Extracorporeal Shock Wave Lithotripsy (ESWL) Outcome Based on CT Scan and Patient Parameters Using ESWL Score
By Yasir Rasheed1, Syed Muhammad Nazim1, Maheen Zakaria1, Muhammad Bin Nasir1, Sadia Khan2Affiliations
doi: 10.29271/jcpsp.2023.02.199ABSTRACT
Objective: To prospectively evaluate ESWL (extracorporeal shock wave lithotripsy) outcomes and validate ESWL Score.
Study Design: An observational study.
Place and Duration of Study: The Aga Khan University Hospital, from January 2021 to December 2021.
Methodology: Patients with symptomatic, solitary, radio-opaque renal stone measuring <15 mm with normal renal functions were included in this study. Stone size <11mm, BMI <27 Kg/m2, and stone density <900 Hounsfield units (HU) were all given 1 point each to give a total ESWL Score between 0-3 to each patient. Patients were evaluated after 4-weeks for the outcome i.e. stone clearance and complications.
Results: A total of 146 patients were included in the study. Median values for age, stone size, BMI and stone density were 40 years, 8 mm, 27 Kg/m2, and 774 HU respectively. Post ESWL, 99 (68%) patients were stone-free while 47 (32%) patients had residual stones. The stone clearance increased with the increasing score: 50% for ESWL score 0, 55.6% for ESWL score 1, 66.1% for ESWL score 2, and 85.7% for ESWL score 3 (p=0.01). The area under the curve (AUC) of ESWL score was 0.655 with 95 % CI (p=0.001).
Conclusion: ESWL Score is a useful predictor of the success of ESWL. It can help decide the individualised and appropriate modality of treatment and assist with patient counselling.
Key Words: Stone, Lithotripsy, Extracorporeal, Score, Shock wave, Outcome.
INTRODUCTION
Renal stones are one of the most common presentations in urological practice.1 They are an important health and economic issue due to high prevalence and recurrence rate.2,3 Pakistan is one of the countries with the highest stone disease burden.4 Treatment modalities evolved over the last few decades comprise various options including invasive, minimally invasive, and non-invasive techniques.
Extracorporeal Shock Wave Lithotripsy (ESWL) is one of the well-recognised non-invasive modalities for the treatment of urolithiasis. It is an outpatient non-invasive procedure performed to fragment urinary stones and is recommended for small to medium-sized renal stones.5,6
Despite recent advancement and success in minimally invasive endoscopic treatment modalities such as flexible ureteroscopy and mini percutaneous nephrolithotomy (PCNL), ESWL is still recommended in major urology guidelines such as the American Urology Association (AUA) and European Association of Urology (EAU) guidelines.7
Several factors influence the stone fragmentation and clearance, and the success rate of ESWL. These include patient-related factors such as body mass index (BMI), renal pelvicalyceal anatomy, and stone-related factors such as stone density and stone size.8
These factors have been studied individually to determine the success of ESWL, however, there is still a need for a better objective scoring system that could predict its outcomes. This will not only optimise the results of ESWL by appropriate patient selection but will also prevent unnecessary treatments.6
Recently, Bengió et al. proposed a scoring system, the ESWL score, based on multivariate analysis of three independent factors, namely BMI, stone size, and stone density in Hounsfield units (HU), to predict the outcome of lithotripsy.9 The score ranges from 0 to 3 in the ascending order of favourability for stone clearance. They found stone-free rates of 31.8% for score 0, 37.1% for score 1, 57.5% for score 2, and 88.3% for score 3. The area under the curve (AUC) for this score was 0.723 (p <0.001).9 However, this scoring system is yet to be validated by a well-designed prospective study. This study aimed to validate ESWL score to help in pragmatic implementation of this scoring system.
