It does Exist! Traumatic Hemorrhage in Septum Pellucidum
By Murat Seyit1, Arif Osun2, Atakan Yilmaz1, Mert Ozen1, Duygu Aras Seyit3Affiliations
doi: 10.29271/jcpsp.2022.08.S139ABSTRACT
Although bleeding into the septum pellucidum often occurs in the presence of a tumour, trauma-induced septal pellucidum hemorrhage has not been reported yet, as far as the current literature is concerned. The absence of hemorrhage on the first post-trauma imaging of the patient but the presence of hemorrhage in the brain tomography taken 12 hours later reveals the existence of trauma-induced septum pellucidum hemorrhage.
Key Words: Head trauma, Brain injury, Septum pellucidum, Hemorrhage.
INTRODUCTION
Though septum pellucidum hemorrhages rarely occur often in the presence of a tumor, septum pellucidum hemorrhages due to trauma have not been reported so far. However, it is reported that the size of the septum pellucidum may increase due to chronic trauma. In post-mortem studies, cavum septu pellucidum (CSP) is designated as one of the causes of chronic traumatic encephalopathy.1
We, herein, present a case of a 61-year male patient admitted to the Emergency Department (ED) because of a history of traffic accidents. Initial computed tomography was unremarkable. Vitally he was stable and discharged after 6 hours of observation. However, he was re-admitted 5 hours after discharge with a history of syncope, and repeat computed tomography at this time revealed hemorrhage in the septum pellucidum which resolved on conservative treatment.
CASE REPORT
A 61-year male patient was brought to the Emergency Department (ED) by the medical team after a non-vehicle traffic accident. On initial hemodynamic monitoring, his blood pressure was 110/70 mm Hg, pulse was 105 beats/min, respiration was 14 breaths/min, and SpO2 was 98%.
During his physical examination, there were no obvious signs except for 2×3cm superficial dermal abrasion in the frontal region. During his neurological examination, his Glasgow Coma Score (GCS) was 15, and he was well-oriented to person, place, and time and was cooperative. As he suffered post-traumatic amnesia and could not recall how the event occurred, his cervical and brain tomography was taken (Figure 1). The initial scans did not show any noticeable signs in the brain and cervical region, he was monitored in the ED for 6 hours. The patient, whose overall status did not worsen because of normal follow-up and stable vital signs. He was discharged from the ED after oral intake (eating) with some recommendations and information about the complications that may occur after head trauma. The patient was re-admitted to the same ED 5 hours after discharge because of complete syncope. The control tomography of the patient, whose vitality was stable with GCS of 15, was taken following the re-examination. Upon detecting a hematoma (Figure 2) in the septum pellucidum (interhemispheric fissure), which did not appear in the first tomography, a neurosurgery specialist was consulted. A conservative treatment was planned for the patient admitted to the intensive care in the neurosurgery unit for follow-up. After the follow-up of the patient, monitored for 7 days, he was discharged as a result of the regression of the hematoma in the brain tomography with the recommendation of an outpatient clinic follow-up. Besides, the hemorrhage was observed to be resorbed in his control tomography after 14 days (Figure 3).
DISCUSSION
Traumatic Brain Injuries (TBI) account for half of the deaths due to more than 1.35 million traffic accidents and injuries due to 50 million traffic accidents worldwide.2 Head injuries in vehicle pedestrian collisions may include injuries, such as skull bones fracture, laceration, contusion, concussion, intracranial hematoma, and common axonal injuries.
