Impact of Intragastric Balloon: A Rare Complication
By Ghulam Mujtaba1, Rida Zehra1, Fizra Balkhi1, Numra Shaikh2Affiliations
doi: 10.29271/jcpsp.2022.08.S89ABSTRACT
Non-surgical interventions for weight loss are being used more commonly and one of the emerging endoscopic bariatric therapies is the insertion of Intragastric Balloons (IGBs).
A 58-year Pakistani female, presented with vomiting and abdominal bloating for 2 weeks. The balloon was impacted at the antrum and pylorus while the external pigtail catheter and blue clasp for retrieval were extending into D1/D2. This is a very rare complication of IGB. We report a rare case of antral impaction, followed by safe removal of the impacted Spatz IGB. Regular follow-ups are necessary to avoid serious complications of IGB insertion.
Key Words: Intragastric balloon, Impaction, Obesity, Safe retrieval, Weight-loss.
INTRODUCTION
Overweight and obesity are global public health issues, particularly in affluent societies. The World Health Organisation reported that 39% of adults were overweight [body mass index (BMI), 25 Kg/m2] in 2016 and 13% were obese worldwide (BMI, 30 Kg/m2).1 The likelihood of a cluster of cardio-metabolic diseases such as type 2 diabetes mellitus, hypertension, and dyslipidemia is elevated by excess body weight, along with an increased risk of coronary heart disease, stroke, and mortality.2,3
Endoscopic bariatric therapies are emerging as non-surgical weight-loss interventions that are being used with increasing frequency, and one of those is Intragastric Balloons (IGBs). IGBs are devices that occupy space and are either filled with saline or nitrogen gas. The fluid-filled IGBs function in many ways, including slowing the rate of gastric emptying from the stomach; thus, patients eat smaller meals and experience early satiety for longer periods resulting in weight loss.4,5
Nausea, difficult inflation or deflation of the balloon, unwanted deflation, and migration of the balloon into the small intestine resulting in intestinal obstruction or perforation were the most common side effects associated with the use of these IGBs.2
Antrum is one of the locations for the placement of the balloon and has shown improvements in weight loss relative to other sites of placement.6 Here, We report a rare case of antral impaction, followed by safe removal of the impacted Spatz IGB.
CASE REPORT
A 58-year Pakistani female, with no known comorbid, was brought to OPD with a 2-week history of persistent vomiting and abdominal bloating. She was having 2-3 episodes of vomiting per day, non-bilious, without blood, and usually post-prandial. The patient had no other symptoms of abdominal pain, diarrhea, or constipation.
On examination, the patient was an elderly female, morbidly obese, conscious awake, oriented to time, place, and person, and vitally stable. Her abdomen was distended without any tenderness or guarding. Bowel sounds were normal. The succussion splash was negative. On abdominal ultrasound, moderate fatty liver was the only remarkable finding. Her initial baseline laboratory tests including complete blood count, electrolytes, and serum creatinine were normal. Based on this assessment and keeping in mind the history, as in the past, the patient had undergone an upper gastrointestinal (GI) endoscopy and IGB insertion 10 months ago as a therapy for her class 3 obesity, an initial diagnosis was made of IGB impaction leading to gastric outlet obstruction. Spatz IGB with the infusion of 400 ml normal saline, was placed endoscopically in the stomach as an outpatient procedure and she was discharged the same day without any post-procedure complications. She was prescribed proton pump inhibitors (PPIs) for dyspepsia, to be taken as needed for symptoms.
BMI at the time of placement of IGB was 42 Kg/m2 (weight: 118 kg, height 167.6 cm). The patient then came after 10 months with the aforementioned symptoms, in the OPD.
Now, her BMI was 36.7 Kg/m2 (weight: 103 kg, height 167.6 cm). After 8 hours of NPO, upper GI endoscopy was performed that revealed the silicon balloon impacted at the antrum and pylorus while the external pigtail catheter and blue clasp for retrieval were extending into D1/D2, as shown in Figures 1 and 2.
