Improvement of Three Duodenal Re-leaks: Two-way Vacuum-assisted Closure
By Ali Alemdar, Seracettin EginAffiliations
doi: 10.29271/jcpsp.2022.04.15ABSTRACT
We share our experience of a two-way vacuum-assisted closure (VAC) technique that allows patients to heal when generalised peritonitis develops because of a recurrent duodenal leak. Two patients underwent omentoplasty for duodenal ulcer perforation and one patient underwent antrectomy, gastrojejunostomy, and tube duodenostomy. Two-way VAC was performed by taking an abdominal fluid culture and washing the abdomen with 6–12 litres of warm saline. Two-way VAC exchange procedures were continued every 3 days and total parenteral nutrition was administered until cessation of the duodenal re-leak. The two-way VAC application was terminated when improvement in the re-leak was macroscopically detected. The subcutaneous layer was dissected from the anterior abdominal wall fascial layer, and the abdominal skin was closed without tension. The patients were subsequently discharged. Controlling the primary source is often difficult when treating duodenal re-leaks, and two-way VAC can localise the source of the peritonitis and remove toxic peritoneal material.
Key Words: Open abdomen, Vacuum-assisted closure, Severe peritonitis, Duodenal leak.
INTRODUCTION
Recurrent duodenal leak, following omentoplasty to treat acute duodenal ulcer perforation, is an extremely difficult complication to manage, and it has a high mortality rate. Re-leak incidence after omentoplasty was reported as 4–16% in two studies.1,2 If the duodenal stump cannot be closed after antrectomy in a large duodenal ulcer perforation, the tube duodenostomy is preferred. However, most tube duodenostomies leak from the edges into the abdomen.
Table I: Demographic and other relevant data of the three cases.
Patient 1
Patient 2
Patient 3
Age (years)
55
83
48
Gender
Male
Female
Male
Postoperative day of duodenal re-leak and relaparotomy
2
9
6
Postoperative day of the two-way VAC
2
9
6
Duration of the two-way VAC (day)
39
17
62
Number of the two-way VAC
12
4
15
Microorganism reproducing in intra-abdominal fluid culture
Acinetobacter baumannii
Enterococcus faecalis
Candida albicans
Klebsiella pneumoniae
Diameter of perforation in the duodenum
20 mm
10 mm
20 mm
Type of the first operation
Omentoplasty
Omentoplasty
Antrectomy, gastrojejunostomy,
tube duodenostomy
Length of hospital stay (days)
129
48
71
Length of ICU stay (days)
95
23
2
Vacuum-assisted closure (VAC), intensive care unit (ICU).
Two patients underwent omentoplasty to treat duodenal ulcer perforation and one patient underwent antrectomy, gastrojejunostomy, and tube duodenostomy. We present a two-way vacuum-assisted closure (VAC) technique that allowed those patients to heal when generalised peritonitis developed because of a recurrent duodenal leak.
CASE REPORT
The demographic and other relevant data for three consecutive patients with duodenal ulcer perforation are shown in Table I, including the day of postoperative re-leak and relaparotomy, the two-way VAC application duration and the number of applications, the micro-organisms in the intra-abdominal fluid culture, the duodenal perforation diameter, the initial surgery type, length of hospital stay, and length of intensive care unit stay. The second patient had chronic obstructive pulmonary disease, hypertension, and heart failure. The first and third patients had no comorbidities. The first operations of three patients on their emergency admission were performed under generalised peritonitis conditions. The first and third patients were operated by the first author with 20 years of surgical experience. The second patient was operated by another surgeon with 25 years of surgical experience. The two-way VAC applications were completely carried out by the second author with 30 years of surgical experience. Generalised peritonitis was present in three patients because of duodenal re-leaks. The generalised peritonitis and duodenal re-leak in the first patient are shown in Figure 1.
In the first patient, the necrotic omentum was separated from the bulbus duodeni. An adequate omentum was not found for stitching up the omental patch. The duodenal mucosa that was turned outward was excised, and the duodenal perforation was sutured using 2/0 vicryl. In the second patient, the omental patch was not necrotic and had not separated from the bulbus duodeni. However, there was a bile leak under the patch. Additional surgical procedures were not required. In the third patient, there was a bile leak from the edge of the tube duodenostomy. The tube was removed and the duodenostomy was closed by suturing with 2/0 vicryl.
 Figure 1: The generalised peritonitis and duodenal re-leak are shown in the first patient.
Figure 1: The generalised peritonitis and duodenal re-leak are shown in the first patient.
