Effects of Low-intensity Extracorporeal Shockwave Therapy on Erectile Dysfunction: A Systematic Review and Meta-analysis
By Shuai Liu, Jiuzhou Pu, Xu Li, Rongxin Li, Yanan Wang, Zhilong DongAffiliations
doi: 10.29271/jcpsp.2022.09.1181ABSTRACT
This present systemic review and meta-analysis was conducted to assess the effectiveness of low-intensity extracorporeal shockwave therapy (Li-ESWT) on erectile dysfunction (ED) based on the relevant randomised controlled trials (RCTs). A comprehensive search of databases, including Medline and Embase databases, from 1st January 2012 to 31st July 2020, that investigated the efficacy of Li-ESWT for ED, was searched. All the trials were divided into two groups: the experimental group received a different shockwave treatment, and the control group received the same treatment as the corresponding experimental group vibration, sound, etc) but no energy transmission. The primary endpoint was the International Index of Erectile Function-Erectile Function domain (IIEF-EF) score/questionnaire or erectile hardness score (EHS). The average IIEF-EF score was increased with statistical significance in the Li-ESWT group relative to the control group (p<0.001). Besides, the Li-ESWT group had evidently elevated changes in IIEF-EF score (p<0.001). Altogether seven articles reported the remarkably elevated EHS score with different total pulses (p<0.001). The favourable outcomes in terms of the average IIEF scores were observed in the cases developing mild or moderate ED (p<0.001). Compared with placebo treatment, Li-ESWT alleviates ED symptoms in patients, particularly those who have mild or moderate ED. Taken together, these results suggest that the Li-ESWT may hold promise for patients with ED.
Key Words: Erectile dysfunction, Low-intensity extracorporeal shockwave therapy, Meta-analysis, Randomised controlled trials.
INTRODUCTION
Erectile dysfunction (ED) is the most common male sexual dysfunction, which means that the penis cannot achieve or maintain sufficient erection to complete satisfactory sexual life. ED is an obvious health issue affecting 52% males (aged 40–70 years) and 22% males aged<40 years in terms of quality of their life.1,2 At present, treatment of ED mainly includes a step-wise method to modify risk factors, optimise the medical comorbidities, and to carry out medical treatments, like vasoactive agents given through cavernous body and phosphodiesterase type 5 (PDE5) inhibitors administered orally; besides, a penile prosthesis may also be implanted in advanced cases.3 While many patients are satisfied with these treatments, others are dissatisfied due to the poor efficacy or inability to use them. Furthermore, the above therapeutic means mainly aim to enhance erectile function but do not address the pathophysiological factors.4,5
Li-ESWT has been proposed as the low-cost and low-risk minor adverse effects therapy. In 2010, Vardi et al. first described its use on ED;6 after that, several reports have been published with encouraging results. Some researchers have established models of erectile dysfunction in diabetic rats and found that low-energy shockwaves promote penile tissue regeneration.7 The published studies have different samples, different protocols, and different inclusion criteria. There is still no evidence of what type of the patient is the best candidate for Li-ESWT. The present meta-analysis was conducted aiming to examine the effectiveness of Li-ESWT on improving ED in the male patients based on IIEF-EF score or EHS relative in relationto those who received placebo treatment, and provide a formal recommendations based on the literature review for future RCTs.
METHODOLOGY
The Medline and Embase databases were systemically searched, from 1st January 2012 to 31st July 2020. This search strategy was as follows: (Shock Wave) or (Shockwave) and (erectile dysfunction or IIEF or EHS). Since this study was a systematic review of the previous articles, ethical approval and informed consent were not required. A flow diagram for the study selection process is outlined in Figure 1.
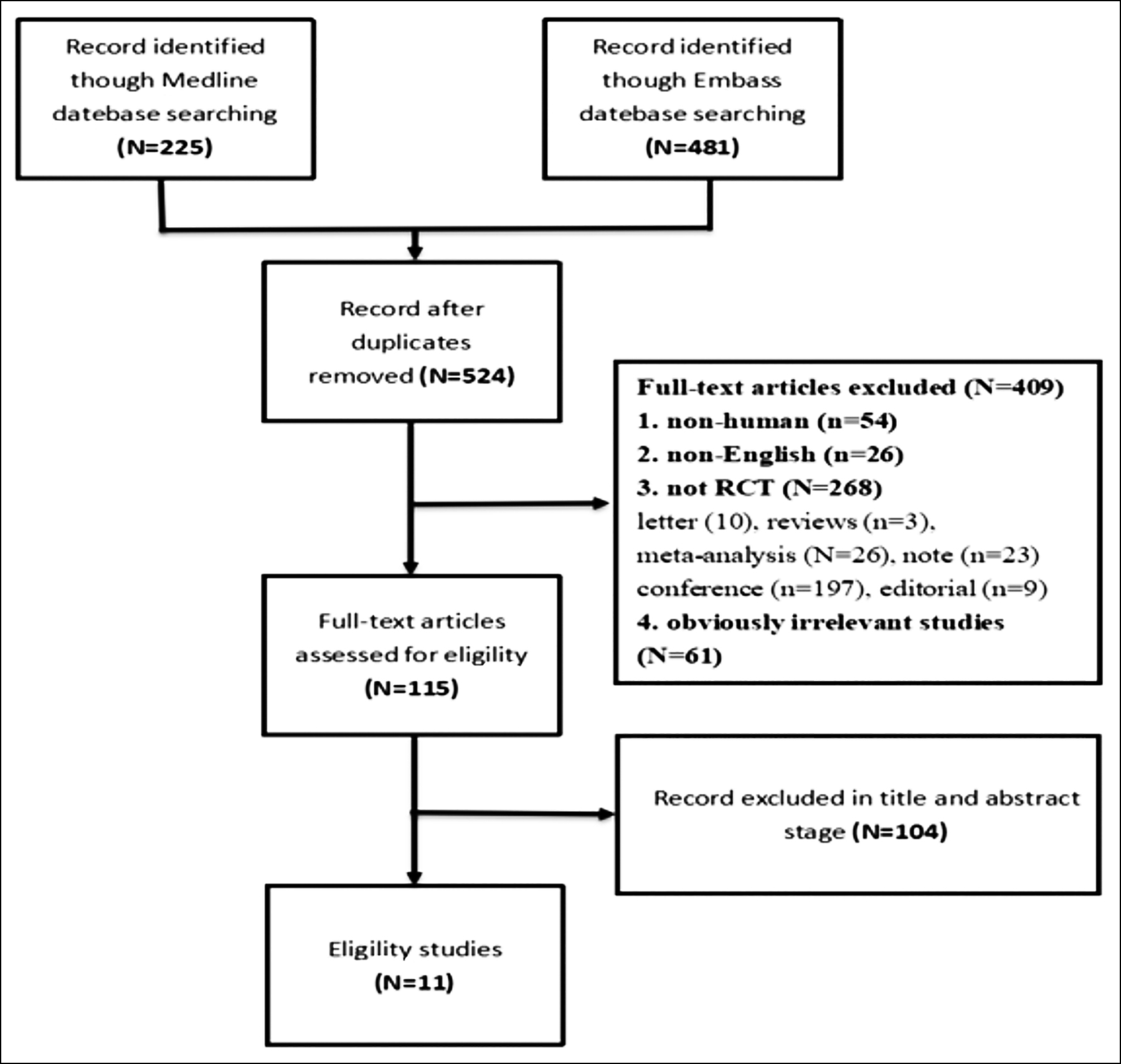 Figure 1: Flow diagram for study selection.
Figure 1: Flow diagram for study selection.
