Evaluation of the Effect of Interscalene Brachial Plexus Block on Intracranial Pressure Using Optic Nerve Sheath Diameter and Internal Jugular vein Collapsibility Index
By Oguz Gundogdu, Onur AvciAffiliations
doi: 10.29271/jcpsp.2022.10.1249ABSTRACT
Objective: To determine the effect of single-shot interscalene brachial plexus (ISBP) block on intracranial pressure (ICP) by evaluating the extravascular volume effect of the medicine on the internal jugular vein (IJV).
Study Design: Interventional study.
Place and Duration of Study: Department of Anaesthesiology and Reanimation, Sivas Cumhuriyet University, Sivas, Turkey, from January to June 2022.
Methodology: Thirty-four patients were included in this prospective clinical study. All patients had single-shot ISBP block with 25 ml of local anaesthetic. Optic nerve sheath diameter (ONSD), maximum (Dmax) and minimum (Dmin) diameters of IJV and IJV collapsibility index (IJV-CI) were recorded before the block (basal), 20 minutes, and 60 minutes after the block.
Results: Twenty-nine patients had higher ONSD values at 60th minute compared to their basal values. There were negative correlations between the changes of ONSD and IJVCI (r=0.616, p<0.001) and ONSD and Dmax (r=0.581, p<0.001) in time period between basal and 20th minute. There were negative correlations between the changes of ONSD and IJVCI (r=0.518, p=0.002), ONSD and Dmax (r=0.664, p<0.001) in time period between basal and 60th minute.
Conclusion: Single-shot ISBP block with 25 ml of local anaesthetic may be a factor that increases ICP. Repeated intraoperative ONSD measurements are recommended in patients operated with ISBP block.
Key Words: Interscalene Brachial Plexus Block, Intracranial pressure, Optic nerve sheath diameter, Internal jugular vein collapsibility index.
INTRODUCTION
The interscalene brachial plexus (ISBP) block is the most preferred method of block to provide anaesthesia and analgesia in humerus and shoulder surgeries. Although, it provides great analgesia in the shoulder and humerus region, it may cause complications such as ipsilateral phrenic nerve block, hoarseness and horner syndrome. The effect of ISBP block on intracranial pressure (ICP) is unknown, but it has recently been shown to increase cerebral oxygenation.1
ONSD is a popular, non-invasive measurement technique that provides information about ICP. Although, a specific and exact cut-off value has not been established, studies have generally accepted 5 millimetres (mm) as the upper limit of ONSD measurement.2,3
Kimberly and colleagues systematically confirmed that the 5-mm threshold in ONSD reflects ICP above 20 mmHg.3 In another study, the optimal ONSD limit for determining ICP above 20 mmHg was found to be ≥5.0 mm with 94% sensitivity and 98% specificity.2
In patients without intracranial pathology, ICP may be affected by mean arterial pressure (MAP), hypothermia, fluid imbalance, electrolyte imbalance, patient position, etc.4-6 The internal jugular vein collapsibility index (IJV-CI) indicates the actual intravascular volume status of the IJV. The reason for using IJV-CI in this study is to demonstrate the relationship between the change in IJV-CI and the change in ONSD due to the extravascular drug-volume effect.
The aim of this study was to determine the effect of single-shot ISBP block with 25 ml local anaesthetic on ICP by evaluating the extravascular volume effect of the agent on the IJV.
METHODOLOGY
This prospective, single-centre, clinical Interventional study was conducted at Sivas Cumhuriyet University, Sivas, Turkey, from January to June 2022. The study included 34 adult patients aged 18-70 years, ASA I-II according to the American Society of Anaesthesiologists (ASA) risk classification, undergoing elective humeral fracture and open rotator-cuff repair surgery with interscalene block. Detailed information about interscalene block, ONSD measurement, and IJV-CI measurements were given to the patients verbally and in writing before the procedure. Written informed consent were obtained from all participating patients. The study was approved by the Ethics Committee of Sivas Cumhuriyet University (date: 21/12/2021 and issue: 2021-12/01).