METHODOLOGY
This observational study was performed in the Section of Urology, The Aga Khan University Hospital after obtaining Ethical Review Committee Approval (ERC No. 2021 - 5319 - 15448). The study duration was one year from January 2021 to December 2021. The sample size was calculated on PASS 11 software. The minimum sample size was 139 patients with renal stones with an inflation of 10%, an anticipated area under the curve 0.85, level of significance of 5%, and power of 80%. All adult patients (18-65 years old) with solitary, symptomatic, radio-opaque renal stone measuring <15 mm with normal renal functions (serum creatinine <1.3 mg/dl) without any anatomical urinary tract abnormality or distal obstruction were included in this study. All patients had a negative urine culture prior to start of ESWL. Patients with pregnancy, uncorrected coagulopathy, morbid obesity (>130 Kg), staghorn calculus or any open, percutaneous or endoscopic intervention(s) were done prior to procedure (including placement of JJ stent and nephrostomy tube), and those lost to follow-up were excluded.
All patients underwent a detailed medical history, physical examination, and laboratory workup. Demographic data including age, gender, comorbid medical conditions, height, weight, and BMI were recorded before ESWL. Pre-procedure radiological evaluation included a non-contrast computed tomography (CT) was performed within two weeks of procedure on a 640-slice scanner using 3-mm axial and reformatted 3-mm coronal sections. The images were evaluated on a picture-archiving computer system (View Pro-X version 4.0.6.2; Rogan-Delft, Veenendaal, Holland). Stone-related parameters such as stone location and laterality were also noted. Stone density in Hounsfield units (HU) was calculated by mean attenuation of three consistent, non-overlapping regions of interest (area = 0.01 cm2) chosen over the stone in the bone window of the CT scan. Stone size was measured using the longest diameter in millimeters (mm). The skin–to stone distance (SSD) was calculated by measuring three distances from skin-to-stone at 0°, 45°, and 90° using radiological callipers and the average of these values was used to represent SSD for each stone. Subsequently, an ESWL score was calculated for each patient. The patient could have a score of 0, 1, 2 or 3 based on the number of favourable parameters i.e. BMI <27 Kg/m2, stone <11 mm and stone density <900 HU. The patient with no favourable parameter had a score 0 and the one with all parameters had score 3.
All patients underwent ESWL with the same protocol as an outpatient treatment. It was performed in lithotripsy suite on electromagnetic shock wave machine Siemens Modularis (Siemens AG, Medical Solutions, Erlangen, Germany). A single operator performed all procedures. With the patient in supine position, under sedo-analgesia, stones were localised using fluoroscopy with or without ultrasound guidance. Gradual ramping up of shock wave energy was done. The authors used a fixed frequency rate of 60 shocks/min. The number of shocks ranged between 2500-3500 per session. Patients’ vital signs, oxygen saturation and pain scores were monitored throughout the procedure. At the end of procedure, patients were discharged on analgesia and alpha-blocker, and were encouraged to drink plenty of fluids. Total number of sessions, number of shockwaves and the total energy used per patient were also calculated.
The stones were reassessed for fragmentation initially after 10-14 days and SWL session was repeated in case of inadequate fragmentation. Follow-up was done with an X-ray KUB (kidney, ureter and bladder) at 4-weeks from the last session of ESWL. The stone-free (SF) status was defined as no evidence of stone on imaging. Any complications post-ESWL was recorded according to the Clavien-Dindo Classification System.10 Need for any ancillary procedure like JJ stent insertion or uretero-renoscopy was also noted. The efficiency of ESWL was also recorded using efficiency quotient (EQ).
EQ = SFR/(100 +% re-treatment+ % ancillary procedure)
Data were analysed using SPSS version 22 (IBM SPSS statistics for Windows version 22.0 Armonk, NY; USA). Continuous variables were presented as means and standard deviation for normally distributed variables, and as median and interquartile range (IQR) for non-normally distributed variables. Normality was assessed using Shapiro-Wilk test. The variables were compared using Mann-Whitney U-test. Categorical variables were presented with numbers and percentages and compared using chi-square test. Univariate analysis associations were further explored using multivariate analysis. Various variables were compared between patients who were rendered stone-free with those with residual stones. To assess the predictive role of ESWL score, receiver operating characteristic (ROC) curve was generated and area under the curve (AUC) was determined. The value of p <0.05 was considered statistically significant.