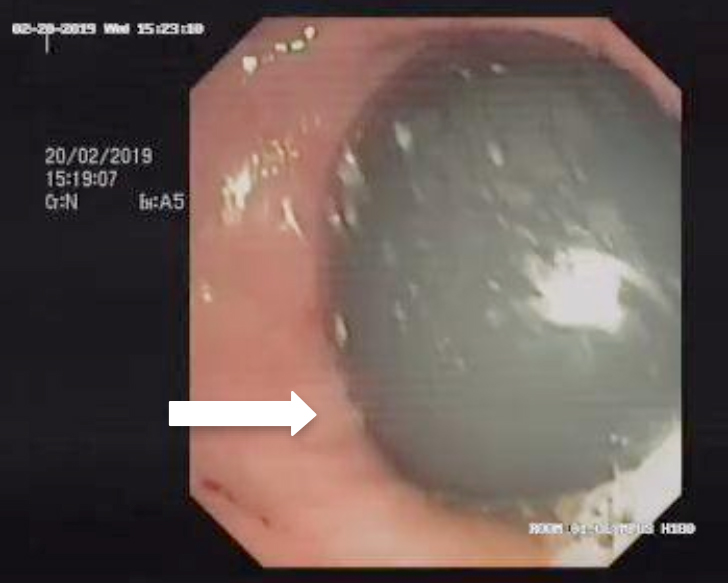 Figure 1: Arrow pointing to intra-gastric balloon.
Figure 1: Arrow pointing to intra-gastric balloon.
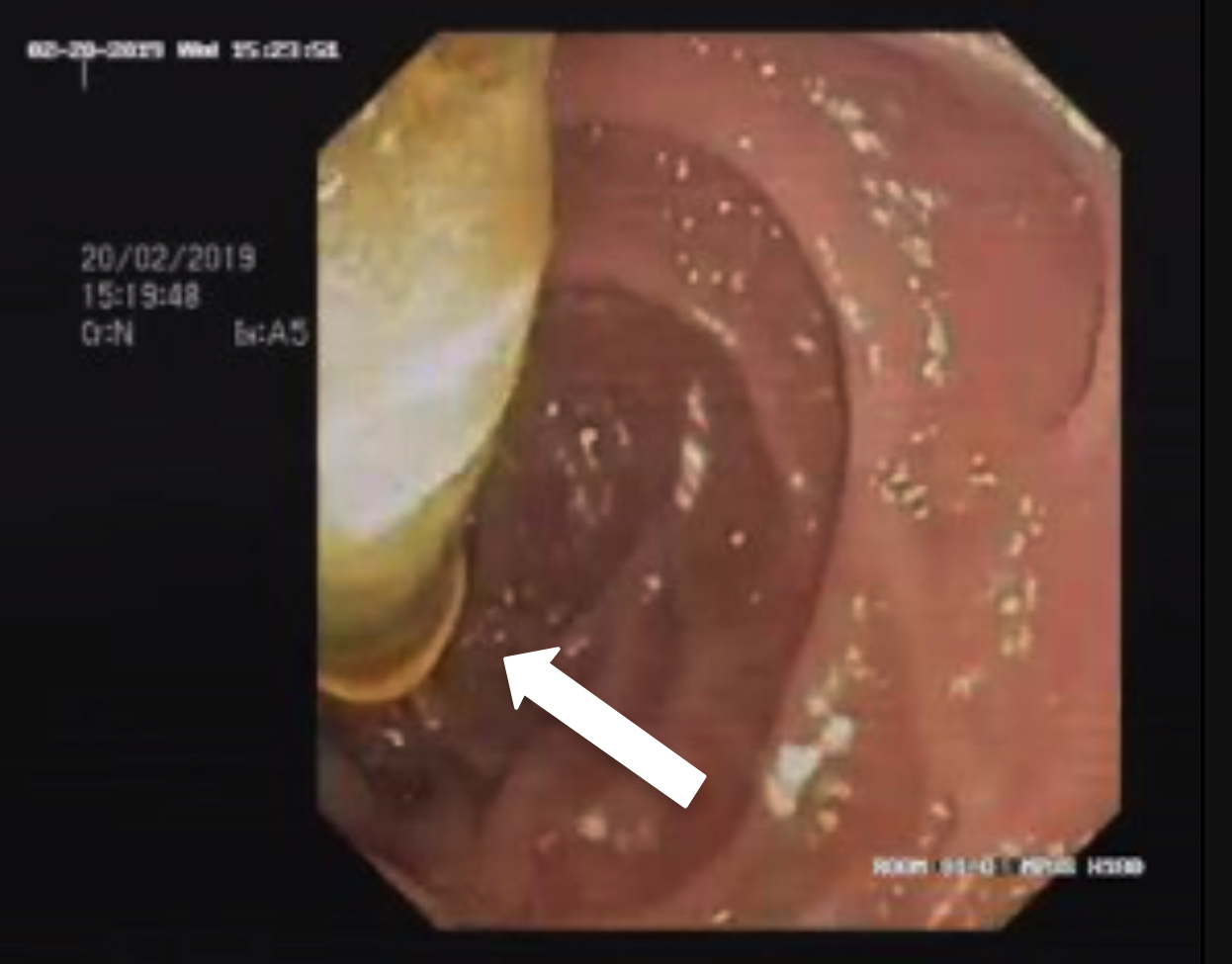 Figure 2: Arrow pointing to external pigtail catheter.
Figure 2: Arrow pointing to external pigtail catheter.
The position made the retrieval a difficult task, as the balloon was not being displaced from the antrum with multiple attempts made to dislodge it. Later, we used Rat Tooth Alligator Jaw Grasping forceps to grasp the external catheter and blue clasp, dragged into the stomach, and then, the balloon was successfully deflated and extracted from the lodged area, as shown in Figures 3 and 4.
Post-procedure recovery was uneventful and the patient was discharged home the same day. She was reassessed in the outpatient clinic later and reported no symptoms.
DISCUSSION
