Hydrocele with Paratesticular Liposarcoma
By Ozer Baran, Ufuk Bozkurt, Aykut AykacAffiliations
doi: 10.29271/jcpsp.2022.04.1ABSTRACT
Paratesticular liposarcoma (PLS) is a rare type of genitourinary malignancy in the spermatic cord presenting as scrotal swelling. In this case study, we report an 82-year male who presented with prolonged left scrotal swelling and pain that did not respond to analgesic treatment for one week. His ultrasound confirmed increased fluid content in the left scrotal compartment in the form of septated hydrocele, and hydrocelectomy was planned. During the operation, infected fluid was drained. The testicle and surrounding tissues were infected; hence, left orchiectomy was performed. The pathological examination revealed a dedifferentiated liposarcoma. To our knowledge, this is the first report of liposarcoma of the spermatic cord with hydrocele in the literature.
Key Words: Liposarcoma, Spermatic cord, Scrotal swelling, Hydrocele.
INTRODUCTION
Lipomatous tumors account for approximately 35% of soft tissue tumors. It constitutes 5% of lipomatous tumors as reported by a study from Turkey.1 Liposarcomas are mostly observed in lower extremities (64%), trunk (20%), genitourinary area (12%), and upper extremity (10%).1 In the literature, approximately 200 paratesticular liposarcoma (PLS) cases have been reported so far.2 In this report, we aimed to present a case of concurrent hydrocele with PLS.
CASE REPORT
An 82-year male patient presented with a left scrotal swelling gradually increasing in six months; and left scrotal pain that did not respond to analgesic treatment and increased in severity for one week. On examination, the right testis could not be palpated and the left was approximately 15 cm in size. The patient’s medical history included right inguinal hernia and orchiectomy 20 years ago, coronary artery disease for 15 years, bypass surgery three years ago, ileus operation five years ago, and hemodialysis due to chronic renal failure for three years. The scrotal ultrasonography of the patient showed increased fluid content in the left scrotal compartment with a septated hydrocele, and the right testis could not be visualised. Hence, hydrocelectomy was performed.
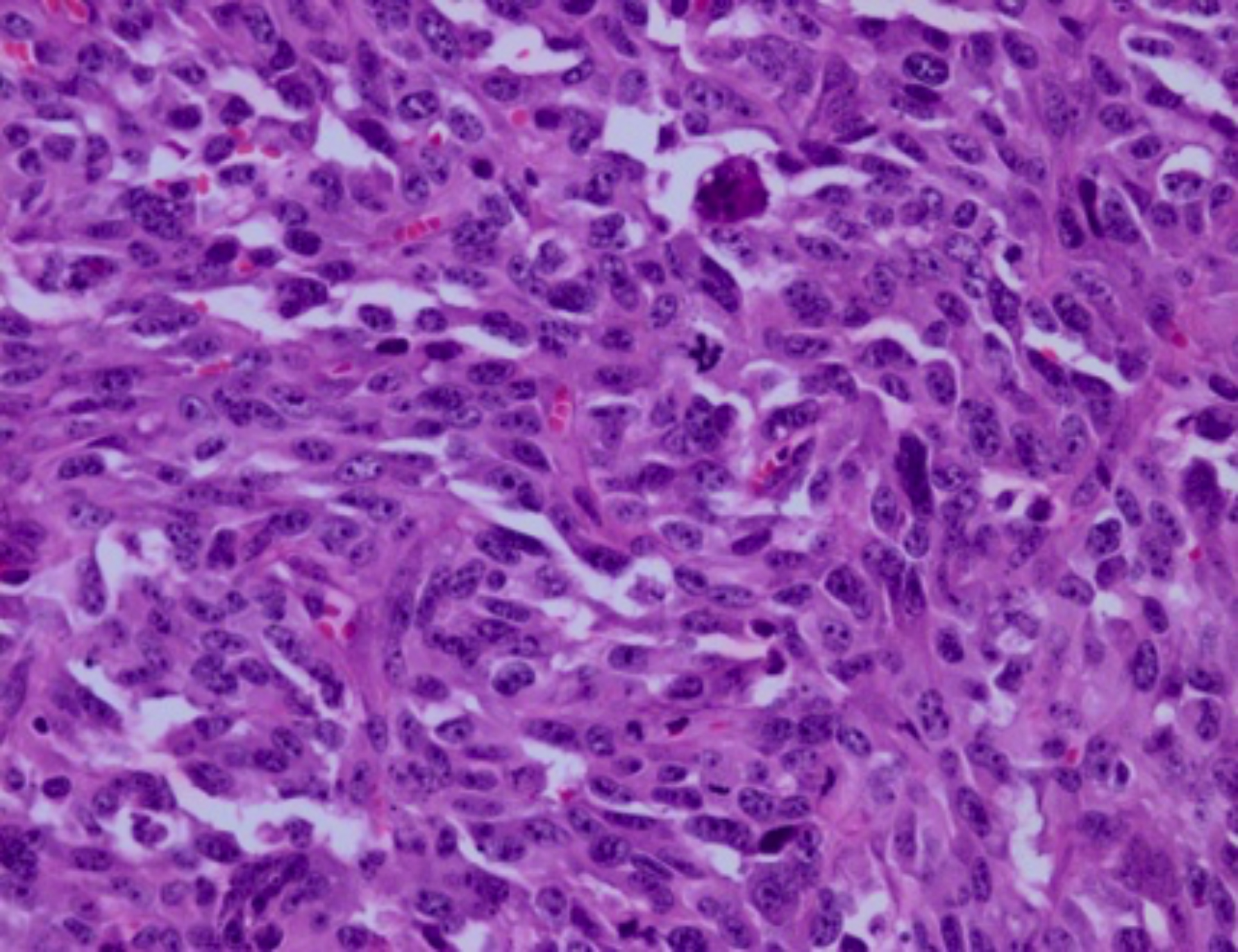 Figure 1: High-grade dedifferentiated portion of the tumor. Atypical mitoses are frequently seen in the tumor.