RESULTS
During the study period, a total of 239 patients underwent ESWL at the setting, of which 146 patients fulfilled the criteria and were included in the final analysis. The median number of ESWL sessions was 2.0 (1-3), with the patients receiving a median number of 6000 shockwaves (IQR=1400; 2500-9000). A single session was required in 34.9 % of patients. The distribution of stones on both the right and left sides was nearly equal. Majority of stones were located in the renal pelvis (n=71, 48.6%) followed by the lower (n=31, 21.2%), middle (n=31, 21.2%), and upper calyces (n=13, 8.9%). Overall median age was 40 (IQR=22) years, while the median BMI was 27 (IQR=7) Kg/m2. Within the study population, 28.8% (n=42) of patients were overweight (25.1-30 Kg/m2), 31.5% (n=46) were obese (>30 Kg/m2), 36.3%(n=53) had normal BMI (18.5-25 Kg/m2), and only 3.4% (n=5) were underweight (<18.5 Kg/m2). The median stone size in this study population was 8 (IQR=5) mm, and ranged from 5 to 15 mm. The overall median stone density and skin-to-stone distance were 774 (IQR=662) HU and 125 (IQR=40) mm, respectively (Table I). The ranges for stone density and skin-to-stone distance were 176-1784 HU, and 69-195 mm, respectively. The overall median ESWL score in this study population was 2.
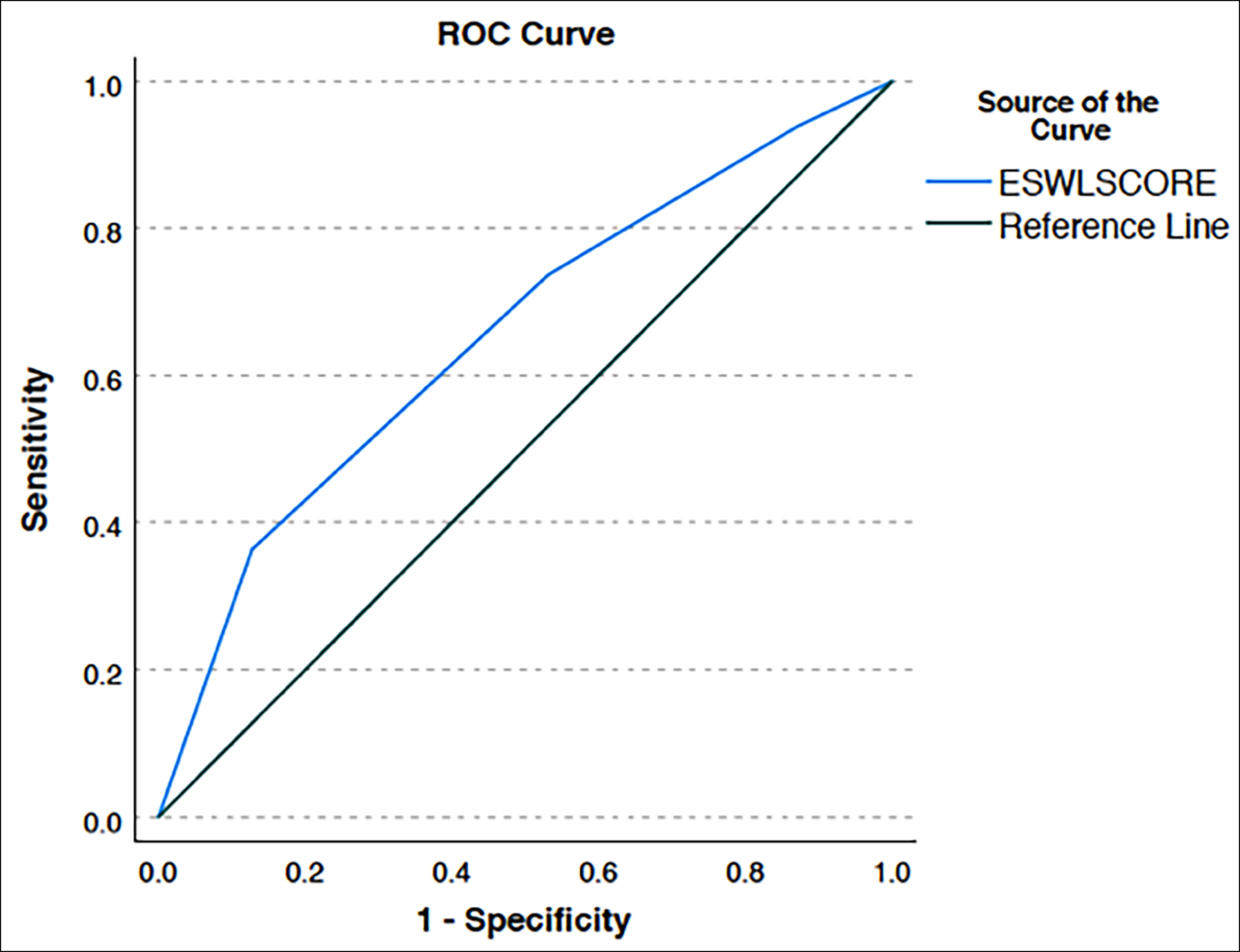 Figure 1: ROC curve for ESWL score.
Figure 1: ROC curve for ESWL score.
Of the 146 patients recruited in this study, 99 (68%) were ultimately stone-free post-ESWL, while 47 (32%) patients had residual stones. The authors did not find any difference in terms of age, gender, laterality, or stone distribution within the kidney. Stones in middle calyx achieved maximum clearance (25 out of 31, 80.6%), followed by renal pelvis (49 out of 71, 69%), lower calyx (18 out of 31, 58%) and upper calyx (7 out of 13, 54%). However, this difference was not statistically significant.