An individual with a BMI of 30 Kg/m2 or more is classified as obese whereas overweight is considered with a BMI of ≥25 g/m2.7 In the modern era, the first-line treatment for obesity is lifestyle modification with a properly balanced diet and increased exercise but its effects are however limited to fewer than 5% of the cases.8 This is where bariatric surgery comes into play with its long-term efficacy, but since it is an invasive procedure and is costly with reported surgical morbidity, it has not been accepted as a standard treatment.9
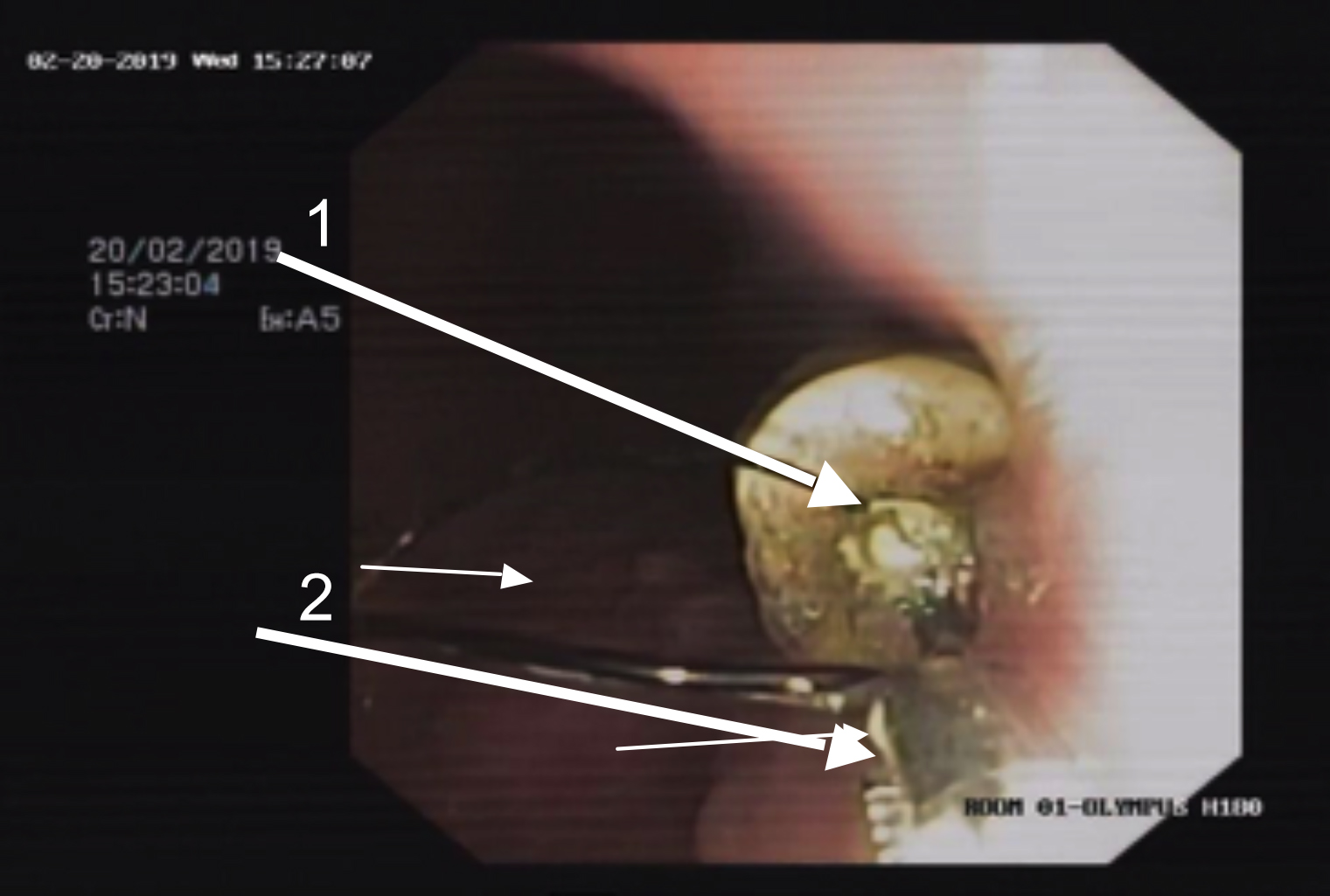 Figure 3: Arrow 1: External catheter and blue clasp, Arrow 2: Rat Tooth Alligator Jaw Grasping forcep.
Figure 3: Arrow 1: External catheter and blue clasp, Arrow 2: Rat Tooth Alligator Jaw Grasping forcep.
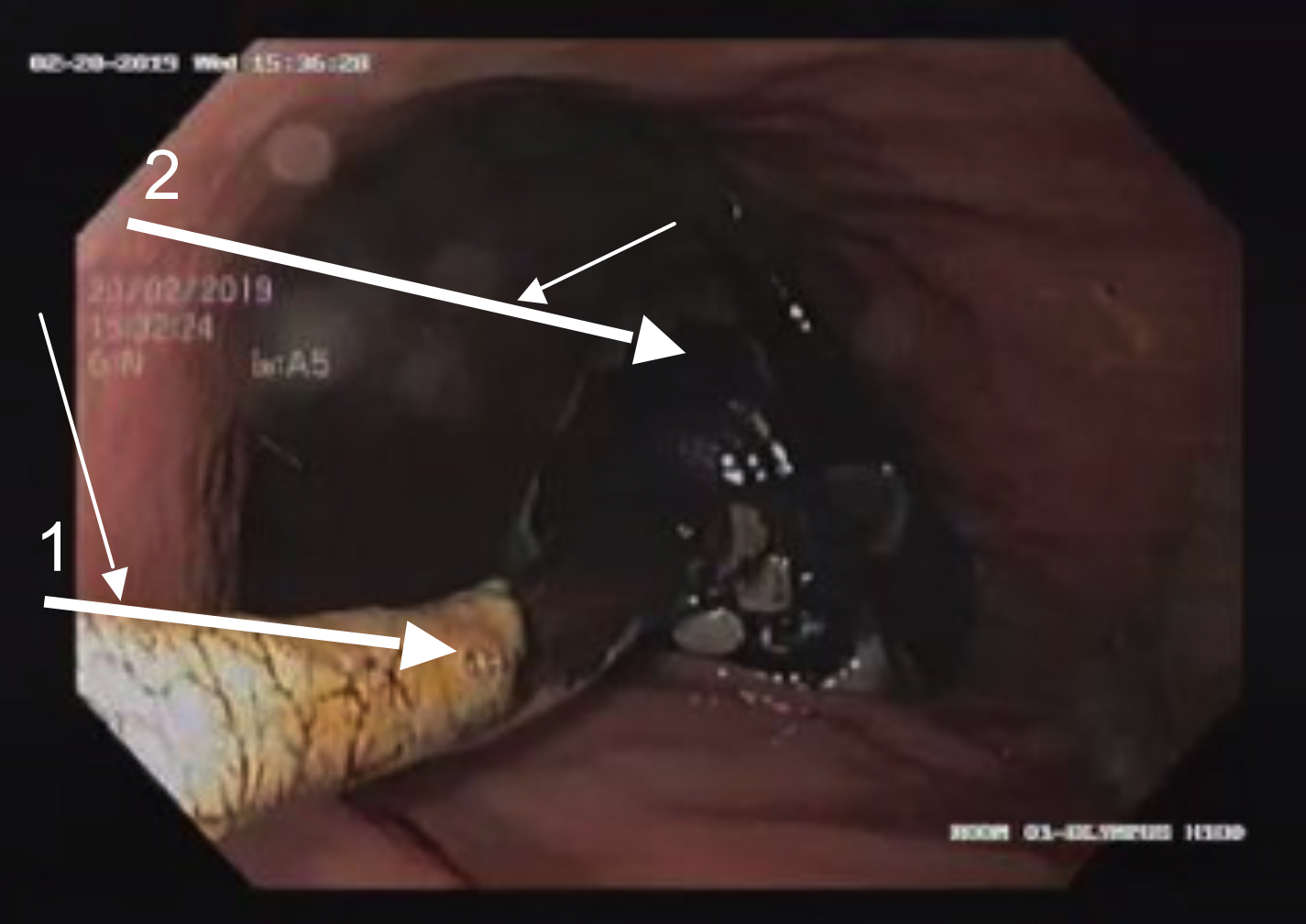 Figure 4: Arrow 1: external catheter, Arrow 2: Deflated intra-gastric balloon.
Figure 4: Arrow 1: external catheter, Arrow 2: Deflated intra-gastric balloon.