Those studies not published in the English language, not conducted on human beings, involving cases suffering from Peyronie’s disease, and the non-RCTs were excluded. Altogether 11 RCTs were finally selected for the subsequent analysis. To be specific, two reviewers (Liu and Pu) read the titles and abstracts independently to examine whether the studies were eligible according to the above exclusion criteria. Later, the two reviewers read the full texts carefully to eliminate articles that conformed to the exclusion criteria. A third reviewer settled down any disagreement between them, and a consensus was reached by mutual negotiation and discussion.
In this article, the Cochrane risk-of-bias assessment method was utilised to assess the eligible RCTs quality and the risk of bias.8 The Cochrane Collaboration standards (Cochrane collaboration Risk of Bias Assessment Tool) were employed to evaluate the study quality by the two researchers (Liu and Pu).9 In the present meta-analysis, the following quality items, including concealment of allocation, random sequence generation, participant and personnel blinding, outcome assessment blinding, selective reporting, incomplete outcome data, along additional sources of bias were evaluated. For all items, they were evaluated as adequate, inadequate, or unclear, corresponding to low, high or uncertain risk of bias, respectively according to Cochrane Handbook.9 RevMan 5.4 software (Review Manager, 2014) was utilised to generate a graph and summarise the risks of bias. Two trained investigators (Liu and Li) were responsible for the independent assessment of each domain. Any disagreement among them was settled down by another (Pu) researcher and a consensus was reached by mutual negotiation and discussion.
Two authors (Liu and Pu) independently carried out data extraction from the 11 available RCTs involving 814 participants. Items abstracted pertained to study characteristics, patient characteristics, and patient-reported outcomes. Data obtained from the eligible studies are presented in Table I. The Review Manager version 5.4 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) was adopted to analyse data from the eligible articles.10 In this work, the primary endpoint was IIEF-EF score used to assess the efficacy of Li-ESWT in ED, while the secondary endpoint was alterations of EHS. None of the enrolled studies reported any severe adverse reaction. The Q-statistic determined upon the chi-square test was adopted to test the heterogeneity in the pooled results, while I2 index was used to calculate inconsistency for determining the heterogeneity effects. When obvious heterogeneity was detected, there was diversity in the variety of study features, like ED severity, total pulse number, as well as follow-up period. The fixed model was selected in the case of no significant heterogeneity (I2 < 60%, p > 0.05); otherwise, the random effect model was adopted, and subgroup analysis might be conducted. In case of high heterogeneity in the subgroup analysis (I2 > 60%, p < 0.05), the random effect model was adopted. The continuous variables were expressed as 95% confidence interval (CI) with the mean difference (MD), whereas dichotomous variables were expressed as 95% CI with odds ratio (OR). In this meta-analysis, the results are presented in the form of a forest plot. A difference of p<0.05 indicated statistical significance.11
RESULTS
From the databases, 706 related documents were identified; 182 articles were repeats and based on the titles and abstracts review, 409 were excluded [either because they were non-human trials (n =54) or non-English language articles (n=26)], non-RCT articles (n=268), and irrelevant studies (n=61). Two authors (Liu and Pu) read the full texts of the remaining 115 articles, and 11 studies were finally included in the analysis.12–22 Figure 1 exhibits the preferred reporting items for systematic reviews and meta-analyses (PRISMA) flowchart,23 which illustrates the screening and selection process.