Figure 1: High-grade dedifferentiated portion of the tumor. Atypical mitoses are frequently seen in the tumor.
The infected fluid was drained when the tunica vaginalis was opened. The testis and surrounding tissues were heavily infected and left orchiectomy was performed considering the general condition of the patient. In the pathological examination, the left testicle size was 2.5×2.5×2 cm. A mass lesion was identified at 1.5 cm distance from the testis in the cord measuring 6.5×4×5 cm in size. The tumor was relatively well-circumscribed, partly solid (gray-white in appearance), partly cystic with necrotic and hemorrhagic areas. The sections from the mass lesion showed a tumor consisting of diffuse infiltration of atypical cells with abundant eosinophilic cytoplasm and large pleomorphic vesicular nuclei with prominent nucleoli. The tumor was not invading the testis and was located in the paratesticular region. Multiple binucleated and multinucleated bizarre cells and atypical mitoses were observed in the tumor (Figure 1). Mitoses were frequent. Myxoid degeneration, cells with hyperchromatic nuclei and atypical stromal cells were present in the surrounding fatty tissue. The tumor contained large areas of necrosis. In the tumor, a few scattered lipoblasts were also found (Figure 2). Immunohistochemical staining showed negativity of SMA, desmin, CD34, S-100, MYF-4, pancytokeratin; and positivity of vimentin. Ki-67 index was 50-60%. Microscopic and immunohistochemical findings were compatible with dedifferentiated liposarcoma. Radiotherapy was recommended after oncology consultation.
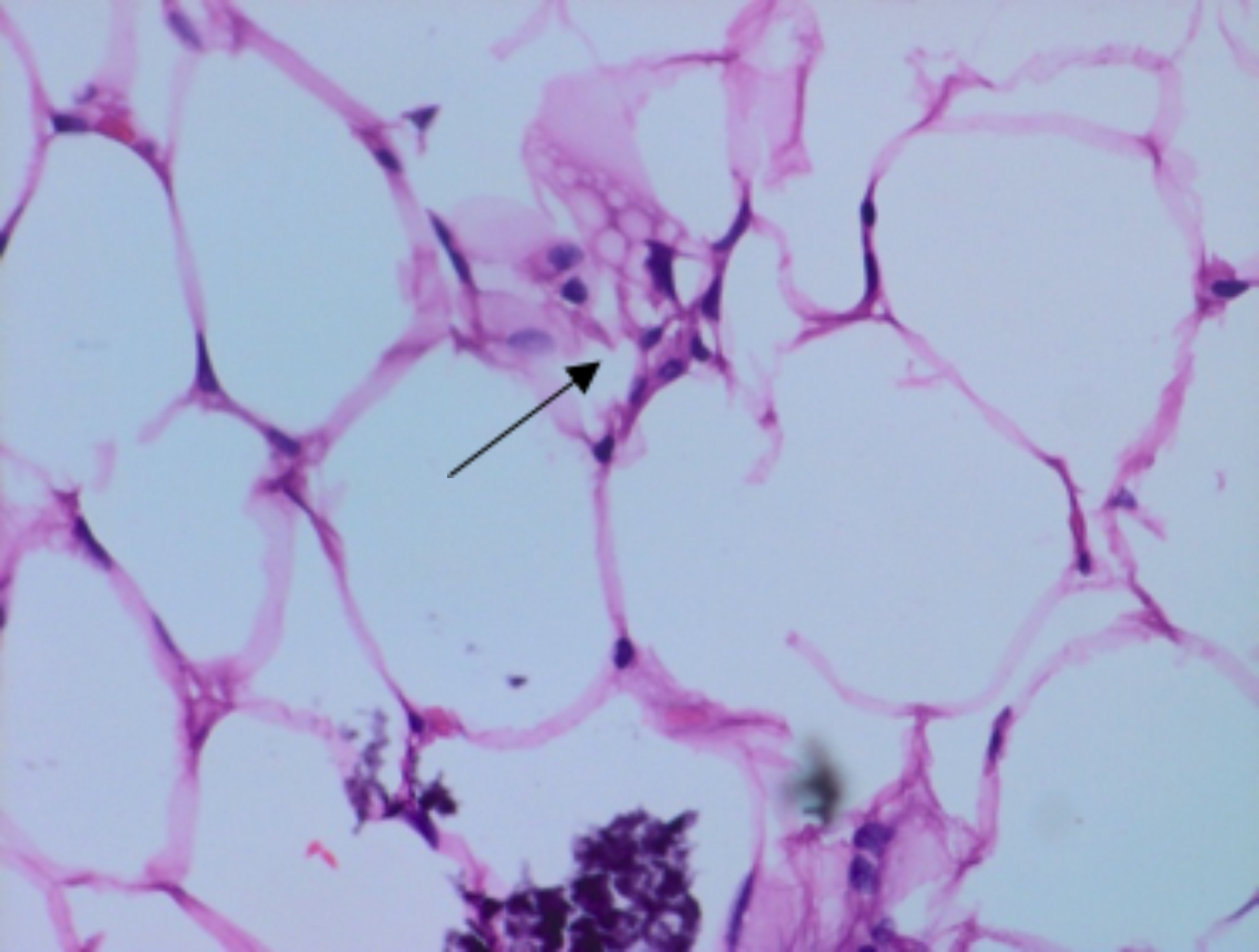 Figure 2: Typical lipoblast with scalloped nuclear outline in the tumor.
