Double Peptic Ulcer Perforation due to Cumulative Effects of Post-surgery Stress and NSAIDs: A Rare Event in Surgical Practice
By Junaid Zia Hashmi, Muhammad Masood-Ur-Rauf Khan Hiraj, Farah Saleem, Usman Malik, Imran Khan MazariAffiliations
doi: 10.29271/jcpsp.2022.04.21ABSTRACT
Peptic ulcer disease affects a large number of people around the world. Complications occur in 10-20% of patients and perforation develops in 2-14% of the cases. It can either be in the pyloric part of the stomach or in the first part of duodenum. Helicobacter pylori infection and nonsteroidal anti-inflammatory drugs (NSAIDs) abuse and smoking are noted to be the most common risk factors in developing countries. Other risk factors are steroid abuse, post-surgery stress, burns and Zollinger-Ellison syndrome. Although small perforations can be treated conservatively but Graham patch repair is the treatment of choice. Double peptic ulcer perforation is a rare event with only a few cases reported worldwide. This patient presented with double peptic ulcer perforation in emergency due to post-surgery stress. She had cesarean section 10 days earlier with delayed recovery.
Key Words: Peptic ulcer disease, Perforation, Graham patch repair, Cesarean section.
INTRODUCTION
A perforated peptic ulcer is a grave complication of peptic ulcer disease (PUD) affecting 2-14% of the patients with PUD.1 Patient of perforated peptic ulcer usually presents with signs and symptoms of the peritonitis. Factors that commonly lead to perforated peptic ulcers are helicobacter pylori infection, cigarette smoking, excessive use of nonsteroidal anti-inflammatory drugs (NSAIDs), stress of serious illness, steroid abuse, and PUD.
It has been noted that 30- and 90-day mortality associated with perforated peptic ulcer is 20% and 30%, respectively.2 Factors contributing towards the poor prognosis of perforated peptic ulcers are the presence of shock at the time of presentation, delay in presentation, metabolic acidosis, extremes of age, decreased body mass index, and excessive smoking.3
Synchronous double perforated duodenal ulcer is a very uncommon condition with only few cases reported worldwide uptill now. Here, we report a case of a 23-year female who developed double perforation of duodenal ulcer due to post-surgery stress and excessive use of NSAIDS.
CASE REPORT
A 23-year female presented in the Emergency Department of the Hospital with the complaints of shortness of breath for one day, generalised abdomen pain for two days, and vomiting, constipation and abdominal distention for two days. There was a history of cesarean section 10 days back, which was followed by delayed recovery. The patient was taking opioids and NSAIDs for postoperative pain. There was no history of fever and weight loss. There was no previous history of pulmonary tuberculosis. The patient was a non-smoker and non-addict. The systemic history was non-significant. There was no family history of the acid peptic disease.
The clinical examination showed her to be a lean young girl of normal build and height. Pulse rate was 124 beats/min, blood pressure 80/50 mmHg, respiratory rate 35 breaths/min, temperature 101oF and warm peripheries on receiving. Her abdomen was distended, tense and tender; hernial orifices were intact and no lymph nodes were palpable on palpation. Liver dullness was absent on percussion and bowel sounds were absent. Per rectal examination was unremarkable. Fine crepitations were audible on both the sides on chest auscultation.
The hemoglobin was 12.7 g/dl and total leucocyte count 30,500/mm3. D-dimers were 3200 ng/ml (normal range: <200 ng/ml). Renal and liver function tests were normal. Arterial pH was 7.2, and PaO2 was 80 mmHg on 50% FiO2. Chest X-ray in erect posture showed free gas under both the domes of diaphragm. Her ultrasound abdomen revealed absent peristalsis and free fluid in the peritoneal cavity. Thus, a diagnosis of sepsis, acute respiratory distress syndrome (ARDS) and peptic ulcer perforation was made.
The patient was resuscitated with intravenous (IV) fluids. Fluid challenge failed to stabilise the blood pressure and nor-epinephrine was started. Exploratory laparotomy was done which revealed two perforations, one in the pylorus and the other on anterior wall of the first part of duodenum with dimensions of 2.5×2.5 and 1×1 cm, respectively (Figure 1). There was 2000 ml free fluid in the peritoneum. Graham’s patch repair of both the perforations was done. The abdomen was washed with 6000 ml normal saline. Postoperative care was continued in the Intensive Care Unit, where the patient was extubated after three days and remained there for two weeks. Postoperative recovery was uneventful. The patient was found to be doing well on follow-up visit one week after the discharge.