According to the Cochrane Collaboration risk-of-bias estimation, for random sequence generation, only 3 trials,17-19 uncertain of the described method of randomisation sequence, were deemed to be at unclear risk, and other trials were at low-risk. In four trials the methods used to conceal the allocation were unclear,12-14,20 and in the other seven trials, the allocation concealment methods were determined as low-risk.15-19,21,22 In one trial,17 cases that were unaware of whether they received placebo treatment were deemed as high-risk. Specifically, seven trials used a standard double-blind format.12-15,20-22 Other three trials were uncertain, if they described the method of blinding.16,18,19 Each study showed a low-risk due to selective reporting or incomplete outcome data (Figure 2).
The seven eligible studies suggested that relative to placebo treatment, male ED patients receiving Li-ESWT had markedly increased IIEF-EF scores [(MD: 2.77 points; 95% CI (1.74, 3.79); I²= 66%, p<0.001; Figure 3a].12-15,17,21,22 Besides, patients were followed up at 1, 3, 6, 9, and 12 months and 7 weeks, and it was found that the patients receiving Li-ESWT had evidently elevated IIEF scores [(MD: 2.96 points; 95% CI [2.31, 3.61] ; I²= 48%, p<0.001; Figure 3b)].
Four articles reported the changes in IIEF-EF scores.15,17,19,21 After data extraction and analysis, the patients receiving Li-ESWT showed evidently elevated changes in IIEF-EF scores relative to those receiving placebo treatment [(MD: 3.75 points; 95% CI (3.15, 4.35); I2 51%, p<0.001; Figure 4].
Table I: Current studies of low-intensity extracorporeal shock wave treatment for erectile dysfunction patients.|
Study authors |
Years of publication |
Number of people design included (n1/n2) |
Setup of Li-ESWT |
Protocol of Li-ESW treatment |
Follow-up, weeks |
Evaluation tools for ED |
p-value of IIEF after Li-ESWT |
study type |
||
|
Energy density, mJ/mm2 |
No. of pulses each treatment |
No. Of treatments each week |
Total treatment courses, weeks |
|||||||
|
Fojecki et al.12 |
2017 |
58/60 |
0.09 |
600 |
1 |
10 |
4,18 |
IIEF, EHS, EDITS, SQoL-M |
0.902 |
RCT |
|
Kalyvianakis et al.13 |
2017 |
30/16 |
0.09 |
1500 |
2 |
6 |
4, 12, 24, 32, 48 |
IIEF, EHS |
<0.05 |
RCT |
|
Kim et al.14 |
2019 |
38/40 |
20,15,12 |
3000 |
2 |
12 |
4, 7 |
IIEF, EHS, SEP2, SEP3 |
<0.001 |
RCT |
|
Kitrey et al.15 |
2016 |
37/18 |
0.09 |
1500 |
2 |
6 |
4 |
IIEF, EHS, FMD, CGIC |
<0.05 |
RCT |
|
Olsen et al.16 |
2015 |
51/54 |
0.15 |
3000 |
1 |
5 |
4, 12, 24 |
IIEF, EHS |
0.67 |
RCT |
|
Sramkova et al.17 |
2019 |
30/30 |
0.16 |
6000 |
2 |
2 |
4, 12 |
IIEF-5, EHS, GAQ, SEP2, SEP3 |
<0.05 |
RCT |
|
Srini et al.18 |
2015 |
95/40 |
NA |
NA |
NA |
NA |
4, 12, 24, 32, 48 |
IIEF, EHS, CGIC |
0.0001 |
RCT |
|
Vardi et al.19 |
2012 |
40/20 |
0.09 |
1500 |
2 |
6 |
4 |
IIEF, EHS, penile blood flow |
0.0322 |
RCT |
|
Vinay et al.20 |
2020 |
40/36 |
0.09 |
5000 |
1 |
4 |
4, 12, 24 |
IIEF-EF,EHS, SEP2,SEP3, GAQ1 |
<0.05 |
RCT |
|
Yee et al.21 |
2014 |
30/28 |
0.09 |
1500 |
2 |
6 |
4 |
IIEF-ED, EHS |
0.001 |
RCT |
|
Yamaçake et al.22 |
2018 |
10/10 |
0.09 |
2000 |
2 |
3 |
4, 16, 48 |
IIEF, EHS |
<0.0001 |
RCT |
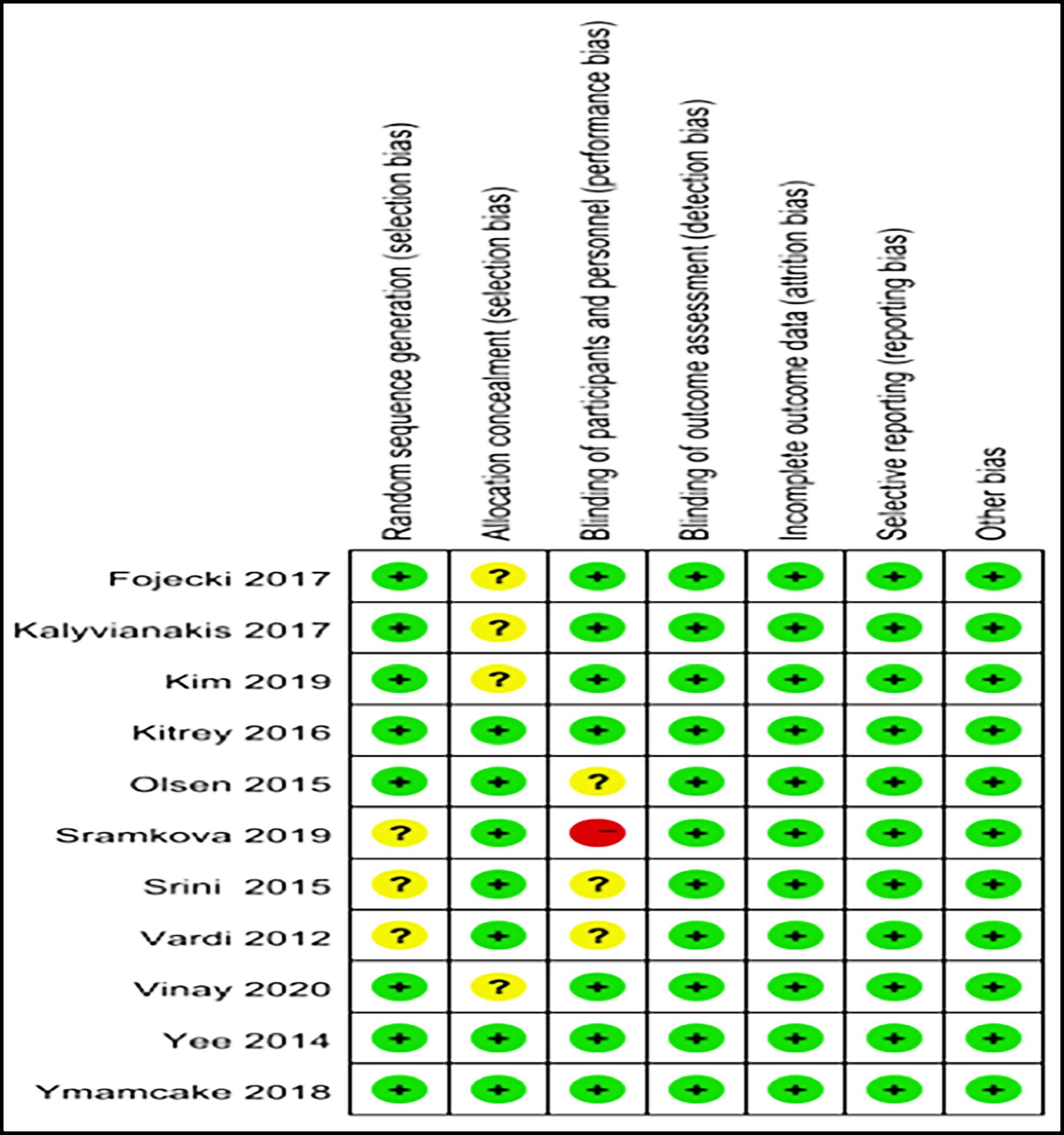 Figure 2A: Eleven randomised controlled trials included in this meta analysis. Quality of studies was assessed with the Cochrane Collaboration’s tool. A: Risk-of-bias graph.
Figure 2A: Eleven randomised controlled trials included in this meta analysis. Quality of studies was assessed with the Cochrane Collaboration’s tool. A: Risk-of-bias graph.
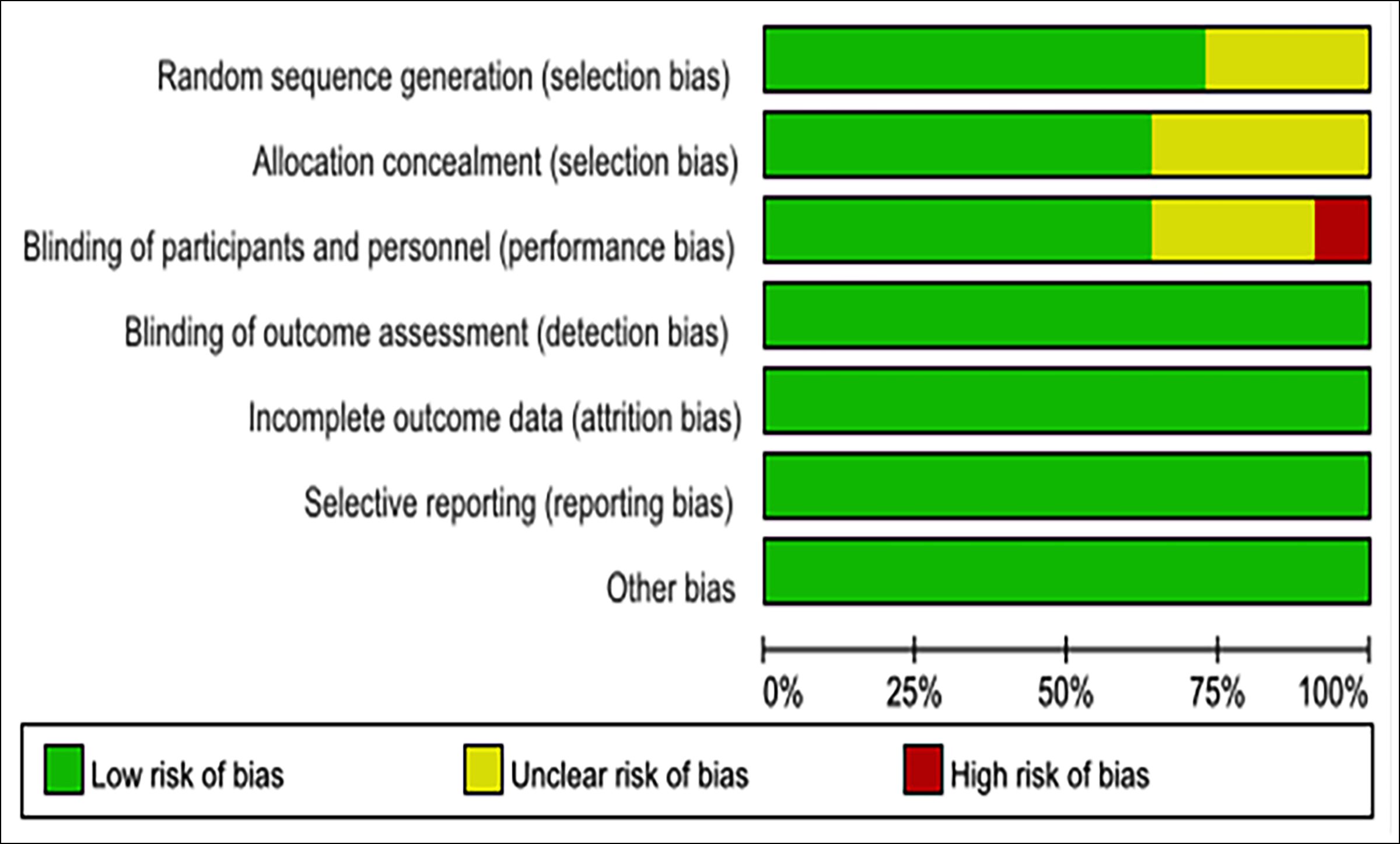 Figure 2B: Eleven randomised controlled trials included in this meta analysis. Quality of studies was assessed with the Cochrane Collaboration’s tool. B: Risk-of-bias summary.