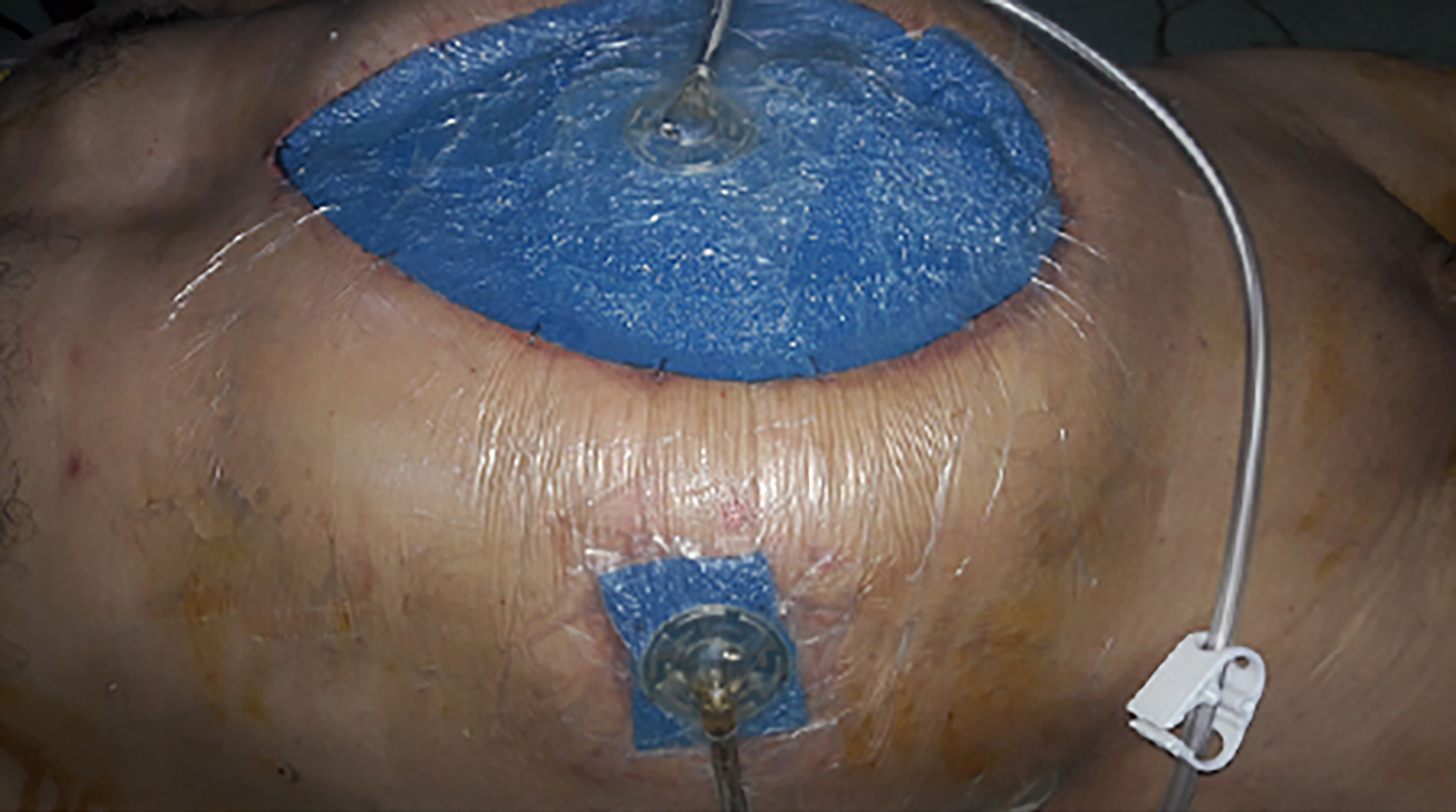 Figure 2. The external appearance of the two-way vacuum-assisted closure technique is shown in the first patient.
Figure 2. The external appearance of the two-way vacuum-assisted closure technique is shown in the first patient.
In the three patients, an intra-abdominal fluid culture was taken before application of the two-way VAC technique and the peritoneal cavity was irrigated with 6–12 litres of warm sterile saline. A two-way VAC management system was applied (ABThera Open Abdomen Management System; Kinetic Concepts Inc./Acelity, L.P. Inc., San Antonio, TX, USA). One arm of the open abdomen management system including six additional sponge arms was extracted by cutting. One tip of the removed additional sponge extension was placed next to the duodenum. The other tip was removed from the upper right quadrant. The remaining open abdomen management system with five additional sponge arms was placed so that it covered the entire abdominal cavity. Two separate collection sets were connected to two separate vacuum devices that were set with a negative pressure of 75 mmHg, one of which was connected to the sponge arm in the middle of the abdomen and the other to the sponge arm in the upper right quadrant. The external appearance of the two-way VAC application can be seen in Figure 2. In all patients, once the duodenal re-leak was detected, total parenteral nutrition (TPN) was started immediately. TPN was continued until the end of the duodenal re-leak. The two-way VAC changes were performed at 3–5-day intervals by culturing and washing the abdomen. The duodenal re-leaks were constantly observed to detect any changes. Nasogastric tube application was maintained until the end of the duodenal re-leak. When no bile was observed in the VAC collection containers, we concluded that the duodenal re-leaks had stopped and the duodenal perforations had completely closed with granulation tissue that developed quickly because of the two-way VAC applications.
In all the patients, when the two-way VAC end applications were removed, no bile leak was observed, and the inside of the abdomen was completely clean. The subcutaneous layer was dissected from the fascial layer of the anterior abdominal wall and the open abdomen was closed.