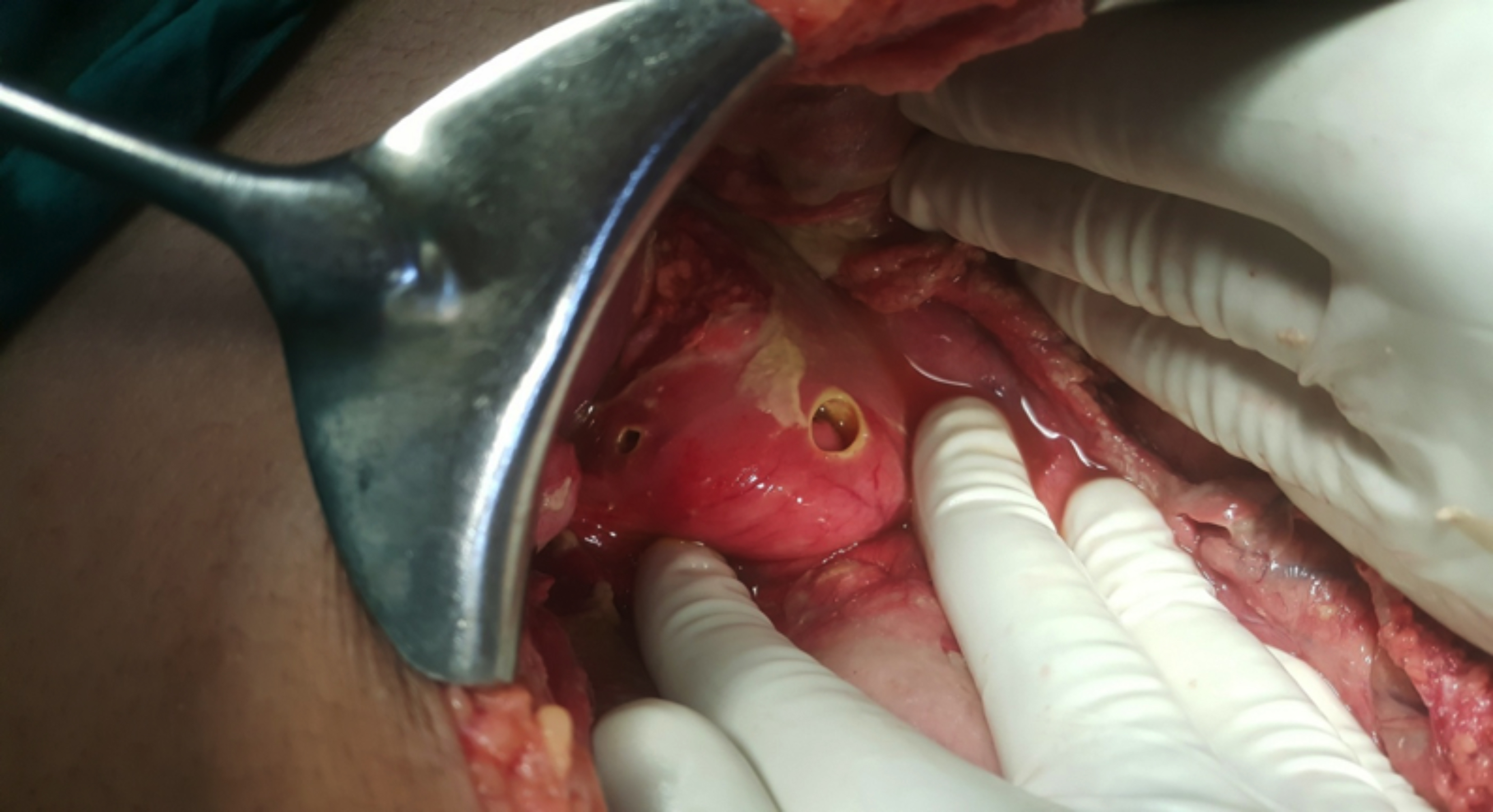 Figure 1: Double peptic ulcer perforations.
Figure 1: Double peptic ulcer perforations.
DISCUSSION
The most common site of perforated peptic ulcer is the first part of duodenum with the pylorus being the second most common site.4 Ulcer on the posterior wall of the duodenum leads to erosion of gastroduodenal artery and the patients present in hemorrhagic shock while perforation on the anterior wall leads to peritonitis. This patient presented with two perforations, one in the pyloric part and the other in the first part of duodenum.
Helicobacter pylori infection is considered the most important risk factor in the development of PUD. Although improved hygiene in developed countries has reduced H. pylori infection rate but it still causes disease in 10-20% of cases.5 According to one study, 2-4% of people, who were regularly using NSAIDS, developed perforated peptic ulcer; but with the introduction of selective COX-2 inhibitors, this percentage has dropped.6 Smoking is an important risk factor in developing countries. A meta-analysis has suggested that 23% of PUD is because of smoking.7 Other important factors are steroid abuse, alcohol, post-surgery stress and Zollinger-Ellison syndrome (ZES).8
Multiple peptic ulcer perforations are very uncommon; and only a few cases have been reported worldwide, in which causative factors were excessive use of NSAIDs, ZES, post-surgery stress, steroid use, burns and Degos disease.9 This patient developed double peptic ulcer perforation in the pylorus and the first part of duodenum due to post-surgery stress.