Figure 2B: Eleven randomised controlled trials included in this meta analysis. Quality of studies was assessed with the Cochrane Collaboration’s tool. B: Risk-of-bias summary.
There were 9 articles that mentioned the ED severity, based on IIEF score or responds to PDE5i.13-15,17-22 Some mentioned the IIEF-EF scores among the cases with severe ED following the treatment,15,21 whereas others mentioned those scores among the cases with mild or moderate ED.13,14,17,22
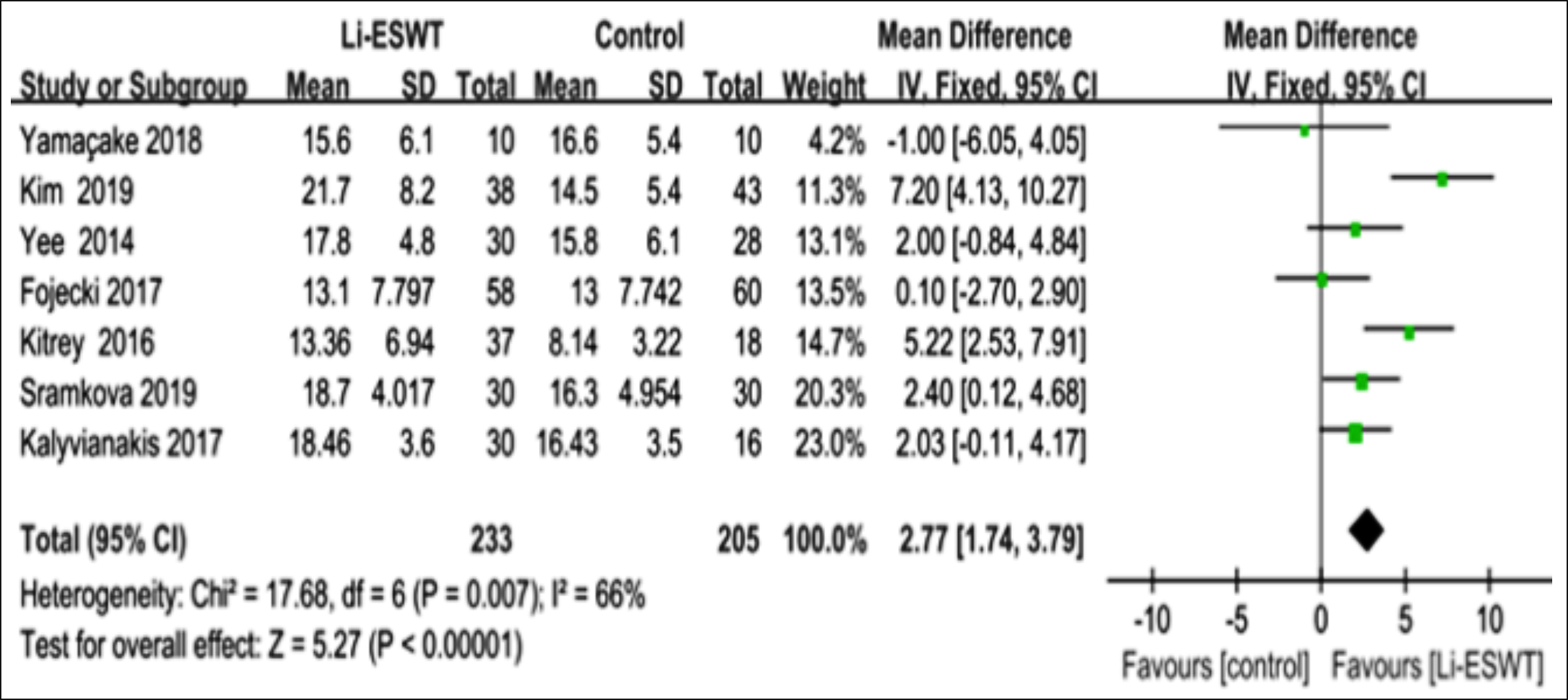 Figure 3a: Clinical outcomes of meta-analysis on the IIEF-EF score. Mean IIEF-EF score.
Figure 3a: Clinical outcomes of meta-analysis on the IIEF-EF score. Mean IIEF-EF score.
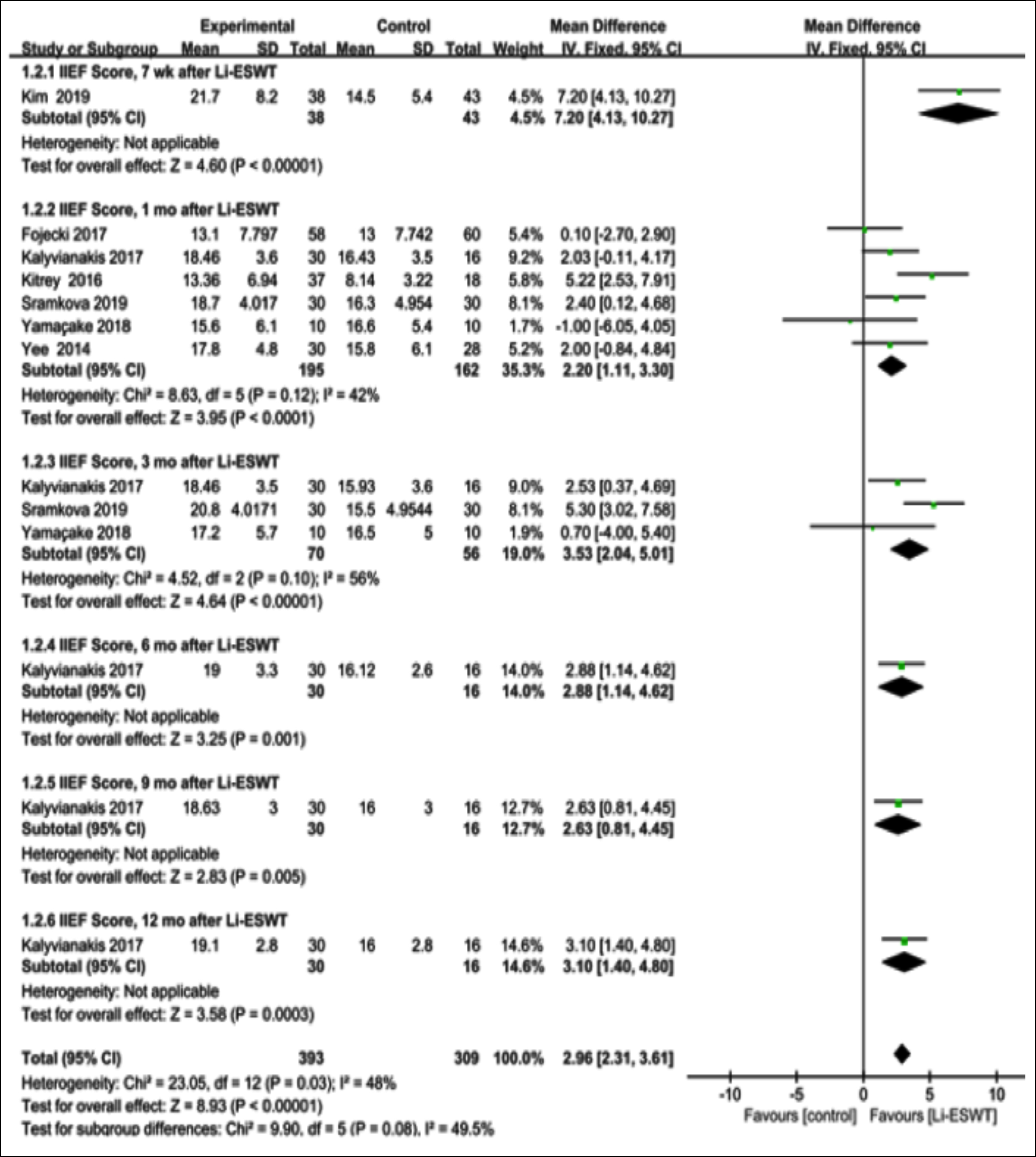 Figure 3b: Clinical outcomes of-meta analysis on the IIEF-EF score mean IIEF EF score of follow-up.