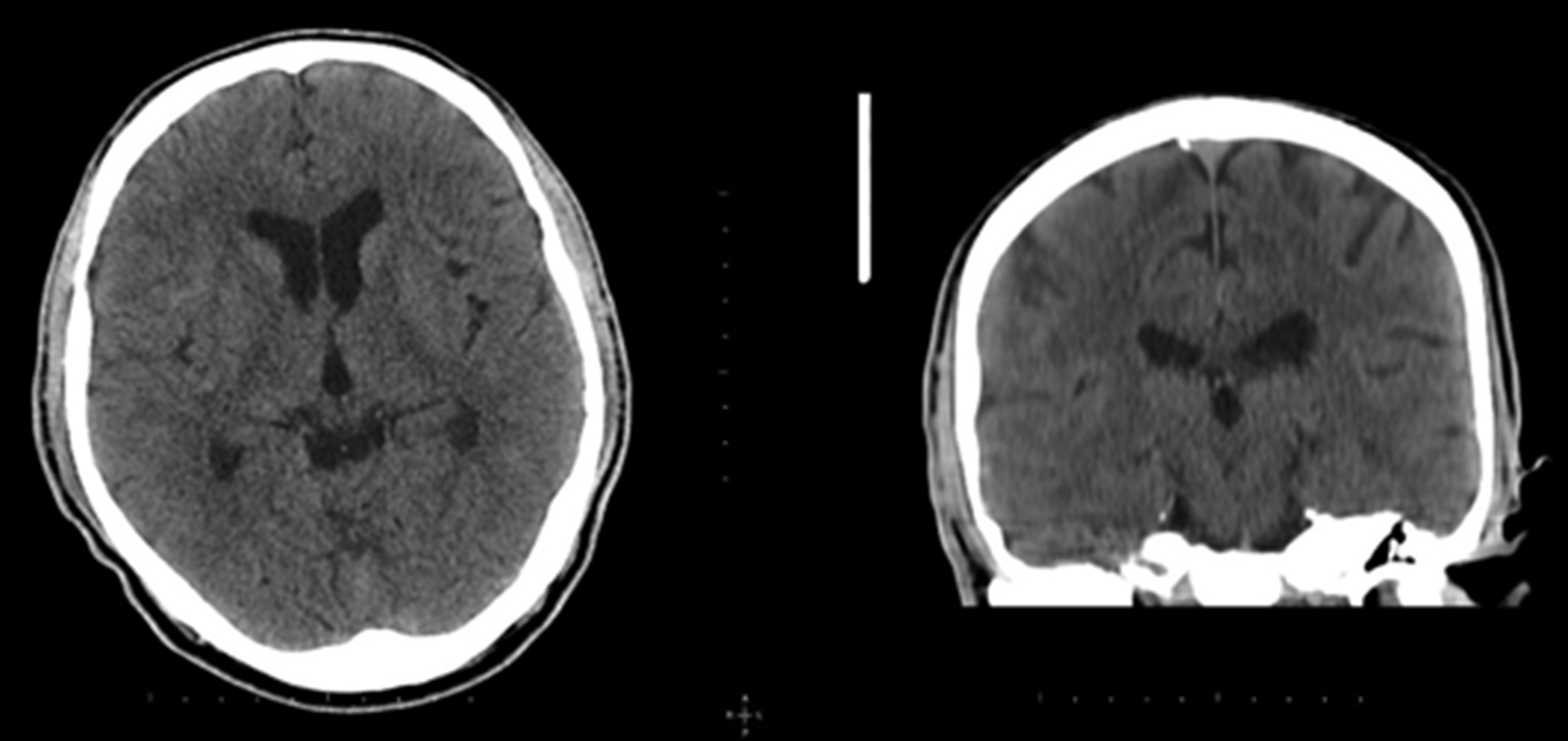 Figure 1: Patients first normal tomography.
Figure 1: Patients first normal tomography.
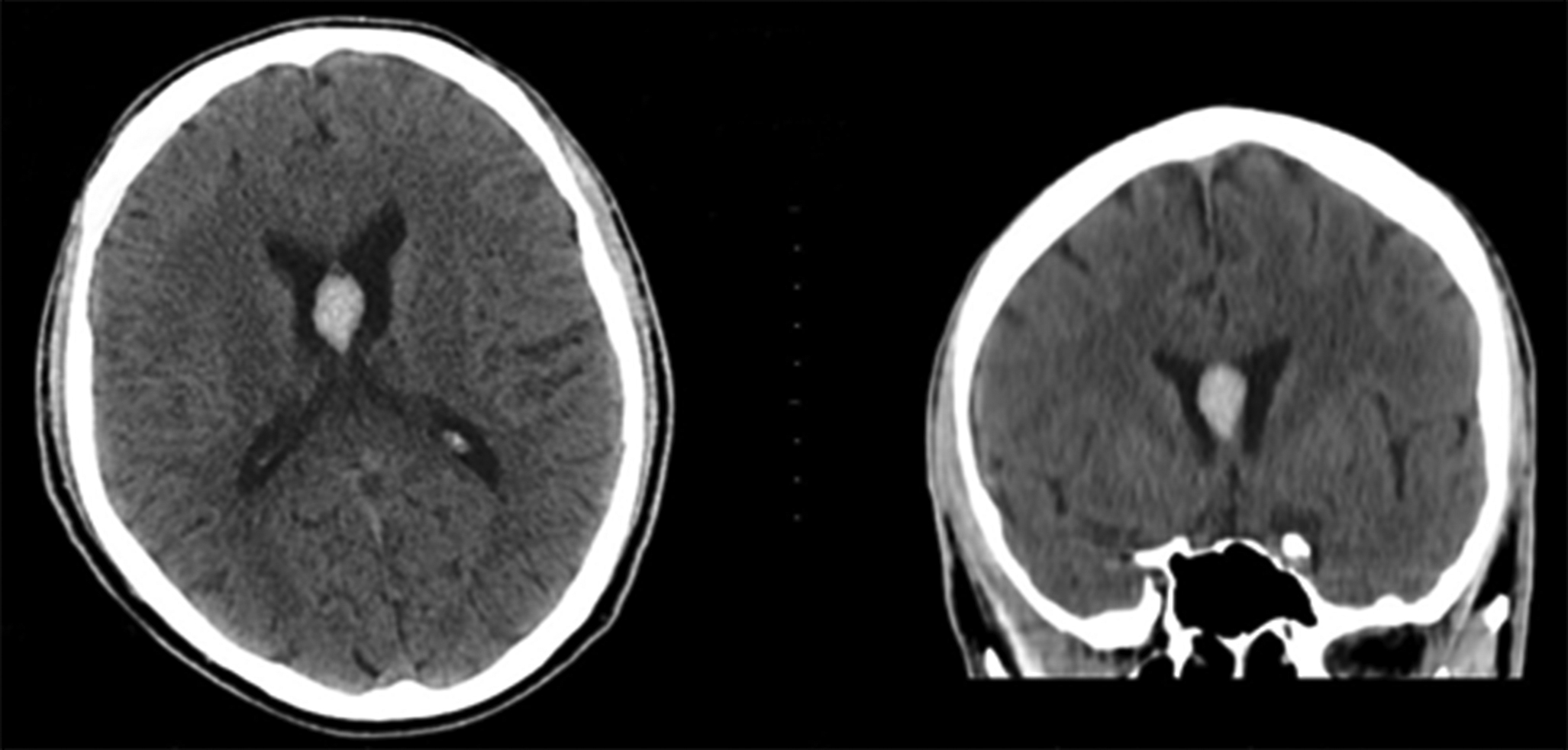 Figure 