The outcome variables, which achieved statistical significance when comparing stone-free patients and patients with residual stone, were BMI and skin-to-stone distance (Table II). Other characteristics of interest were stone-size and stone density as these were utilised to compute the ESWL score, (range=0 to 3) per patient. However, for these variables, on comparison across clearance categories, no statistically significant difference was found in this study.
An assessment of the clearance status distribution for each ESWL score revealed that the percentage of patients with stone clearance post-ESWL increased with increasing score: 50% for ESWL score 0, 55.6% for ESWL score 1, 66.1% for ESWL score 2, and 85.7% for ESWL score 3. This difference was statistically significant (p=0.015, Table II).
The association between individual parameters and the clearance status was further explored on multivariate analysis; no individual parameter achieved statistical significance. The ESWL score as a whole was statistically significant (p = 0.015), and the AUC of ESWL score was 0.655 with 95% CI 0.562,0.747 (p=0.003) (Figure 1).
Overall complications were detected in 7.5% (n=11) patients. There was no significant difference in terms of complications between stone-free and residual stone groups. Majority of complications (63.6 %) were MCG grade 1-2. Two patients presented with post- ESWL colic requiring parenteral analgesia; however, none of them required inpatient admission. There were no cases of febrile UTI or urosepsis. Nine patients presented with steinstrasse (mainly for SWL done for larger size stones), of which five were managed conservatively and four required interventions. None of the patients developed significant haematuria with a drop in haemoglobin or perinephric hematoma. Eleven patients required ancillary treatment. (URS in 9 patients and PCNL in 2 patients).
The overall EQ for ESWL in this setting was 0.63. The EQ was 0.50 for ESWL score 0, 0.52 for score 1, 0.64 for score 2, and 0.85 for scores 3, respectively.