Figure 3b: Clinical outcomes of-meta analysis on the IIEF-EF score mean IIEF EF score of follow-up.
In the patients receiving Li-ESWT treatment, the IIEF-EF scores were elevated relative to those receiving placebo treatment [(MD: 3.21 points; 95% CI (2.10, 4.31); I2=65%, p<0.001; Figure 5a]. Some mentioned post-treatment EHS scores for the cases developing severe ED,15,20 whereas others mentioned those scores in the cases with mild or moderate ED.14,18,19 Patients receiving Li-ESWT treatment had dramatically elevated IIEF-EF scores in relation to those taking placebo treatment [OR: 10.40 points; 95% CI (5.60, 19.31); I2 66%, p<0.001; Figure 5b].
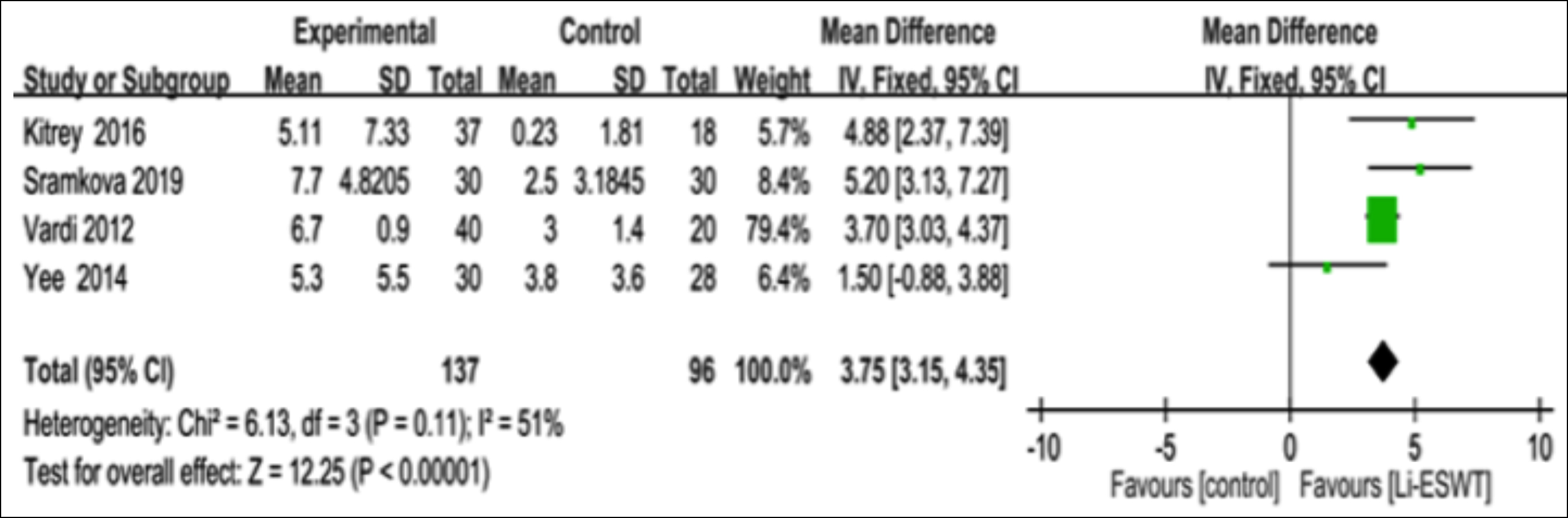 Figure 4: Clinical outcomes of meta analysis on the IIEF EF score change of IIEF EF score.
Figure 4: Clinical outcomes of meta analysis on the IIEF EF score change of IIEF EF score.
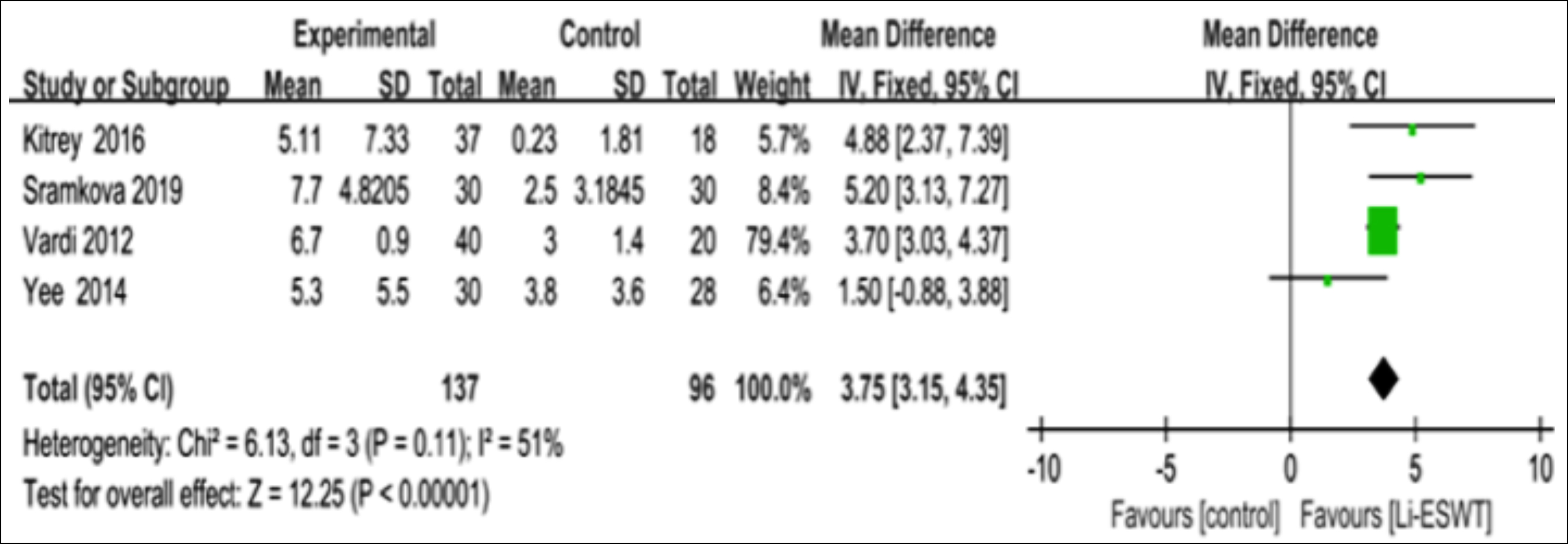 Figure 5a: Clinical outcomes of meta analysis on the IIEF EF score mean of IIEF EF score on severity of ED.