Figure 2: Typical lipoblast with scalloped nuclear outline in the tumor.
DISCUSSION
PLS usually presents as a painless, slowly developing inguinal or inguinoscrotal mass. Therefore, it may be misdiagnosed as scrotal lipoma, inguinal hernia and epididymitis.3 In this case, the patient presented with scrotal swelling, and the hydrocele was detected in the examination. The ultrasonography (USG) is sensitive for the detection of testicular masses. However, it may not be able to distinguish PLS from lipomas, if the tumor is small or PLS resembles lipoma and contains a homogenous fat pattern. MRI provides clear information about tumor focus.4
There are no data in the literature for the diagnosis and treatment of PLS. The standard treatment is considered to be radical orchiectomy and high ligation of the spermatic cord due to the possibility of high recurrence after inadequate excision.5 Adjuvant radiotherapy is required in all subtypes due to local residual lesions in one-third of PLS cases.6 Cerda et al. found no recurrence during the follow-up period of approximately 18 months in five patients with spermatic cord sarcoma who underwent radiotherapy.6
To our knowledge, this is the first case of PLS presenting with symptomatic hydrocele. Hydrocele is a common and benign disease seen as a fluid collection between the layers of tunica vaginalis. Our findings suggest that hydrocele may mask benign and malignant masses and should not deter from investigating for concurrent pathology in patients diagnosed with hydrocele. PLS is a rare and malignant tumor characterised by a slow growth that is often misdiagnosed preoperatively. Although it has been reported in the literature in patients operated for inguinal hernia and scrotal lipoma, it may be associated with hydrocele as in this case. USG, CT and MRI can be used for diagnosis, but the definitive diagnosis of PLS depends on histopathology and immunohistochemistry. When preoperatively diagnosed or suspected, wide local excision and radical orchiectomy with high ligation is the best treatment strategy and, if necessary, multimodal treatment can be applied. Long-term follow-up is recommended because of the risk of local recurrence and distant metastasis.
PATIENT’S CONSENT:
The patient’s informed consent was obtained for publishing this case report.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHOR’S CONTRIBUTION:
UB: Material, data collection and processing, writer.
OB: Concept, literature review, writer.
AA: Design, supervision, critical review.
REFERENCES
- Ustundag N, Dervişoglu S. Lipomatoz tumor serimizin dagılımı ve yeni tanımlanan lipomatoz tumorler. Cerrahpaşa J Med 2003; 34(3):119-26.
- Chiodini S, Luciani LG, Cai T, Molinari A, Morelli L, Cantaloni C, et al. Unusual case of locally advanced and metastatic paratesticular liposarcoma: A case report and review of the literature. Arch Ital Urol Androl 2015; 87(1):87-9. doi: 10.4081/aiua.2015.1.87.
- Fitzgerald S, Maclennan GT: Paratesticular liposarcoma. J Urol 2009; 181: 331‑2. doi: 10.1016/j.juro.2008.10.080.
- Schoonjans C, Servaes D, Bronckaers M: Liposarcoma scroti: A rare paratesticular tumor. Acta Chir Belg 2016; 116: 122‑5. doi: 10.1080/00015458.2016.1139939.
- Vukmirovic F, Zejnilovic N, Ivovic J: Liposarcoma of the paratesticular tissue and spermatic cord: A case report. Vojnosanit Pregl 2013; 70:693‑6. doi: 10.2298/vsp13 07695v.
- Cerda T, Martin É, Truc G, Créhange G, Maingon P. Safety and efficacy of intensity‑modulated radiotherapy in the management of spermatic cord sarcoma. Cancer Radiother 2017; 21: 16‑20. doi: 10.1016/j.canrad.2016. 07.102.