DISCUSSION
Among the multiple options available for the management of renal stones, ESWL is the one which has been used widely for the last 40 years. It is still considered as a first-line treatment option along with RIRS and PCNL for the treatment of renal stones in major urology guidelines such as the European Association of Urology (EAU) and American Urology Association (AUA). With recent advancements in endo-urological technology and intra-corporeal lithotripsy, the stone-free rates have become superior with endoscopic intervention as compared to ESWL. However, ESWL has the advantage of being a truly non-invasive and cost-efficient outpatient treatment option without the need for general anaesthesia which becomes one of the many reasons for it being a patient preference and choice of treatment modality. There is also a reduced need for a stent placement with this procedure as compared to endo-urological treatment options.
The success rate of ESWL has a wide variation ranging from 46% to 91% in contemporary series.11 This is related not only to the efficacy of lithotripsy machine but also to various patient and stone-related factors that influence stone fragmentation and clearance mentioned in different studies.6,8
A systematic review in 2018 by Yamashita et al. predicted that SSD, stone density and variation in stone density were independent predictors on NCCT for stone clearance via ESWL.12
Various authors have suggested different scoring systems by incorporating and combining these individual factors to improve patient selection for optimising the ESWL outcomes. ESWL score is one such attempt by Bengio et al., which was proposed after retrospective analysis of 114 patients who underwent ESWL.9 In this study, the authors have prospectively applied and validated this scoring system in the population. The overall stone-free rate in the patients undergoing ESWL was 67.8% consistent with the contemporary results. ESWL score was found to significantly predict the success of ESWL. This study population had an overall higher stone-free rate (67.8%) compared to the study by Bengio et al.
Table I: Evaluation of patients (n=146) and stone characteristics in both clearance status groups.|
Variable |
Overall (n=146) |
Clearance status |
p-value |
||
|
Free (n=99) |
Residual (n=47) |
||||
|
|
Median (IQR) |
|
|||
|
Age (years) |
40 (22) |
40 (25) |
41 (18) |
0.648 |
|
|
BMI (Kg/m2) |
27 (7) |
26 (8) |
29 (8) |
0.035* |
|
|
Stone size (mm) |
8 (5) |
8 (4) |
10 (4) |
0.059 |
|
|
Skin-to-Stone distance (mm) |
125 (40) |
122 (31) |
134 (47) |
0.034* |
|
|
Stone density (Hounsfield units) |
774 (662) |
704 (609) |
891 (708) |
0.076 |
|
|
Residual size (mm) |
– |
– |
6.0 (3.0) |
– |
|
|
|
|
Numbers (%) |
|
||
|
Gender |
Male |
98 (67.1) |
69 (70.5) |
29(29.5) |
0.352 |
|
Female |
48 (32.9) |
30(62.5) |
18(37.5) |
||
|
Site |
Left |
69 (47.3) |
47(68) |
22(32) |
>0.99 |
|
Right |
77 (52.7) |
52(67.5) |
25(32.5) |
||
|
Location |
Pelvis |
71 (48.6) |
49(69) |
22(31) |
0.180 |
|
Upper Calyx |
13 (8.9) |
7(54) |
6(46) |
||
|
Middle Calyx |
31 (21.2) |
25(80.6) |
6(19.4) |
||
|
Lower Calyx |
31 (21.2) |
18(58) |
13(41.9) |
||
|
*The authors have used chi-square test for categorical variables including Gender, site, and location, and Mann-Whitney U test for all other variables in this table. |
|||||
|
|
Clearance Status |
p-value |
||
|
Free (n=99) |
Residual (n=47) |
|||
|
ESWL score |
0 |
6 (50.0) |
6 (50.0) |
0.015* |
|
1 |
20 (55.6) |
16 (44.4) |
||
|
2 |
37 (66.1) |
19 (33.9) |
||
|
3 |
36 (85.7) |
6 (14.3) |
||
|
*Calculated using chi-square test with a significant p-value of <0.05. |
||||
The present definition of stone-free (SF) status was different. Bengio et al. used a cut-off of 4 mm residual stone size at 3 weeks follow-up for designating them a stone-free status. The authors used a much strict criterion of non-visualisation of any stone fragment at 4 weeks follow-up. Similarly, score wise, there was higher success for ESWL scores 0 (50%), 1 (55.6%), and 2 (66.1%), and 3 (85.7%) compared to Bengio et al. 0 (31.8%), 1 (37.1%), and 2 (57.5%), and 3 (88.3%) respectively. Although stone density and BMI were nearly similar in both studies, the mean stone size in this study was smaller (8.90 ± 3.09 mm) compared to 11.9 ± 5.4 mm in Bengio et al. Patients were younger (40.89 ± 14.13 years) compared to Bengio et al. study (50.02 ± 14.8 years). It is suggested that with increasing age, there is sclerotic change in renal parenchyma leading to increased acoustic impedance and poor stone fragmentation.13