2: Hematoma in the septum pellucidum.
Figure 2: Hematoma in the septum pellucidum.
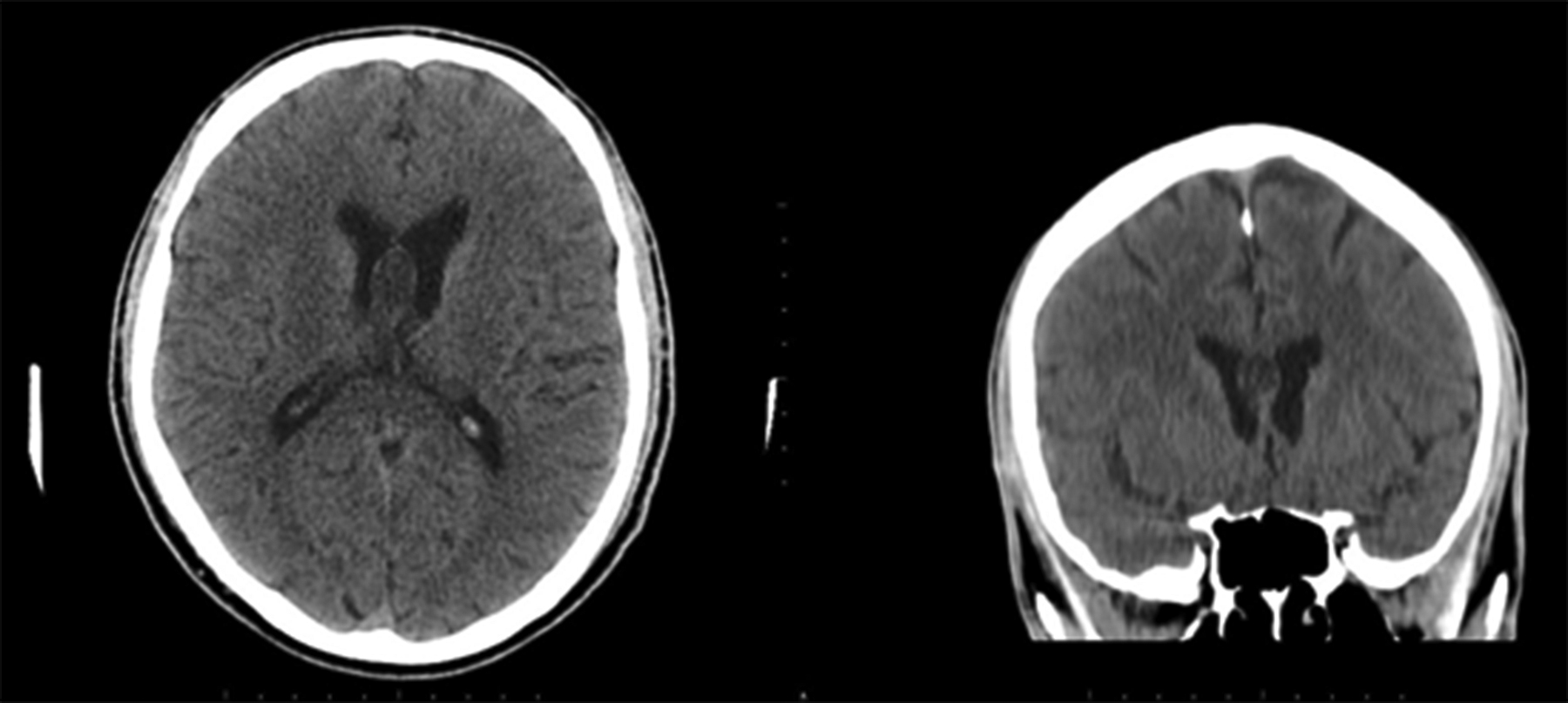 Figure 3: Resorbed hematoma in control tomography.