Figure 5a: Clinical outcomes of meta analysis on the IIEF EF score mean of IIEF EF score on severity of ED.
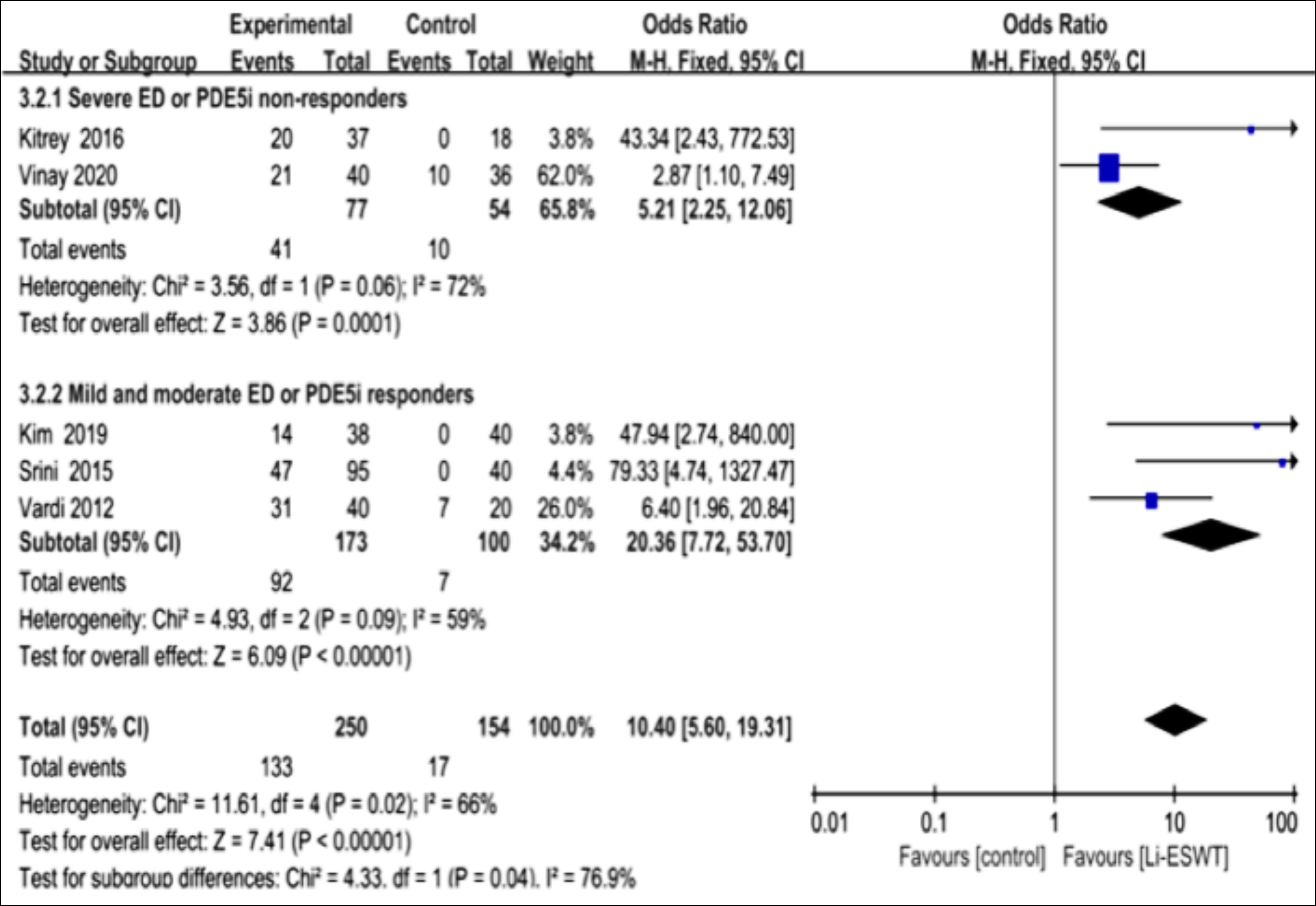 Figure 5b: Clinical outcomes of meta analysis on the EHS score on severity of ED.
Figure 5b: Clinical outcomes of meta analysis on the EHS score on severity of ED.
There were 7 RCTs mentioning EHS scores with different total pulses, which reported that the EHS scores evidently elevated following the Li-ESWT (OR: 9.37; 95% CI [5.65, 15.52. ; I2 61%, p<0.001).14-16,18-20,22 Olsen et al. used 15,000 shockwaves,16 whereas the other four articles used 18,000 pulses shockwaves.14,15,18,19 Clearly, Li-ESWT increased the penis EHS scores to different degrees among the ED cases, no matter how many shockwaves were used (Figure 6).
DISCUSSION
Eleven RCTs, including 814 male patients, were enrolled in the present systematic review and meta-analysis.12-22 The pooled results suggested that ED patients, who received Li-ESWT, had markedly improved IIEF-EF and EHS scores relative to those who received placebo treatment. Thus, Li-ESWT may be adopted to be a treatment for ED cases.
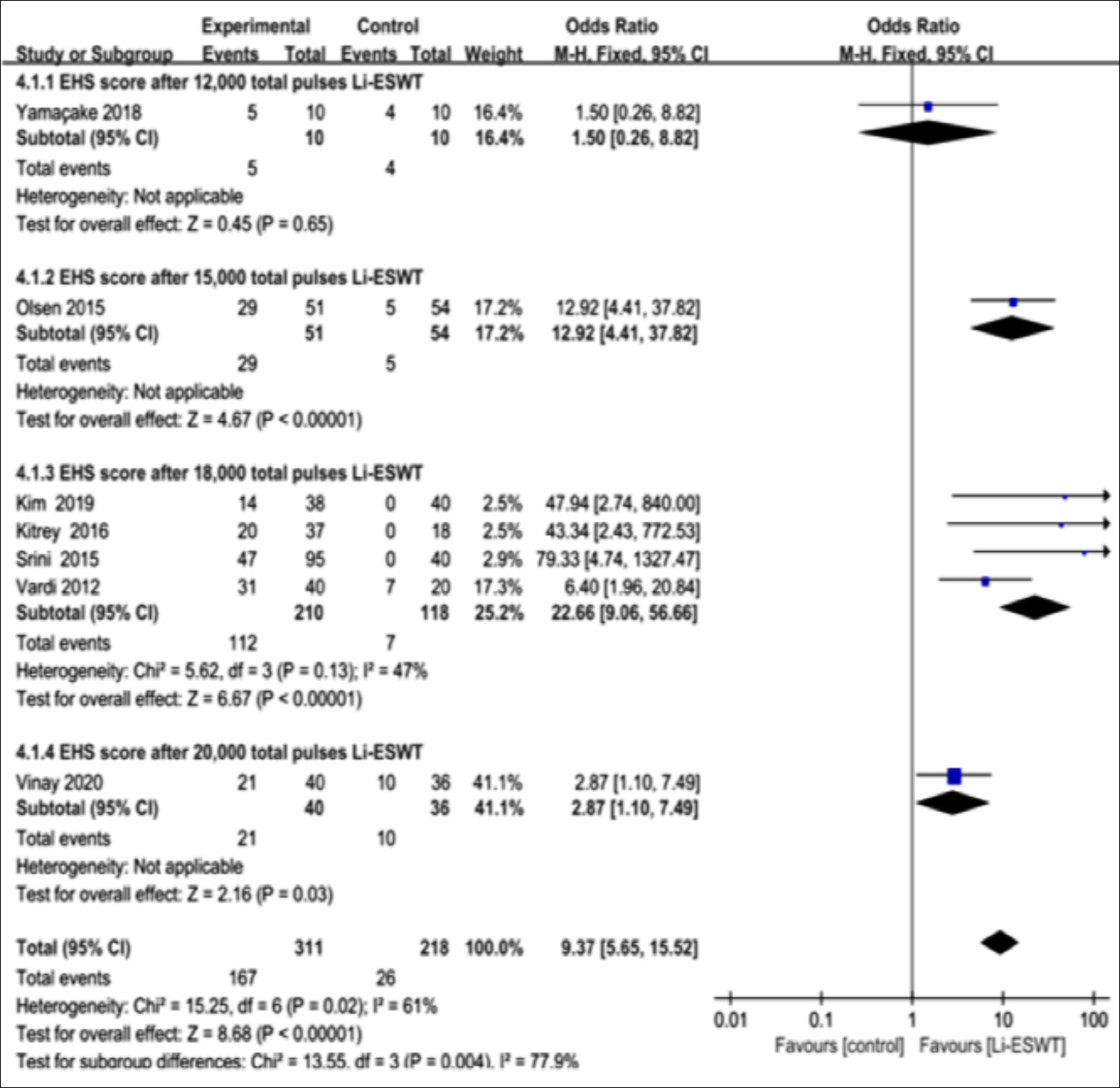 Figure 6: Clinical outcomes of meta analysis on the EHS score with different total pulses.