The present study did not include patients with pre-operative JJ stent placement compared to 17.5% patients in Bengio et al. study. Pre-treatment insertion of JJ sent is recommended in larger renal stones (15-25 mm) to prevent steinstrasse and to lessen the need to visit the emergency department.14 Multiple studies have shown that JJ stenting does not seem to improve SFR. In-fact Hirsch et al. found that JJ stent may absorb shock waves and thus reduce the success of ESWL.15
Stone surface area and volumetric assessment of stone is found to be more useful to predict stone-free rate of ESWL for staghorn stones. Stone size measured at the largest stone diameter on CT scan has been found to be relatively easier and one of the important factors to measure ESWL outcome.16
Pareek et al. found significantly smaller mean BMI (26.9 ± 0.5 Kg/m2) in stone-free patients compared to patients with residual stones (30.8 ± 0.9 Kg/m2) for ESWL performed for renal stones between 5-10 mm.17 This study had findings similar to Pareek et al. Skin-to-stone distance (SSD) is also reported to be one of the predictors of treatment success for ESWL. Other studies have reported a cut-off values between of 10-11 cm.18,19
In some of the studies, SSD was found to have a better correlation than BMI due to different body types and fat distribution in different body regions.19 In the present study, the authors also found that the SSD was statistically significantly different between the two groups. The patients with lower SSD had better stone clearance in this study.
In this series, patients with ESWL scores 2 and 3 achieved stone-free rate of 66.1% and 85.7% respectively. Hence patients with these scores could be good candidates for ESWL. This can be communicated to the patients who often have the questions pertaining to the chances of success of a ESWL procedure. Tran et al. reported a ‘Triple D score’ by incorporating ‘D’istance (SSD), ‘D’ensity (HU) and stone ‘D’imension (volume). A triple D score 0, 1, 2 and 3 correlates successfully with ESWL in 21%, 41%, 78% and 96% of cases, respectively.20
Ichiyanagi et al. included additional parameter of stone location (‘D’istribution) to formulate a Quadruple- D scoring system with an additional score for non-lower pole region stones.21 Yoshioka et al. developed S3 HoCK score using initials of variables (size, SSD, sex, HU, colic and kidney or ureter).22
The authors believe that these scoring systems are too complex to calculate, require specialised software and are difficult to use in clinical practice. In this study, ESWL score was applied which includes parameters that had cut-offs established via multivariate regression analysis. The three parameters i.e. patients’ BMI, stone size, and HU used in ESWL score are not only simple to calculate but are also already available in patients’ records and radiology reports with no need for individual manual measurement in a busy outpatient clinic.
This score can help predict the outcome of ESWL and based on that, patients can be counselled about the chances of success of ESWL. Patients with a higher score have greater chances of stone clearance as compared to those with a lower score.
Therefore, it can help in shared decision-making regarding the choice of treatment modality between a patient and urologist can potentially lead to appropriate personalised treatment options for the patients. Patients will thus be better prepared to hear about outcomes and move to another modality of treatment, if needed after ESWL. This will have an economic impact too, as it can help in the timely application of other modalities for stone treatment.
To the authors knowledge, this is the first study of its kind validating ESWL score prospectively in Asian population to measure the outcome of ESWL. Most studies have used a follow-up duration of 3 months and stone size of <4 mm for rendering a stone-free status which could have over estimated their results. The authors used a strict definition of ‘no residual fragment’ as stone-free status and calculated it at 4 weeks follow-up. This timing for outcome evaluation may be too short for endpoint evaluation and may have overestimated the failure rate.