In this medical scenario, the only minimally invasive choice for obese patients is IGB placement. This is inserted endoscopically in the stomach where it decreases its capacity, delays gastric emptying, and promotes satiety.10 After these balloons are endoscopically inserted in the stomach, they are inflated with either air or saline and methylene blue. Post-procedure, within a few hours, the patient is discharged and then instructed to follow up in the outpatient clinic for the next 6-12 months, after which, the balloon is endoscopically removed.11
Common side effects of the procedure include abdominal pain (33.7% of patients), nausea (29%), and reflux (18.3%). Although rare, reported serious complications are visceral perforation (0.1%), postoperative bowel obstruction (0.3%) and death (0.08%).12 Balloon leaking was identified in 32 patients (0.54%) and balloon enlargement gas output was observed in 12 patients (0.20%); all complications were quickly detected and IGBs were replaced, helping patients to pursue care.12
In this case, we have reported the migration of the external pigtail catheter and blue clasp for retrieval of IGB into the duodenum and the silicon balloon portion of the IGB stuck at the antrum. Recently, a meta-analysis by the American Society for Gastrointestinal Endoscopy reported Orbera® balloon migration to be 1.4%, which is very rare.13 Balloon migration into the small intestine, potentially causing bowel obstruction, is a possible complication but antral obstruction, is considered a very rare IGB complication and very few have been reported in the literature.14
In conclusion, the presented case is of a safe removal of an impacted Spatz intIGB. Regular follow-up and adherence to manufacturer and physician guidelines are important tools for avoiding serious complications of IGB insertion.