Figure 6: Clinical outcomes of meta analysis on the EHS score with different total pulses.
In previous studies, the minimal clinically important difference was indicated by the change of 4 points in the IIEF-EF score, and it stands for a potentially and clinically important difference to the patients that may alter the treatment strategy.24 The ED patients receiving Li-ESWT are reported with improved IIEF and EHS scores. In the present meta-analysis, IIEF scores were also improved in the control group,19,21 but none of these improvements was clinically meaningful.
The specific mechanisms, by which Li-ESWT improves the IIEF scores among the ED male patients, remain controversial. According to the some recent studies, these effects could be exerted by promoting cell proliferation, angiogenesis, and tissue regeneration.25,26 The studies on the Li-ESWT efficacy in rat penile tissues reported that the erectile function, together with regeneration of smooth muscles, NOS-expressing nerves and endothelium, is improved after the treatment.27 Besides, Li-ESWT also up-regulates certain protein levels, including nNOS, von Willebrand factor, vascular endothelial growth factor (VEGF), and smooth muscle actin.8 Recently, Li-ESWT is used to treat mouse models with type 2 Diabetes, which is suggested to improve erectile function but not via the NO or cyclic guanosine monophosphate-dependent mechanism.28 In addition, it is indicated by in vitro animal research that Li-ESWT mainly functions in angiogenesis and the improvement of penile hemodynamics to exert its effects.
In 2016, Lu et al. were the first to carry out a systematic review and meta-analysis regarding the effect of Li-ESWT on the ED treatment. More meta-analyses are conducted since then. 29-32 In this meta-analysis, which presents an update of the latest studies, it was demonstrated that the diverse treatment protocols and setup parameters of Li-ESWT greatly affected the therapeutic effect.
Further, age is also a factor affecting the ED severity, which is possibly associated with cytokine production by Li-ESWT. However, the possible effects of ED-related factors, like age, diabetes, hypertension, coronary artery disease, or hyperlipidemia, have not been investigated yet.16,19,21 In the research by Lu et al., the actual association of Li-ESWT with ED severity was not mentioned.29 Yet, it is reported that the Li-ESWT efficacy is tightly correlated with EFD or the energy delivered to the target unit area. In the present meta-analysis, 0.09–0.25 mJ/mm2 EFD was used. More research and long-term treatment should be conducted to determine the relationship between the therapeutic effect and the energy density. In the research by Kim et al. the Li-ESWT therapeutic effect was determined by its dosage.33 Fojecki et al. employed the 6000 treatment shocks for ten weeks,12 while in the other studies, 18,000 treatment shocks were used in nine weeks. Clavijo’s work reported different results since, it was the first published article on the ED male patients alone.30 Moreover, only RCTs were enrolled in the meta-analysis, and that article was deemed to be the level 1a evidence.30 Majority of the articles only carry out follow-up for about one year. Currently, many piezoelectric, electromagnetic, and electrohydraulic generators-based devices are commercially available. In the future, research on Li-ESWT must concentrate on the basic science and clinical researches. More investigation is needed to examine the diverse influencing factors like age, follow-up period, ED severity or devices. The investigators may adopt the MCID of IIEF to accurately evaluate the Li-ESWT effect on treating ED cases.24 Furthermore, according to the latest European Association of Urology (https://uroweb.org/guidelines/) and American Urological Association (https://www.auanet.org/ guidelines-x15197) guidelines, Li-ESWT is being studied and recommended as a new treatment option for men with erectile dysfunction. This is not a standard treatment option but should be considered worthy of study with an evidence level of Grade C. In the future, Li-ESWT might be used in combination with other therapies as an auxiliary method, such as PDE5i and stem cells to maximise the therapeutic effects.
CONCLUSION
Based on this analysis results, Li-ESWT is a promising treatment to improve erectile dysfunction significantly in patients with mild or moderate severity ED. Nevertheless, setup parameters, period of treatment, and type of patients are also very important for the efficacy of Li-ESWT in the treatment. Therefore, further controlled studies are needed to determine which therapeutic options are the most beneficial. However, the specific molecular mechanism(s) of this treatment are unknown. Further studies are also needed to better understand the specific mechanisms involved in Li-ESWT effects on ED.
PATIENTS’ CONSENT:
Written informed consent was obtained from all the study participants.
COMPETING INTEREST:
The authors declared no competing interests.
AUTHORS’ CONTRIBUTION:
ZD: Conceptualisation and methodology, review, writing and editing.
SL: Conceptualisation and methodology, software, validation, data collection and curation, formal analysis, writing the original draft, review, writing and editing.
JP: Software, validation, data collection and curation, write-up and the original draft.
XL: Validation, data collection and curation, review, writing and editing.
RL: Formal analysis, visualisation, drafted original article.
YW: Visualisation, review, writing, and editing.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol 1994; 151(1): 54-61. doi:10.1016/s0022-5347(17) 34871-1.
- Heruti R, Shochat T, Tekes-Manova D, Ashkenazi I, Justo D. Prevalence of erectile dysfunction among young adults: results of a large-scale survey. J Sex Med, 2004; 1(3): 284-91. doi:10.1111/j.1743-6109.04041.x.
- Shamloul R, Ghanem H. Erectile dysfunction. Lancet 2013; 381(9861):153-65. doi:10.1016/S0140-6736(12)60520-0.
- Karakus S, Burnett AL. The medical and surgical treatment of erectile dysfunction: A review and update. Can J Urol 2020; 27(null): 28-35. PMID:32876000.
- Michael RE, Martin GS. Are we overstating the risk of priapism with oral phosphodiesterase Type 5 inhibitors? J Sex Med 2020; 17(8):1579-82. doi:10.1016/j.jsxm.2020. 05.019.
- Yoram V, Boaz A, Giris J, Omar M, Ilan G. Can low-intensity extracorporeal shockwave therapy improve erectile function? A 6-month follow-up pilot study in patients with organic erectile dysfunction. Eur Urol 2010; 58(2):243-8. doi:10.1016/j.eururo.2010.04.004.