There are some limitations of this study. The stone composition was not examined in all patients. Compared to intravenous urography (IVU), some of the anatomical abnormalities such as ureteropelvic junction obstruction, narrow infundibulopelvic angle and stones in the calyceal diverticulum could not have been picked up in NCCT. There are inherent diagnostic limitations of a plain X-ray KUB for detecting residual stones, but the radiation and cost are the major factors for not using a CT scan in the follow-up. The cost of overall treatment was not calculated for the patients. Another limitation of this study was single centre-study design and small sample size. This scoring system has not been validated for ureteral stones, and the authors are not clear whether the findings of this study could be extrapolated to ureteral stones.
CONCLUSION
ESWL score is a useful predictor of success of ESWL. It can help decide the appropriate modality of treatment and assist with patient counselling. For a better assessment of its predictive capability, further evaluation of this score in a multicentre prospective study is warranted.
ETHICAL APPROVAL:
We performed this study after obtaining approval from ethical review committee (ERC) of Aga khan University Hospital, Karachi (ERC No. 2021-5319-15448).
PATIENTS’ CONSENT:
This was a prospective observational study with no direct contact with patients and no change in management plan of patients hence requirement for consent for exempted by ERC.
COMPETING INTEREST:
This study is not funded and there is no competing interest to declare.
AUTHORS’ CONTRIBUTION:
YR: Design of the work, acquisition, analysis and interpretation of data, and manuscript writing.
SMN: Design of the work, interpretation of data, and manuscript writing.
MZ, MBN: Acquisition and analysis of data, and manuscript writing.
SK: Acquisition of data.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Watson G, Payne SR, Kunitsky K, Natchagande G, Mabedi C, Scotland KB. Stone disease in low- and middle-income countries: Could augmented reality have a role in its management? BJU Int 2022; 130(4):400-7. doi: 10.1111/bju.15877.
- Kim MM, Harvey J, Gusev A, Norton JM, Miran S, Bavendam T. A scoping review of the economic burden of non-cancerous genitourinary conditions. Urology 2022; 166: 29-38. doi: 10.1016/j.urology.2021.10.008.
- Hyams ES, Matlaga BR. Economic impact of urinary stones. Transl Androl Urol 2014; 3(3):278-83. doi: 10.3978/j.issn. 2223-4683.2014.07.02.
- Memon A. Epidemiology of stone disease in Pakistan. In: Talati J, Tiselius HG, Albala DM, et al.editors. Urolithiasis: basic science and clinical practice, vol. 1: epidemiology. London: Springer; 2012. p. 21–38.
- Shafi H, Moazzami B, Pourghasem M, Kasaeian A. An overview of treatment options for urinary stones. Caspian J Intern Med 2016; 7(1):1-6.
- Petrides N, Ismail S, Anjum F, Sriprasad S. How to maximize the efficacy of shockwave lithotripsy. Turk J Urol 2020; 46 (Suppl. 1):S19-26. doi: 10.5152/tud.2020.20441.
- Quhal F, Seitz C. Guideline of the guidelines: Urolithiasis. Curr Opin Urol 2021; 31(2):125-9. doi: 10.1097/MOU.000 0000000000855.
- Shinde S, Al Balushi Y, Hossny M, Jose S, Al Busaidy S. Factors affecting the outcome of extracorporeal shockwave lithotripsy in urinary stone treatment. Oman Med J 2018; 33(3):209-17. doi: 10.5001/omj.2018.39.
- Bengió RG, Arribillaga L, Epelde J, Orellana S, GarcIa-onto H, Montedoro A, et al. Sistema predictivo de éxito adaptado a nuestro medio para mejorar los resultados de la Litotricia extracorpórea predictive score of success adapted to our environment to improve results of extracorporeal lithotripsy. PMID: 27617549.