Subjects who did not consent to the study, had infection and open wounds on the skin puncture site and eyelids, had any intracranial pathology in the history, had contraindications for nerve blockade such as coagulation disorder and antithrombotic-anticoagulant therapy, were excluded. Other exclusion criteria were: History of allergy to any of the injected agents, body mass index (BMI) over 35 Kg/m2, contralateral pneumothorax, severe respiratory distress, operated under emergency conditions, uncontrolled hypertension, acute or chronic eye disease, previous eye surgery and beta-blocker, calcium channel blockers, statins and nitrates use. Patients requiring intraoperative sedation who developed any complications (hoarseness, horner's syndrome, respiratory distress, and local anaesthetic toxicity) due to ISBP block were also excluded.
The age and gender of all patients were recorded. Patients were monitored including electrocardiography, invasive radial artery cannulation, and pulse oximetry. All patients received peripheral intravenous access to the non-procedured arm and volume replacement with crystalloid solution in standard dose of 6-8 ml/kg/hour was performed. Urinary catheterisation was performed by the surgical team in all patients before the start of surgery.
For single shot-ISBP block in all patients, 15 ml 0.5% bupivacaine+10 ml 2% prilocaine dose of local anaesthetic was administered for a total of 25 ml. Patients were positioned in a 45-degree head-up position with their faces approximately 45 degrees opposite to the direction of the procedure. For the block procedure, following an imaginary horizontal line drawn from the thyroid cartilage to the sternocleidomastoid (SCM) muscle, at the site of injection, the lateral aspect of the SCM muscle was cleaned with povidone-iodine. A portable ultrasound device and a 6-10 MHz linear probe were used for the block. The nerve roots were identified at the level of C6 to be blocked, 22 G 80 mm echogenic needle was inserted and injected around the plexus roots and the distribution of the local anaesthetic that dilates the tissues and separates the nerve roots from other tissues was monitored by ultrasound. Motor block was confirmed by the absence of abduction movement in the arm and sensory block was confirmed by a pin-prick test.
The IJV-CI was measured with the same ultrasound linear probe placed on the IJV and the distance between the widest measurement of the vessel diameter (Dmax) and the narrowest measurement distance (Dmin) was recorded during the change in IJV diameter during one spontaneous breathing cycle. Measurements of the IJV were made only on the IJV on the side of the block. These measurements were recorded by calculating IJV-CI using the following formula:
IJV‑ Collapsibility index (CI) = ([Dmax – Dmin]/Dmax) × 100%
For ONSD measurement, the transducer was placed on the eyelids taking care not to apply pressure. Two measurements were made for each optic nerve: One was the sagittal plane with the transducer placed vertically and the other was the transverse plane with the transducer placed horizontally. The ONSD perpendicular to this axis was measured by moving 3 mm away from the posterior of the optic globe in the longitudinal axis. The final ONSD is the average of these 4 measurements.
Heart rate (HR), MAP, ONSD value, IJV-CI value were recorded before (baseline), 20 and 60 minutes after the interscalene block. All blocks were performed by the same anesthesiologist. Recording of all data was performed by another anaesthesiologist. All measurements and surgery were performed in the same patient position (45 degrees head up, beach-chair).
Statistical analyses were performed with SPSS version 25.0 program. The conformity of the variables to normal distribution was analysed by histogram plots and Kolmogorov-Smirnov test. Mean, standard deviation, median, and min-max values were used to present descriptive analyses. The categorical variables were expressed as numbers and percentages. Basal-20 min differences and Basal-60 min differences in measured values were analysed by Spearman Correlation Analysis. The p-values below 0.05 were considered as statistically significant results.