- Xuefeng Q, Guiting L, Zhongcheng X, Ludovic F, Haiyang Z, Tom LF, et al. Effects of low-energy shockwave therapy on the erectile function and tissue of a diabetic rat model. J Sex Med 2013; 10(3):738-46. doi:10.1111/jsm.12024.
- Higgins Julian PT, Altman Douglas G, Gøtzsche Peter C, Peter J, David M, Andrew OD, et al. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011; 343(undefined):d5928. doi:10.1136/bmj.d5928.
- Higgins JPT, Altman DG, (editors) Cochrane handbook for systematic reviews of interventions. Version 5.0.0 (updated February 2008) The cochrane collaboration; 2008. Chapter 8: Assessing risk of bias in included studies. www. cochrane-handbook.org.
- Higgins JPT, Green S. The Cochrane collaboration. 2011. Cochrane handbook for systematic reviews of interventions, version 5.2.0.
- Zhang P, Mo L, Li X, Wang Q. Psychological intervention and its immune effect in cancer patients: A meta-analysis. Medicine (Baltimore) 2019; 98(38):e17228. doi:10.1097/ MD.0000000000017228.
- Fojecki GL, Tiessen S, Osther PJ. Effect of low-energy linear shockwave therapy on erectile dysfunction-a double-blinded, sham-controlled, randomised clinical trial. J Sex Med 2017; 14(1):106-12. doi: 10.1016/j.jsxm.2016.11.307.
- Kalyvianakis D, Hatzichristou D. Low-intensity shockwave therapy improves hemodynamic parameters in patients with vasculogenic erectile dysfunction: A triplex ultrasonography-based sham-controlled trial. J Sex Med 2017; 14(7):891-97. doi: 10.1016/j.jsxm.2017.05.012.
- Kim KS, Jeong HC, Choi SW, Choi YS, Cho HJ, Ha US, et al. Electromagnetic low-intensity extracorporeal shock wave therapy in patients with erectile dysfunction: A sham-controlled, double-blind, randomised prospective study. World J Mens Health 2020; 38(2):236-42. doi: 10.5534/wjmh. 190130.
- Kitrey ND, Gruenwald I, Appel B, Shechter A, Massarwa O, Vardi Y. Penile low intensity shock wave treatment is able to shift PDE5i nonresponders to responders: A double-blind, sham controlled study. J Urol 2015; 195(5): 1550-5. doi:10.1016/j.juro.2015.12.049.
- Olsen AB, Persiani M, Boie S, Hanna M, Lund L. Can low-intensity extracorporeal shockwave therapy improve erectile dysfunction? A prospective, randomized, double-blind, placebo-controlled study. Scand J Urol 2015; 49(4):329-33. doi: 10.3109/21681805.2014.984326.
- Sramkova T, Motil I, Jarkovsky J, Sramkova K. Erectile dysfunction treatment using focused linear low-intensity extracorporeal shockwaves: Single-blind, sham-controlled, Randomised Clinical Trial. Urol Int 2020; 104(5-6):417-24. doi: 10.1159/000504788.
- Srini VS, Reddy RK, Shultz T, Denes B. Low intensity extracorporeal shockwave therapy for erectile dysfunction: a study in an Indian population. Can J Urol 2015; 22(1): 7614-22. PMID: 25694008.
- Vardi Y, Appel B, Kilchevsky A, Gruenwald I. Does low intensity extracorporeal shock wave therapy have a physiological effect on erectile function? Short-term results of a randomised, double-blind, sham controlled study. J Urol 2012; 187(5):1769-75. doi: 10.1016/j.juro.2011.12.117.
- Vinay J, Moreno D, Rajmil O, Ruiz-Castañe E, Sanchez-Curbelo J. Penile low intensity shock wave treatment for PDE5I refractory erectile dysfunction: A randomised double-blind sham-controlled clinical trial. World J Urol 2020; 39(6):2217-22. doi:10.1007/s00345–020–03373-y.
- Yee CH, Chan ES, Hou SS, Ng CF. Extracorporeal shockwave therapy in the treatment of erectile dysfunction: A prospective, randomised, double-blinded, placebo controlled study. Int J Urol 2014; 21(10):1041-45. doi: 10.1111/iju.12506.
- Yamaçake KGR, Carneiro F, Cury J, Lourenço R, Françolin PC, Piovesan AC, et al. Low-intensity shockwave therapy for erectile dysfunction in kidney transplant recipients. A prospective, randomised, double blinded, sham-controlled study with evaluation by penile Doppler ultrasonography. Int J Impot Res 2019; 31(3):195-203. doi: 10.1038/s41443– 018–0062–2.
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 2009; 6(7):e1000097. doi:10.1371/journal.pmed.1000097.
- Rosen RC, Allen KR, Ni X, Araujo AB. Minimal clinically important differences in the erectile function domain of the International index of erectile function scale. Eur Urol 2011; 60(5):1010-6. doi:10.1016/j.eururo.2011.07.053.
- Li H, Matheu MP, Sun F, Wang L, Sanford MT, Ning H, et al. Low-energy shock wave therapy ameliorates erectile dysfunction in a pelvic neurovascular injuries rat model. J Sex Med 2016; 13(1):22-32. doi: 10.1016/j.jsxm.2015. 11.008.
- Qiu X, Lin G, Xin Z, Ferretti L, Zhang H, Lue T, et al. Effects of low-energy shockwave therapy on the erectile function and tissue of a diabetic rat model. J Sex Med 2013, 10(3): 738-46. doi:10.1111/jsm.12024.
- Liu J, Zhou F, Li GY, Wang L, Li HX, Bai GY, et al. Evaluation of the effect of different doses of low energy shock wave therapy on the erectile function of streptozotocin (STZ)-induced diabetic rats. Int J Mol Sci 2013; 14(5):10661-73. 10661-73. doi:10.3390/ijms140510661.
- Assaly-Kaddoum R, Giuliano F, Laurin M, Gorny D, Kergoat M, Bernabé J,et al. Low inte nsity extracorporeal shockwave therapy (Li-ESWT) improves erectile function in a model of type II diabetes independently of NO/cGMP pathway. J Urol 2016; 196(3):950-6. doi: 10.1016/j.juro.2016.03.
- Lu Z, Lin G, Reed-Maldonado A, Wang C, Lee YC, Lue TF. Low-intensity extracorporeal shock wave treatment improves erectile function: A systematic review and meta-analysis. Eur Urol 2017; 71(2):223-33. doi: 10.1016/j.eururo.2016.05.050.
- Clavijo RI, Kohn TP, Kohn JR, Ramasamy R. Effects of low-intensity extracorporeal shockwave therapy on erectile dysfunction: A systematic review and meta-analysis. J Sex Med 2017; 14(1):27-35. doi: 10.1016/j.jsxm.2016.11.001.
- Sokolakis I, Hatzichristodoulou G. Clinical studies on low intensity extracorporeal shockwave therapy for erectile dysfunction: A systematic review and meta-analysis of randomised controlled trials. Int J Impot Res 2019; 31(3):177-94. doi: 10.1038/s41443–019–0117-z.
- Man L, Li G. Low-intensity extracorporeal shock wave therapy for erectile dysfunction: A systematic review and meta-analysis. Urology 2018; 119(undefined):97-103. doi: 10.1016/j.urology.2017.09.011
- Kim JH, Kim JY, Choi CM, Lee JK, Kee HS, Jung KI, et al. The dose-related effects of extracorporeal shock wave therapy for knee osteoarthritis. Ann Rehabil Med 2015; 39(4): 616-23. doi:10.5535/arm.2015.39.4.616.