The conservative management is only feasible, if there is minimal leakage in the peritoneal cavity on a gastroduodenogram. A large number of the patients can be treated conservatively by putting on IV fluids, IV antibiotics, proton pump inhibitors (PPIs); and are kept nil by mouth.10 Regular assessment by a senior surgeon is required during conservative treatment. Endoscopic technique is employed if the patient presents early (< 24 hours) and the size of perforation is small.11 Laparoscopic repair and open surgery have same outcomes. The only difference is that laparoscopic repair is associated with less postoperative pain, but prolonged operating time.12 Primary repair or Graham patch repair with peritoneal lavage are commonly used methods. This patient presented after 24 hours of peritonitis and was already in sepsis, so Graham’s patch repair of both the perforations and a thorough peritoneal lavage were done.
In conclusion, multiple peptic perforations are rare, but could potentially be fatal if not diagnosed in time. One should always keep in mind the possibility of multiple perforations in cases with multiple risk factors, such as analgesic abuse and surgical stress.
PATIENT’S CONSENT:
Informed consent was taken from the patient.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
JZH: Introduction, case report, discussion.
MMURHK: Abstract, discussion, proofreading.
FS: Literature search, introduction.
UM: Discussion, proofreading.
IKM: Literature search, discussion.
REFERENCES
- Lau JY, Sung J, Hill C, Henderson C, Howden CW, Metz DC. Systematic review of the epidemiology of complicated peptic ulcer disease: Incidence, recurrence, risk factors and mortality. Digestion 2011; 84(2):102-13. doi: 10.1159/000 323958.
- Soreide K, Thorsen K, Søreide JA. Strategies to improve the outcome of emergency surgery for perforated peptic ulcer. Br J Surg 2014; 101(1):e51-e64. doi: 10.1002/bjs. 9368.
- Kocer B, Surmeli S, Solak C, Unal B, Bozkurt B, Yildirim O, et al. Factors affecting mortality and morbidity in patients with peptic ulcer perforation. J Gastroenterol Hepatol 2007; 22(4):565-70. doi: 10.1111/j.1440-1746.2006.04500.x.
- Bulut OB, Rasmussen C, Fischer A. Acute surgical treatment of complicated peptic ulcers with special reference to the elderly. World J Surg 1996; 20(5): pp. 574-7. doi: 10.1007/s002689900089.
- Malfertheiner P, Chan FK, McColl KE. Peptic ulcer disease. Lancet 2009; 374(9699):1449-61. doi: 10.1016/ S0140-6736(09)60938-7.
- Christensen S, Riis A, Nørgaard M, Thomsen RW, Sørensen HT. Introduction of newer selective cyclo-oxygenase-2 inhibitors and rates of hospitalisation with bleeding and perforated peptic ulcer. Aliment Pharmacol Ther 2007; 25(8):907-12. doi: 10.1111/j.1365-2036.2007.03274.x.
- Kurata JH, Nogawa AN. Meta-analysis of risk factors for peptic ulcer. Nonsteroidal antiinflammatory drugs, Helico-bacter pylori, and smoking. J Clin Gastroenterol 1997; 24(1):2-17. doi: 10.1097/00004836-199701000-00002.
- Barazandeh F, Yazdanbod A, Pourfarzi F, Sepanlou SG, Derakhshan MH, Malekzadeh R. Epidemiology of peptic ulcer disease: Endoscopic results of a systematic investigation in iran. Middle East J Dig Dis 2012; 4(2):90-6.
- Sharma AK, Sharma RK, Sharma SK, Soni D, Singh TP. Double peptic perforation: Report of a rare case. Asian J Surg 2015; 38(4):239-41. doi: 10.1016/j.asjsur.2013. 04.001.
- Songne B, Jean F, Foulatier O, Khalil H, Scotté M. Non operative treatment for perforated peptic ulcer: Results of a prospective study. Ann Chir 2004; 129(10):578-82. doi: 10.1016/j.anchir.2004.06.012.
- Paspatis GA, Dumonceau JM, Barthet M, Meisner S, Repici A, Saunders BP, et al. Diagnosis and management of iatrogenic endoscopic perforations: European society of gastrointestinal endoscopy (ESGE) position statement. Endoscopy 2014; 46(8):693-711. doi: 10.1055/s-0034- 1377531.
- Hill AG. Management of perforated duodenal ulcer. In: Holzheimer RG, Mannick JA, editors. Surgical treatment: Evidence-based and problem-oriented. Munich: zuckschwerdt; 2001. Available from: https://www.ncbi.nlm. nih.gov/books/NBK6926.