- Mittal V, Srivastava A, Kappor R, Ansari MS, Patidar N, Arora S et al. StandardiZed Grading of shock wave lithotripsy complications with modified clavien system. Urol Int 2016; 97(3):273-8. doi: 10.1159/000446968.
- Laksita TB, Soebadi MA, Wirjopranoto S, Hidayatullah F, Kloping YP, Rizaldi F. Local anesthetics versus systemic analgesics for reducing pain during extracorporeal shock wave lithotripsy (ESWL): A systematic review and meta-analysis. Turk J Urol 2021; 47(4):270-278. doi: 10.5152/tju.2021. 21143.
- Yamashita S, Kohjimoto Y, Iwahashi Y, Iguchi T, Nishizawa S, Kikkawa K, et al. Noncontrast computed tomography parameters for predicting shock wave lithotripsy outcome in upper urinary tract stone cases. Biomed Res Int 2018; 2018: 9253952. doi: 10.1155/2018/9253952.
- Ng CF. The effect of age on outcomes in patients undergoing treatment for renal stones. Curr Opin Urol 2009; 19(2):211-4. doi: 10.1097/mou.0b013e32831e16b7.
- Yazici O, Kafkasli A, Erbin A, Bilal Hamarat M, Cubuk A, Sarilar O, et al. Effect of JJ stent on outcomes of extracorporeal shock wave lithotripsy treatment of moderate sized renal pelvic stones: A randomized prospective study. Actas Urol Esp (Engl Ed). 2019; 43(8):425-30. English, Spanish. doi: 10.1016/j.acuro.2019.03.009.
- Hirsch B, Abt D, Güsewell S, Langenauer J, Betschart P, Pratsinis M et al.Outcome groups and a practical tool to predict success of shock wave lithotripsy in daily clinical routine. World J Urol 2021; 39(3):943-51. doi: 10.1007/ s00345-020-03253-5.
- Buchholz NP, Rhabar MH, Talati J. Is measurement of stone surface area necessary for SWL treatment of nonstaghorn calculi? J Endourol 2002; 16(4):215-20. doi: 10.1089/08927 7902753752151.
- Pareek G, Armenakas NA, Panagopoulos G, Bruno JJ, Fracchia JA. Extracorporeal shock wave lithotripsy success based on body mass index and Hounsfield units. Urology 2005; 65(1):33-6. doi: 10.1016/j.urology.2004.08.004.
- Park BH, Choi H, Kim JB, Chang YS. Analyzing the effect of distance from skin to stone by computed tomography scan on the extracorporeal shock wave lithotripsy stone-free rate of renal stones. Korean J Urol 2012; 53(1):40-3. doi: 10.4111/ kju.2012.53.1.40.
- Cho KS, Jung HD, Ham WS, Chung DY, Kang YJ, Jang WS et al. Optimal skin-to-stone distance is a positive predictor for successful outcomes in upper ureter calculi following extracorporeal shock wave lithotripsy: A bayesian model averaging approach. PLoS One 2015; 10(12):e0144912. doi: 10.1371/journal.pone.0144912.
- Tran TY, McGillen K, Cone EB, Pareek G. Triple D score is a reportable predictor of shockwave lithotripsy stone-free rates. J Endourol. 2015; 29(2):226-30. doi: 10.1089/end. 2014.0212.
- Ichiyanagi O, Fukuhara H, Kurokawa M, Izumi T, Suzuki H, Naito S, et al. Reinforcement of the triple D score with simple addition of the intrarenal location for the prediction of the stone-free rate after shockwave lithotripsy for renal stones 10-20 mm in diameter. Int Urol Nephrol 2019; 51(2):239-245. doi: 10.1007/s11255-018-02066-1.
- Yoshioka T, Ikenoue T, Hashimoto H, Otsuki H, Oeda T, Ishito N, et al. Okayama-Ehime S.W.L. Study group. Development and validation of a prediction model for failed shockwave lithotripsy of upper urinary tract calculi using computed tomography information: the S3HoCKwave score. World J Urol 2020; 38(12):3267-73. doi: 10.1007/s00345- 020-03125-y.