Figure 3: Resorbed hematoma in control tomography.
CSP is a fluid-filled, midline cavity bordered by thin septum pellucidum leaves trapped between the third ventricle and corpus callosum. The common embryological origins of the septum pellucidum, corpus callosum, and limbic system explain the anatomical basis for the simultaneous involvement of these structures in varying degrees, both in developmental and acquired disease processes.3 When both leaves of septum pellucidum do not merge completely and a separate cystic section appears in the lateral ventricles, it is called cavum vergae (CV).
After assessing the cerebral angiography of a 16-year-old male patient with spontaneous subarachnoid bleeding, Yanaka et al. reported that an aneurysm rupture developed in the anterior cerebral artery which bled into the CSP. In our case, angiography was not performed since aneurysm was not suspected in the follow-up by neurosurgery.4
In his letter to the editor entitled “Hemorrhage in cavum septum pellucidum et vergae: it does exist!” published in 2015, Ghuman et al. state that a 70-year-old female patient was admitted with the complaints of severe headache related to vomiting and that hemorrhage was identified in her CSP.5 Although intraventricular hemorrhage (IVH) and subsequent hydrocephalus frequently occur due to the rupture of cerebral aneurysms and vascular malformations, a dearth of caval-septal hematomas in the published literature remains unexplained. While Ghuman et al.5 report hemorrhage induced by aneurysm rupture in their case, our case showed that trauma-induced septum pellucidum hemorrhage did not appear in the first brain tomography, and that hemorrhage was identified in the repeat computed tomography and resorbed over time with conservative management.
In conclusion, this case is the first in the literature of a traumatic hemorrhage in septum pellucidum that was missed on initial computed tomography and detected on readmission and resolved without active intervention.
ACKNOWLEDGEMENTS:
I would like to thank Dr. Emine Kadioglu and Dr. Murat Korkmaz for the follow-up of the patient.
PATIENT’S CONSENT:
Informed consent was taken from the patient's parents for publication of this case report and related images.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
MS: Searched the literature and has written the whole case report.
AO: Helped in literature review and discussion writing.
AY: Revised it critically for important intellectual content; final approval of the version to be published.
MO: Highlighted the importance of the case, and suggested to work upon this case.
DAS: Conception, drafting, and critical review.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Koerte IK, Hufschmidt J, Muehlmann M, Tripodis Y, Stamm JM, Pasternak O, et al. Cavum septi pellucidi in symptomatic former professional football players. J Neurotrauma 2016; 33(4):346-53. doi: 10.1089/neu. 2015.3880.
- Global status report on road safety – 2018: Supporting the decade. Geneva, World Health Organization, 2018. www.who.int/violence_injury_prevention/road_safety_status/2018/en/. (Accessed on 1/20/2020).
- Sarwar M. The septum pellucidum: Normal and abnormal. AJNR Am J Neuroradiol 1989; 10(5):989-1005.
- Yanaka K, Meguro K, Narushima K, Takano S, Doi M, Nose T. Basal perforating artery aneurysm within the cavum septi pellucidi. Case report. J Neurosurg 1998; 88(3):601-4. doi: 10.3171/jns.1998.88.3.0601.
- Ghuman MS, Gupta V, Kumar A, Tiwari MK, Khandelwal N. Hemorrhage in cavum septum pellucidum et vergae: It does exist! Acta Neurochir (Wien) 2015; 157(9):1489-91. doi: 10.1007/s00701-015-2508-3.