RESULTS
For the study, 40 patients underwent ISBP block. Of these, 6 patients were excluded from the study (3 due to horner syndrome and 3 due to failed block). No complications related to ISBP block were observed in the remaining 34 patients. A total of 34 patients, 16 (47%) females and 18 (53%) males, aged between 21 and 84 years, were included in the study. Of these, 19 (55.8%) patients underwent surgery on the right and 15 (44.2%) on the left side. In 19 (55.8%) patients the type of surgery was humeral fracture and in 15 (44.2%) patients rotator-cuff repair surgery. Mean age of the patients: 50, 18±16, 06 years. The mean values of ONSD, IJV-CI, Dmax, Dmin, HR and MAP measured at baseline, 20th minute and 60th minute are given in Table I.
Basal-20th minute differences of ONSD, IJVCI, Dmax, Dmin, HR and MAP values were calculated and their correlations with each other were analysed. Accordingly, there were negative correlations between ONSD and IJVCI (r=0.616, p<0.001) and ONSD and Dmax (r=0.581, p<0.001), positive correlations between IJVCI and Dmax (r=0.607, p<0.001), and negative correlations between IJVCI and Dmin (r=0.455, p=0.007, Table II).
Table I: Mean values of ultrasonographic measurements and vital signs at different times.|
|
Basal |
20th minute |
60th minute |
|||
|
Mean±SD |
Median (min-max) |
Mean±SD |
Median (min-max) |
Mean±SD |
Median (min-max) |
|
|
ONSD (mm) |
4.33±0.42 |
4.28 (3.55-5.45) |
4.67±0.48 |
4.65 (3.85-5.85) |
5.08±0.64 |
5 (4.15-6.5) |
|
IJVCI (%) |
24.18±9.02 |
22 (12-61) |
19.94±7.27 |
18.5 (9-42) |
18.74±7.66 |
17.5 (8-45) |
|
Dmax (mm) |
4.94±2.47 |
3.95 (2.5-13) |
4.46±1.94 |
3.75 (2.3-9.9) |
4.13±1.86 |
3.5 (2-9.4) |
|
Dmin (mm) |
3.61±1.52 |
3 (1.8-7.4) |
3.56±1.59 |
2.8 (1.9-7.6) |
3.34±1.53 |
2.75 (1.6-7.5) |
|
HR (/minute) |
70.68±9.94 |
70 (52-90) |
69.71±9.73 |
70 (52-88) |
69.35±10.18 |
68 (53-90) |
|
MAP (mmHg) |
84.94±5.07 |
86 (74-93) |
84.85±5.11 |
85 (72-93) |
84.44±4.31 |
84 (74-93) |
|
ONSD: Optic nerve sheath diameter; IJVCI: Internal jugular vein collapsibility index; Dmax: Maximum diameter of internal jugular vein; Dmin: Minimum diameter of internal jugular vein; HR: Heart rate; MAP: Mean arterial pressure; SD: Standard deviation; mm: Millimetre; mmHg: Millimetre mercury. |
||||||
Table II: The correlation of the changes of ultrasonographic measurements and vital signs, between basal and 20th minute, and basal and 60th minute.
