biopsy was performed for histological evaluation, confirming that the neorectum was a normo-ganglionic pulled-through colon. Then, a laparoscopic approach was made. The muscular cuff was rolled down, encircling the neorectum. There was an evident plane between the cuff and the colon without any adhesion. The anterior rectal cuff was completely divided from the pulled-through colon (Figure 2A-D). After surgery, no intraluminal stenosis was revealed on digital rectal examination.
On the 3rd day after surgery, the infant was discharged home with proper oral intake, no signs of abdominal distention and stooling several times per day.
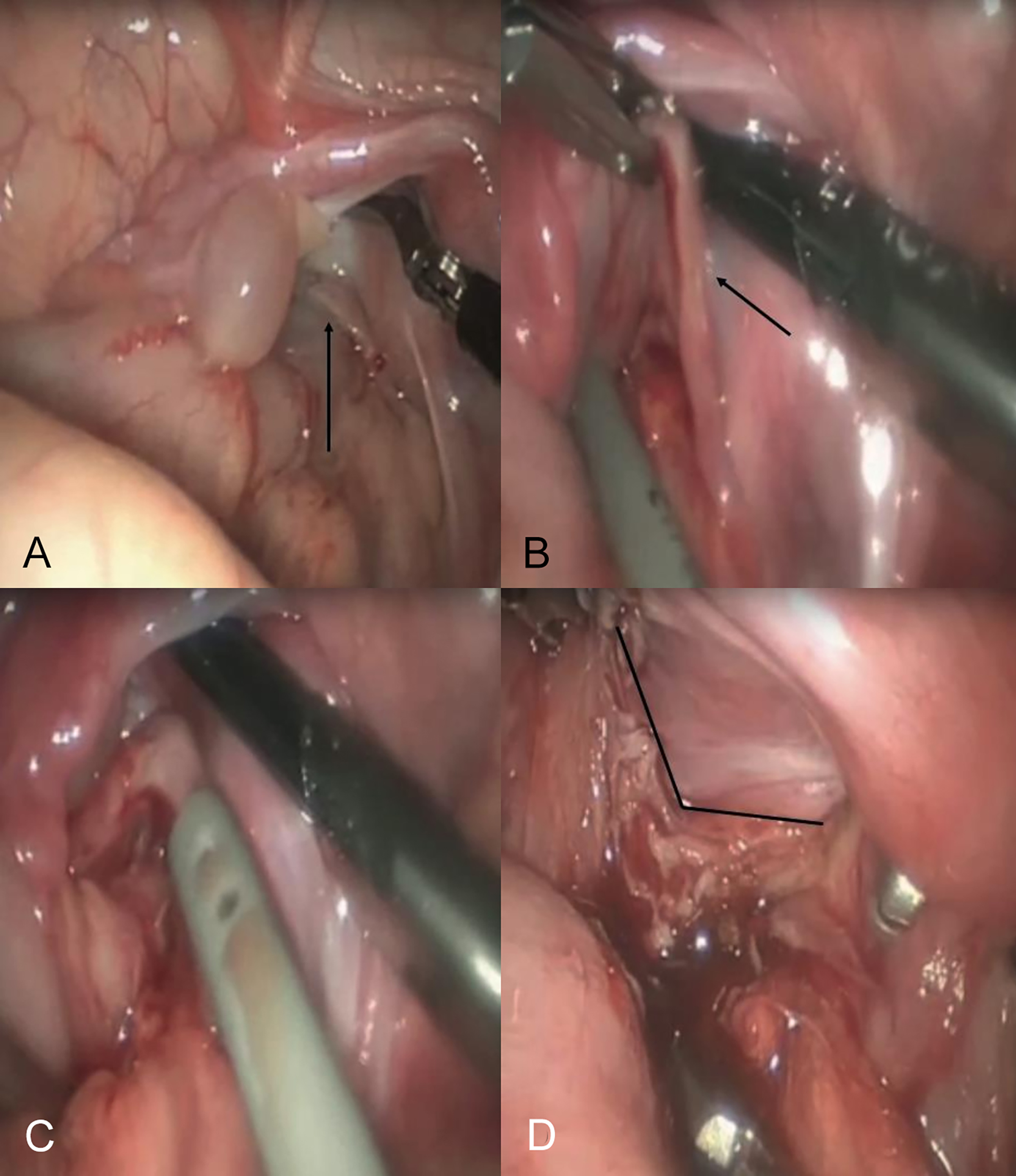 Figure 2: (A, B) Laparoscopic view. The arrows indicate the muscular cuff. (C) Beginning of laparoscopic resection. (D) The muscular cuff has been completely divided.
Figure 2: (A, B) Laparoscopic view. The arrows indicate the muscular cuff. (C) Beginning of laparoscopic resection. (D) The muscular cuff has been completely divided.
One year after the surgery, the patient has a completely normal life.