DISCUSSION
Multiple surgical procedures and conservative methods to manage a re-leak following omentoplasty have been recommended. The largest series with 41 cases were conducted by Saurabh et al.3 Cholecystoduodenoplasty, a jejunal patch, triple-tube-ostomy, T-tube duodenostomy, and conservative methods were recommended by Saurabh et al.3 The mortality rate in their study was 78%, and the success rate of all surgical techniques applied in their study was very low. Saurabh et al.3 stated that 26 of 32 patients died because of sepsis.
The second major series with 17 cases was published by Maghsoudi and Ghaffari in 2011.1 They recommended sub-hepatic drainage and re-insertion of the omental patch, only sub-hepatic drainage, and a jejunal serosal patch. Their mortality rate was lower (29.4%, five cases). Additional surgical procedures that were defined to treat a re-leak after omentoplasty were generally not successful. Unfortunately, the success rate of additional surgical procedures recommended in the above two studies was quite low.
Controlling a persistent source of infection is possible with the application of an open abdomen (OA). Additionally, OA may effectively remove the infected and cytokine-loaded peritoneal fluid. VAC techniques have been extensively used for temporary abdominal closure.4 If controlling the primary source of existing peritonitis is unsuccessful, the OA is an alternative for patients with severe peritonitis and severe sepsis or septic shock (grade of recommendation 2C).5 For generalised peritonitis, sutures are not safe because of the infected and oedematous tissues. Stitched tissues are usually cut by the applied sutures. All types of anastomosis in intra-abdominal sepsis may develop a leak. All surgical procedures in patients with severe peritonitis usually increase the morbidity and mortality rates.
It is not possible to completely control the primary source of the existing peritonitis in patients with a duodenal re-leak. However, it is necessary to localise the duodenal leakage in these patients. The two-way VAC technique can accurately localise the duodenal leakage and remove the toxic liquids that accumulate in the abdominal cavity. Moreover, the VAC system reasonably accelerates the development of granulation tissue; thus, the duodenal leakage closes early with granulation tissue. Low pressure of 75 mmHg is applied so that the duodenal re-leak does not increase because of an excessive negative pressure effect. The two-way VAC technique should cure a re-leak following Roscoe–Graham omentoplasty or a duodenal stump leak following upper gastrointestinal system surgery.
OA complications include enteroatmospheric fistula, infection, bleeding, uncontrolled fluid and protein loss, abdominal area loss, adhesion of organs to the abdominal wall, giant hernias, prolonged intensive care and hospital stay, and increased hospital cost. The most serious complication is a fistula. The most effective way to reduce complications is to close the abdomen as soon as possible. All of the patients in this case report had abdominal area loss, adhesion of organs to the abdominal wall, giant hernia, prolonged intensive care and hospital stay, and increased hospital cost. These complications are acceptable in patients with OA.
In conclusion, control of the primary source is often difficult when treating duodenal re-leaks, and the two-way VAC technique is a convenient solution for localising the source of the peritonitis and removing toxic peritoneal material. Additionally, in recurrent duodenal leaks, intra-abdominal sepsis can be treated without the need for additional surgical procedures using the two-way VAC technique. We acknowledge that this proposed treatment, based on the success of only three cases, should not be generalised. Larger series and randomised controlled studies are needed on this subject.
PATIENTS’ CONSENT:
Informed consents were obtained from all the three patients to publish the data concerning these cases.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
AA: Surgical and medical practices, literature search, conception or design of the work, data collection, data analysis and interpretation, drafting the article.
SE: Surgical and medical practices, data analysis and interpretation, critical revision of the article, final approval of the version to be published.
REFERENCES
- Maghsoudi H, Ghaffari A. Generalised peritonitis requiring re-operation after leakage of omental patch repair of perforated peptic ulcer. Saudi J Gastroenterol 2011; 17(2): 124-8. doi: 10.4103/1319-3767.77243.
- Chalya PL, Mabula JB, Koy M, Mchembe MD, Jaka HM, Kabangila R, et al. Clinical profile and outcome of surgical treatment of perforated peptic ulcers in Northwestern Tanzania: A tertiary hospital experience. World J Emerg Surg 2011; 6:31. doi: 10.1186/1749-7922-6-31.
- Sanjanwala SS, Thatil VN, Rohondia OS, Rambhia SU. Comparison of operative procedures for re-leaks duodenal perforation: A cross-sectional analysis from a tertiary care hospital in a developing country. Int Surg J 2016; 3:1314-7.
- Sartelli M, Abu-Zidan FM, Ansaloni L, Bala M, Beltran MA, Biffl WL, et al. The role of the open abdomen procedure in managing severe abdominal sepsis: WSES position paper. World J Emerg Surg 2015; 10:35. doi: 10.1186/s13017-015- 0032-7.
- Coccolini F, Roberts D, Ansaloni L, Ivatury R, Gamberini E, Kluger Y, et al. The open abdomen in trauma and non-trauma patients: WSES guidelines. World J Emerg Surg 2018; 13:7. doi: 10.1186/s13017-018-0167-4.