|
Basal-20th minute |
ONSD |
IJVCI |
Dmax |
Dmin |
HR |
|
|
ONSD |
r |
|
|
|
|
|
|
p |
|
|
|
|
|
|
|
IJVCI |
r |
-0.616 |
|
|
|
|
|
p |
<0.001 |
|
|
|
|
|
|
Dmax |
r |
-0.581 |
0.607 |
|
|
|
|
p |
<0.001 |
<0.001 |
|
|
|
|
|
Dmin |
r |
0.140 |
-0.455 |
0.136 |
|
|
|
p |
0.430 |
0.007 |
0.442 |
|
|
|
|
HR |
r |
-0.238 |
0.219 |
0.231 |
-0.166 |
|
|
p |
0.175 |
0.213 |
0.188 |
0.349 |
|
|
|
MAP |
r |
0.124 |
-0.194 |
-0.167 |
0.024 |
-0.169 |
|
p |
0.485 |
0.272 |
0.344 |
0.892 |
0.339 |
|
|
Basal-60th minute |
ONSD |
IJVCI |
Dmax |
Dmin |
HR |
|
|
ONSD |
r |
|
|
|
|
|
|
p |
|
|
|
|
|
|
|
IJVCI |
r |
-0.518 |
|
|
|
|
|
p |
0.002 |
|
|
|
|
|
|
Dmax |
r |
-0.664 |
0.568 |
|
|
|
|
p |
<0.001 |
<0.001 |
|
|
|
|
|
Dmin |
r |
-0.338 |
-0.098 |
0.571 |
|
|
|
p |
0.050 |
0.580 |
<0.001 |
|
|
|
|
HR |
r |
-0.350 |
0.092 |
0.205 |
0.122 |
|
|
p |
0.042 |
0.603 |
0.245 |
0.493 |
|
|
|
MAP |
r |
0.129 |
-0.181 |
-0.257 |
-0.087 |
-0.436 |
|
p |
0.467 |
0.306 |
0.142 |
0.625 |
0.010 |
|
|
Spearman correlation test was used p<0.05: Statistically significant; ONSD: Optic nerve sheath diameter; IJVCI: İnternal jugular vein collapsibility index; |
||||||
The correlation between the changes in ONSD, IJV-CI and Dmax values between baseline and 20 minutes are shown in Figure 1.
Basal-60th min differences of ONSD, IJVCI, Dmax, Dmin, HR, and MAP values were calculated and their correlations with each other were analysed. Accordingly, ONSD and IJVCI (r=0.518, p=0.002), ONSD and Dmax (r=0.664, p<0.001) and ONSD and HR (r=0.350, p=0.042) were negatively correlated, IJVCI and Dmax (r=0.568, p<0. 001), Dmax and Dmin (r=0.571, p<0.001) were positively correlated, and HR and MAP (r=0.436, p=0.010) were negatively correlated (Table II). The correlation between the changes in ONSD, IJV-CI and Dmax values between baseline and 60 minutes are shown in Figure 2.
In 4 patients, ONSD measurements minimally decreased at 60th minute compared to baseline. In one patient, there was no change in ONSD measurements at 60th minute compared to baseline.
ONSD measurements of 9 patients were in the range of 5.0-5.5 mm. ONSD measurements of 2 patients reached the range of 5.5-6.0 mm. Two patients had ONSD values in the range of 6.0-6.5 mm. Patients with ONSD measurements in the range of 5.0-6.0 mm did not have any symptoms related to increased ICP.
DISCUSSION
In this study, the effect of ISBP block on ICP was investigated for the first time to the authors’ knowledge in the literature. Another unique feature of the study is that it was performed on patients who did not receive any other medical treatment that may affect ICP such as general anaesthesia. The most important result of the study was that the Dmax of IJV decreased and ICP increased with the volume effect of 25 ml of the drug. The fact that ICP increased independently of MAP in 29 of 34 patients who received standard fluid replacement may be explained by the external compression of the IJV by the 25 ml drug.
There may be other factors that affect ICP intraoperatively, such as i.v. anaesthetics, volatile anaesthetics, mechanical ventilation, amount of bleeding, and certain patient positions during surgery.7 In this study, all patients were in the beach-chair position during measurements and block application, and patients receiving i.v. sedative agents and general anaesthesia were not included in the study. Therefore, this anaesthetic approach is much more suitable to investigate the effect of ISBP block on ICP other than general anaesthesia.
 Figure 1: The correlation between ONSD and IJV-CI in terms of change in values measured at basal and 20th minute and the correlation between ONSD and Dmax in terms of change in values measured at basal and 20th minute.