DISCUSSION
TEPT procedure has been and is still being used by many pediatric surgeons, and numerous scientific studies have been published that demonstrate the feasibility of this technique.4
Although the advantages of performing the procedure transanally are clear, there are some reasonable drawbacks, such as the formation of stenosis and enterocolitis.5
In an article published in 2012, it was suggested that when stenosis is found in the upper part of the anal canal, it can generally be expected to be the direct result of an ischemic segment.1 Now, this case demonstrates that there is another cause besides the ischemic one. In this case, as in another case published in 2006, anastomotic leakage was unlikely as the main cause because the narrowing was found above the coloanal anastomotic site. Neorectal biopsy demonstrated that the pulled-through colon was normo-ganglionic, ruling out the possibility of transitional innervation.3
The rectal cuff can cause mechanical obstruction if it is not divided satisfactorily or if a long length of it is left in the patient.6 Many experts recommend a posterior muscular cuff´s myectomy fully down to the pectinate line to prevent residual constipation.2,3 On the other hand, Levitt et al. and De la Torre et al. found that despite the division of the muscular cuff during the first procedure, it can sometimes curl downward, narrowing the pulled-through colon and causing difficulty in stool passage, with resultant intestinal obstruction predisposing the patient to enterocolitis, as in the present case.6,7
There are several approaches which we can diagnose a tight muscular rectal cuff, such as digital rectal examination, contrast enema that would reveal an increased distance between the neo-rectum and the sacrum and, finally, an MRI, which may be necessary to confirm the diagnosis.2,6
Numerous cuff-related strictures and narrowings can be resolved using repeated dilations. If dilatations are unsuccessful, the patient may require surgical correction.7
Peña et al. reviewed 21 patients with some kind of stricture or acquired atresia of the rectum. They postulated a posterior sagittal approach to be used in the reoperation of these patients.8 We think that the laparoscopic approach is the best option because it is less invasive than a sagittal approach, without making any incision, with no stitches, and without touching the pulled-through colon.
In summary, we recommend a thorough split of the muscular cuff and leaving a shorter one to minimise postoperative complications to be considered in the initial surgery. In this case, the obstructive complication was managed safely by laparoscopic cuff myectomy.
PATIENT'S CONSENT:
Informed consent was obtained to publish the data concerning this case.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
VV: Designed the study, drafted the initial manuscript, approved the final manuscript as presented, and agrees to be responsible for all aspects of the work to ensure that questions related to the accuracy or completeness of any part of the work are investigated and resolved appropriately.
JMSM: Carried out the initial analysis, coordinated and supervised the data collection, critically reviewed the manuscript, approved the final manuscript as presented, and agrees to be responsible for all the aspects of the work to ensure that the questions related to the accuracy or completeness of any part of the work are properly investigated and resolved.
MJAG: Performed the initial analysis, critically revised the manuscript, approved the final manuscript as presented, and agrees to be responsible for all the aspects of the work to ensure that questions related to the accuracy or completeness of any part of the work is properly investigated and resolved.
RRP: Coordinated and supervised the data collection, reviewed the manuscript, approved the final manuscript as presented, and agrees to be responsible for all aspects of the work to ensure that questions related to accuracy or integrity of any part of the work are duly investigated and resolved.
MFI: Reviewed the manuscript, approved the final manuscript as presented, and agrees to be responsible for all aspects of the work to ensure that questions related to accuracy or integrity of any part of the work are duly investigated and resolved.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Ralls MW, Coran AG, Teitelbaum DH. Reoperative surgery for hirschsprung disease. Semin Pediatr Surg 2012; 21(4):354-63. doi: 10.1053/j.sempedsurg.2012.07.011.
- Hay SA, El Shafei I, El Debeky M, Bassiouny A. Release of obstructing rectal cuff following transanal endorectal pullthrough for Hirschsprung´s disease: A laparoscopic approach. Ann Pediatr Surg 2012; 8:90-2.
- Shimotakahara A, Yamataka A, Kobayashi H, Miyano G, Kusafuka J, Lane GJ, et al. Obstruction due to rectal cuff after laparoscopy-assisted transanal endorectal pull-through for Hirschsprung's disease. J Laparoendosc Adv Surg Tech A 2006; 16(5):540-2. doi: 10.1089/lap.2006. 16.540.
- Kim HY, Oh JT. Stabilisation period after 1-stage transanal endorectal pull-through operation for Hirschsprung disease. J Pediatr Surg 2009; 44(9):1799-804. doi: 10.1016/j.jpedsurg. 2008.10.070.
- Masiakos PT, Ein SH. The history of Hirschsprung´s disease: Then and now. Semin Colon Rectal Surg 2006; 17:10-9.
- Levitt MA, Dickie B, Pena A. Evaluation and treatment of the patient with Hirschsprung disease who is not doing well after a pull-through procedure. Semin Pediatr Surg 2010; 19(2):146-53. doi: 10.1053/j.sempedsurg.2009.11.013.
- De La Torre L, Langer JC. Transanal endorectal pull-through for Hirschsprung disease: Technique, controversies, pearls, pitfalls, and an organised approach to the management of postoperative obstructive symptoms. Semin Pediatr Surg 2010; 19(2):96-106. doi: 10.1053/j.sempedsurg. 2009. 11.016.
- Pena A, Elicevik M, Levitt MA. Reoperations in Hirschsprung disease. J Pediatr Surg 2007; 42(6):1008-14. doi: 10. 1016/j.jpedsurg.2007.01.035.