PATIENT’S CONSENT:
Informed consent was obtained from the patient before being included in the case report.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
GM: Provided the concept, authored the manuscript, and proofread the final version before Submission.
RZ: Designed and authored the manuscript.
FB, NS: Contributed to analysis, acquisition, and revision.
All authors approved the final version of the manuscript to be published.
REFERENCES
- World Health Organisation. Factsheet: Obesity and overweight. 16th February 2018. www.who.int/news-room/ fact-sheets/detail/obesity-and-overweight. doi.org/10.1787/ a47d0cd2-en.
- Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American heart association task force on practice guidelines and the obesity society. J Am Coll Cardiol 2014; 63(25 Pt B): 2985-3023. doi.org/10.1161/01.cir.0000437739.71477.ee.
- Yumuk V, Tsigos C, Fried M, Schindler K, Busetto L, Micic D, et al. European guidelines for obesity management in adults. Obesity Facts 2015; 8(6):402-24. doi: 10.1159/0004 42721.
- Alsohaibani FI, Alkasab M, Abufarhaneh EH, Peedikayil MC, Aldekhayel MK, Zayied MM, et al. Acute pancreatitis as a complication of intragastric balloons: A case series. Obesity Surg 2019; 29(5):1694-6. doi.org/10.1007/s11695-019- 03796-6.
- Shahnazarian V, Ramai D, Sarkar A. Endoscopic bariatric therapies for treating obesity: A learning curve for gastroenterologists. Transl Gastroenterol Hepatol 2019; 4:16. doi.org/10.21037/tgh.2019.03.01.
- Papavramidis TS, Stavrou G, Papakostas P, Grosomanidis V, Kokkota S, Michalopoulos A, et al. Displacement of the intragastric balloon from the fundus to the antrum results in enhanced weight loss. Obesity Surg 2018; 28(8):2374-8. doi.org/10.1007/s11695-018-3168-1.
- NHLBI Expert panel on the identification and treatment of overweight and obesity in adults. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. Obes Res 1998; 6 Suppl 2:51S-209s. doi.org/10.1037/e565682010-001.
- Kumar N, Thompson CC. Endoscopic solutions for weight loss. Current Opinion Gastroenterol 2011; 27(5):407-11. doi.org/10.1097/mog.0b013e328349e240.
- Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev 2014; 2014(8):CD003641. doi.org/10.1002/14651858.cd003641.
- Zheng Y, Wang M, He S, Ji G. Short-term effects of intragastric balloon in association with conservative therapy on weight loss: A meta-analysis. J Transl Med 2015; 13:246-. doi.org/10.1186/s12967-015-0607-9.
- Al Shammari NM, Alshammari AS, Alkandari MA, Abdulsalam AJ. Migration of an intragastric balloon: A case report. Int J Surg Case Rep 2016; 27:10-2. doi.org/10. 1016/j.ijscr.2016.08.006.
- Yahia M, Najeh H, Zied H, Khalaf M, Salah AM, Sofienne BM, et al. Hayenne M. Wernicke's encephalopathy: A rare complication of hyperemesis gravidarum. Anaesthe Crit Care Pain Med 2015; 34(3):173-7. doi: 10.1016/j.accpm. 2014.09.005.
- Abu Dayyeh BK, Kumar N, Edmundowicz SA, Jonnalagadda S, Larsen M, Sullivan S, et al. ASGE bariatric endoscopy task force systematic review and meta-analysis assessing the ASGE PIVI thresholds for adopting endoscopic bariatric therapies. Gastrointestinal Endosc 2015; 82(3):425-38.e5. doi.org/10.1016/j.gie.2015.03.1964.
- Dumonceau J-M. Evidence-based review of the bioenterics intragastric balloon for weight loss. Obe Surg 2008; 18(12):1611-7. doi.org/10.1007/s11695-008-9593-9.