Figure 1: The correlation between ONSD and IJV-CI in terms of change in values measured at basal and 20th minute and the correlation between ONSD and Dmax in terms of change in values measured at basal and 20th minute.
IJVCI: Internal jugular vein collapsibility index; ONSD: Optic nerve sheath diameter; Dmax: Maximum diameter of internal jugular vein.
There are two studies evaluating ISBP block with near-infrared spectroscopy (NIRS) and its effect on cerebral oxygenation.1,8 The major disadvantage of these studies is that all patients were under general anaesthesia. Even if other factors affecting ICP are present in those studies, ISBP block does not decrease cerebral oxygenation in patients in the beach-chair position.1,8 In a retrospective study, by Coşarcan et al., they found that ISBP block can increase cerebral oxygenation in patients in the beach-chair position.1 Their hypothesis was related to cervical sympathetic blockade due to local anaesthetic injection during ISBP block, which cases cerebral vasodilation and increases cerebral oxygenation. The present hypothesis differed from that of Cosarcan and colleagues. It was thought that local anaesthetic may limit the maximum IJV diameter and venous return from the cranium is reduced. ICP may have increased as a result of this decreased venous return. Cerebral oxygenation may have increased due to increased ICP. In the study by Cosarcan et al. ISBP block was catheter-guided, whereas in this study, we examined the effects of single-shot ISBP block using 25 ml of the anaesthetic drug. Hence, the drug-volume effect problem is rarely experienced in continuous ISBP block compared to single-shot, cervical sympathetic blockade may be the cause of ICP increase in their patient group.
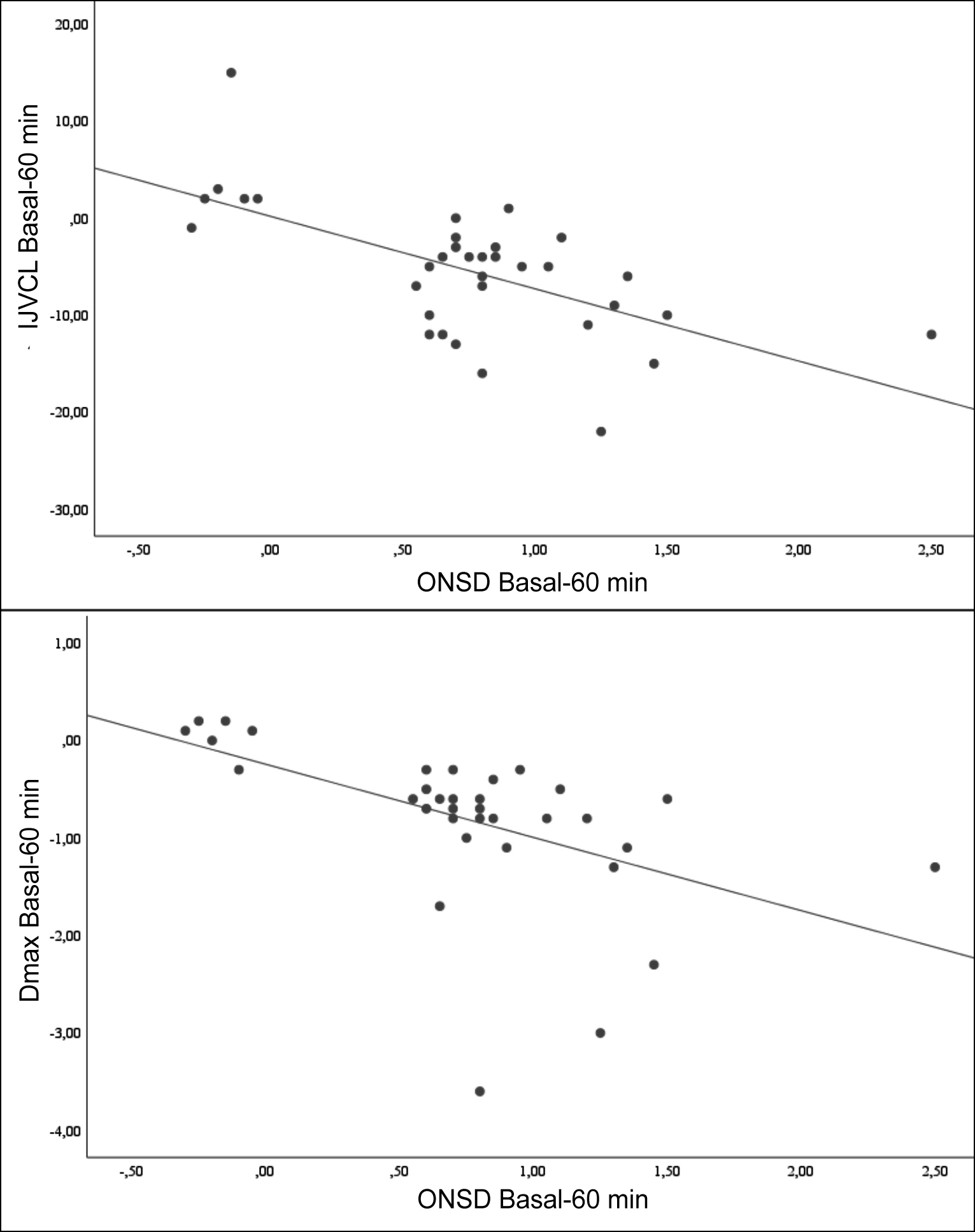 Figure 2: The correlation between ONSD and IJV-CI in terms of change in values measured at basal and 60th minute and the correlation between ONSD and Dmax in terms of change in values measured at basal and 60th minute.
Figure 2: The correlation between ONSD and IJV-CI in terms of change in values measured at basal and 60th minute and the correlation between ONSD and Dmax in terms of change in values measured at basal and 60th minute.
IJVCI: Internal jugular vein collapsibility index; ONSD: Optic nerve sheath diameter; Dmax: Maximum diameter of internal jugular vein.
Basaran and colleagues performed intraocular pressure (IOP) assessment with tonometry by applying only interscalene block in 30 patients who did not receive general anaesthesia and found low IOP values in the eye on the side of the block and concluded that ISBP can be used safely in patients with glaucoma.9 In their study, 30 ml single-shot ISBP block was applied and Horner’s syndrome developed in all patients. The development of Horner's syndrome indicates severe cervical sympathetic ganglion blockade. Although, there are studies suggesting an increase in ICP due to an increase in cerebral blood flow as a result of cerebral vasodilation caused by the sympathetic blockade, cerebral autoregulatory mechanisms are still a controversial issue in the literature.10,11 The reason why Coşarcan et al. did not comment on ICP in their study evaluating cerebral oxygenation is that the stage after cerebral vasodilation due to sympathetic blockade is not clear in the mechanism of cerebral autoregulation.1 Although, there is a correlation between IOP and ICP, IOP measurements may not reflect minimal changes in ICP. In the study by Li et al. on IOP-ICP correlation, IOP was able to accurately predict ICP in 65.4% of patients.12 Because IOP and ICP are related but relatively independent pressure systems. In addition to studies reporting a weak correlation between IOP and ICP, there are also studies that do not find these two measurements correlated.13-17 Therefore, interpreting ICP based on the IOP values measured by Başaran et al. in patients with ISBP block would be an out-of-truth assessment.9
IJV-CI has been used in recent years as an ultrasonographic measurement reflecting the intravascular fluid status in the patient. Although, there are studies reporting that inferior vena cava diameter measurements give more reliable results than IJV-CI, IJV-CI can also give an idea about intravascular volume status.18 The most important handicap of IJV-CI is that it can be easily affected by patient position. In the study by Simka et al. IJV measurements were performed while patients were in supine, right lateral decubitis, left lateral decubitis and sitting positions and the lowest Dmax measurement was found in the sitting position.19
In a study of 31 patients comparing the IJV-CI of hypovolemic and euvolemic patients, the mean IJV-CI of euvolemic patients was found to be 23%.19 In this study, the baseline mean IJV-CI values were 24.18±9.02%. Killu et al. performed measurements in a 30-degree head-up position, whereas in the present cases, measurements were performed in a 45-degree head-up position.20 In the present study, basal IJV-CI values can be considered euvolemic because elective cases in which preoperative fluid replacement was included. Since fluid deficit or fluid overload is a factor affecting ICP, using IJV-CI in basal measurements (before block) in this study has an important place in terms of demonstrating that patients are euvolemic.
In the study, the most important result revealing the drug-volume effect at 25 ml was the decrease in Dmax. Since Dmax is more effective than Dmin in the IJV-CI formula, a decrease in IJV-CI was also observed due to the decrease in Dmax. Thus, in this study, it was demonstrated that 25 ml of anaesthetic used in single-shot ISBP block reduced IJV diameter. Reduced IJV diameter means decreased venous return from the cranium to the heart. This led to an increase in ICP, causing ONSD measurements to be higher than baseline in 29 of 34 patients.
This study has some limitations; the amount of intraoperative bleeding was not recorded. Although, these are surgeries without major bleeding, the amount of bleeding is a value that can affect ICP intraoperatively. Measurement of IJV on the unblocked side would have been an important contribution to the study to reveal the compensation mechanism of decreased venous return. In this study, the authors investigated the volume effect of 25 ml of drug, but a volume-controlled study can be designed later to reveal the drug volume effect more clearly. The number of patients was also one of the limitations of the study.
CONCLUSION
Single-shot ISBP block with 25 ml of local anaesthetic may increase ICP. Although, there are many other factors that increase ICP, in clinical practice, repeated intraoperative ONSD measurements are recommended in patients operated with ISBP block.
ETHICAL APPROVAL:
The study was approved by the Ethics Committee of Sivas Cumhuriyet University [Institutional Review Board (IRB) No. 2021-12/01 IRB date: 21.12.2021].
CLINICAL TRIAL REGISTRATION:
This research was registered to clinicaltrials.gov.tr with the clinical trial number of NCT05434975.
PATIENTS’ CONSENT:
Consent for publication was obtained from the patients whose data are included in this manuscript.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
OG: Conception and designing of the study, selected patients, created the study plan, and wrote the manuscript.
OA: Selected patients analysed the data and critically reviewed for important intellectual content.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Cosarcan SK, Gurkan Y, Dogan AT, Koyuncu O, Ercelen O. Could ınterscalene block possibly be protective against cerebral ischemia during shoulder surgery in a beach chair position? Cureus 2021; 13(7):e16773. doi: 10. 7759/cureus.16773.
- Maissan IM, Dirven PJ, Haitsma IK, Hoeks SE, Gommers D, Stolker RJ. Ultrasonographic measured optic nerve sheath diameter as an accurate and quick monitor for changes in intracranial pressure. J Neurosurg 2015; 123(3):743-7. doi: 10.3171/2014.10.JNS141197.
- Kimberly HH, Shah S, Marill K, Noble V. Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure. Acad Emerg Med 2008; 15(2): 201-4. doi: 10.1111/j.1553-2712.2007.00031.x.
- Omileke D, Bothwell SW, Pepperall D, Beard DJ, Coupland K, Patabendige A, et al. Decreased ıntracranial pressure elevation and cerebrospinal fluid outflow resistance: A potential mechanism of hypothermia cerebroprotection following experimental stroke. Brain Sci 2021; 11(12): 1589. doi: 10.3390/brainsci11121589.
- Pedersen SH, Andresen M, Lilja-Cyron A, Petersen LG, Juhler M. Lumbar puncture position influences intracranial pressure. Acta Neurochir 2021; 163(7):1997-2004. doi: 10.1007/s00701-021-04813-3.
- Rossi S, Picetti E, Zoerle T, Carbonara M, Zanier ER, Sitocchetti N. Fluid management in acute brain ınjury. Curr Neurol Neurosci Rep 2018; 18(11):74. doi: 10. 1007/s11910-018-0885-8.
- Nunes RR, Bersot CDA, Garritano JG. Intraoperative neurophysiological monitoring in neuroanaesthesia. Curr Opin Anaesthesiol 2018; 31(5): 532-8. doi: 10.1097/ACO. 0000000000000645.
- Soeding PF, Currigan DA, Mamo Y, Hoy G. Effect of ınterscalene anaesthesia on cerebral oxygen saturation. Anaesth Intensive Care 2016; 44(3):359-363. doi: 10. 1177/0310057X1604400301.
- Basaran B, Yilbas AA, Gultekin Z. Effect of interscalene block on intraocular pressure and ocular perfusion pressure. BMC Anesthesiol 2017; 17(1):144. doi: 10. 1186/ s12871-017-0436-x.
- Partington T, Farmery A. Intracranial pressure and cerebral blood flow. Anesth Intensive Care Med 2014; 15(4): 189-94.
- Zhang R, Crandall CG, Levine BD. Cerebral hemo-dynamics during the valsalva maneuver ınsights from ganglionic blockade. Stroke 2004; 35(4):843-7. doi: 10.1161/01.STR.0000120309.84666.AE.
- Li Z, Yang Y, Lu Y, Liu D, Xu E, Jia J, et al. Intraocular pressure vs. intracranial pressure in disease conditions: A prospective cohort study (Beijing iCOP study). BMC Neurol 2012; 12:66. doi: 10.1186/1471-2377-12-66.
- Sheeran P, Bland JM, Hall GM. Intraocular pressure changes and alterations in intracranial pressure. Lancet 2000; 355(9207):899. doi: 10.1016/s0140- 6736(99) 02768-3.
- Han Y, McCulley TJ, Horton JC. No correlation between intraocular pressure and intracranial pressure. Ann Neurol 2008; 64(2):221-4. doi: 10.1002/ana.21416.
- Czarnik T, Gawda R, Latka D, Kolodziej W, Sznajd-Weron K, Weron R. Noninvasive measurement of intracranial pressure: Is it possible? J Trauma 2007; 62(1): 207-11. doi: 10.1097/01.ta.0000219128.29515.d5.
- Kirk T, Jones K, Miller S, Corbett J. Measurement of intraocular and intracranial pressure: Is there a relationship? Ann Neurol 2011; 70(2):323-6. doi: 10. 1002/ana.22414.
- Czarnik T, Gawda R, Kolodziej W, Latka D, Sznajd-Weron K, Weron R. Associations between intracranial pressure, intraocular pressure and mean arterial pressure in patients with traumatic and non-traumatic brain injuries. Injury 2009; 40(1):33-9. doi: 10.1016/j.injury.2008.10.010.
- Kent A, Patil P, Davila V, Bailey JK, Jones C, Evans DC, et al. Sonographic evaluation of intravascular volume status: Can internal jugular or femoral vein collapsibility be used in the absence of IVC visualisation? Ann Thorac Med 2015; 10(1):44-9. doi: 10.4103/1817-1737.146872.
- Simka M, Czaja J, Kowalczyk D. Collapsibility of the internal jugular veins in the lateral decubitus body position: A potential protective role of the cerebral venous outflow against neurodegeneration. Med Hypotheses 2019; 133:109397. doi: 10.1016/j.mehy. 2019.109397.
- Killu K, Coba V, Huang Y, Andrezejewski T, Dulchavsky S. Internal jugular vein collapsibility index associated with hypovolemia in the intensive care unit patients. Crit Ultrasound J 2010; 2:13-17.