Cutaneous T-cell Lymphoma Predisposing to Recurrent Infective Endocarditis by Methicillin-resistant Staphylococcus Aureus (MRSA) in a Patient with Intracardiac Defibrillator (ICD)
By Muhammad Azam Shah1, Muhammad Adil Soofi1, Faisal Alsmadi1, Muhammad Amin Ur Rehman2, Faisal Abdullah Alghamdi1Affiliations
doi: 10.29271/jcpsp.2022.08.S95ABSTRACT
Cutaneous T-cell lymphoma (CTCL) is a rare group of extra-nodal non-Hodgkin's lymphomas resulting in infiltration of the skin by the malignant cells. Sézary syndrome (SS) and mycosis fungoides (MF) are the most common subtypes, and infectious complications are the major cause of death in such patients. The presence of implantable cardiac devices (ICD) and CTCL make the patient more vulnerable to the device-related infective endocarditis (IE) caused by methicillin-resistant staphylococcus aureus (MRSA). The need for reimplantation of ICD should be assessed in detail and non-cardiac conditions should be considered while making such decisions. Herein, we report a unique case of non-ischemic cardiomyopathy with an implantable cardiac defibrillator (ICD), who later developed CTCL, complicated by the recurrent right-sided IE which is caused by MRSA.
Key Words: Cutaneous T-cell lymphoma, Methicillin-resistant staphylococcus aureus (MRSA), Infective endocarditis.
INTRODUCTION
Cutaneous T-cell lymphoma (CTCL) is a rare group of extra-nodal non-Hodgkin's lymphomas resulting in infiltration of the skin by the malignant cells. Sézary syndrome (SS) and mycosis fungoides (MF) are the most common subtypes of CTCL, comprising of two-thirds of the total cases.1 Infectious complications are the major cause of death in the patient suffering from CTCL with the skin being the most common site of involvement.2
Infective endocarditis (IE) is associated with the significant morbidity and mortality. The rate of infection of implantable cardiac devices varies but mostly ranges from 0.2% to 3.7%.3 Here, we report a unique case of non-ischemic cardiomyopathy with an implantable cardiac defibrillator (ICD), which later developed CTCL, complicated by recurrent right-sided IE which is caused by methicillin-resistant staphylococcus aureus (MRSA).
CASE REPORT
A 63-year male, known case of non-ischemic cardiomyopathy with the left ventricular ejection fraction (LVEF) of 20-25% for the last five years and with dual-chamber ICD implanted for the primary prevention, started noticing dark discoloration of whole skin with scaly changes about one year back. He was referred to the dermatologist, who based on his skin changes and biopsy, labeled him as SS with large cell transformation. His biopsy showed parakeratosis and mild spongiosis. There were atypical small and large CD3 positive lymphocytes. Overall histologic and immunohistochemical features suggested the diagnosis of MF/SS with the large cell transformation (Figure 1). About six months back, he was admitted with an acute decompensated heart failure. On workup, he was found to have multiple large vegetations on ICD lead and positive blood cultures for MRSA. Both lead and device were extracted, and intravenous (IV) vancomycin was given for 6 weeks. During the same admission, the patient had multiple runs of sustained ventricular tachycardia without cardiac arrest which led to the decision of second ICD (single chamber) implantation on the right side. He was discharged in stable condition about four months ago.
On his current admission, he presented to the emergency with the complaints of exertional dyspnea NYHA functional class III/IV with orthopnea and paroxysmal nocturnal dyspnea for the two weeks, associated with the low-grade fever with lethargy and fatigability.
Table I: Blood investigations during the admission.
|
Parameters |
Unit |
At admission |
After one month |
After two months |
On the day of demise |
|
White blood cell count |
×109/L |
8.07 |
7.87 |
9.43 |
13.94 |
|
Hemoglobin |
g/dl |
10.0 |
9.7 |
8.7 |
7.7 |
|
Platelets |
×109/L |
234 |
239 |
104 |
65 |
|
Serum creatinine |
umol/L |
249 |
101 |
218 |
263 |
|
Urea |
umol/L |
23.8 |
10.7 |
18.8 |
30.7 |
|
Sodium |
umol/L |
131 |
128 |
123 |
127 |
|
Potassium |
umol/L |
5.08 |
2.80 |
5.63 |
5.78 |
|
Total bilirubin |
umol/L |
41.4 |
38.9 |
179 |
236 |
|
Alanine aminotransferase (ALT) |
U/L |
93 |
26 |
62 |
148 |
|
Alkaline phosphatase |
U/L |
372 |
181 |
183 |
141 |
|
Serum albumin |
g/L |
25.4 |
22.9 |
18.8 |
20.2 |
|
INR |
|
1.86 |
1.26 |
4.72 |
5.9 |
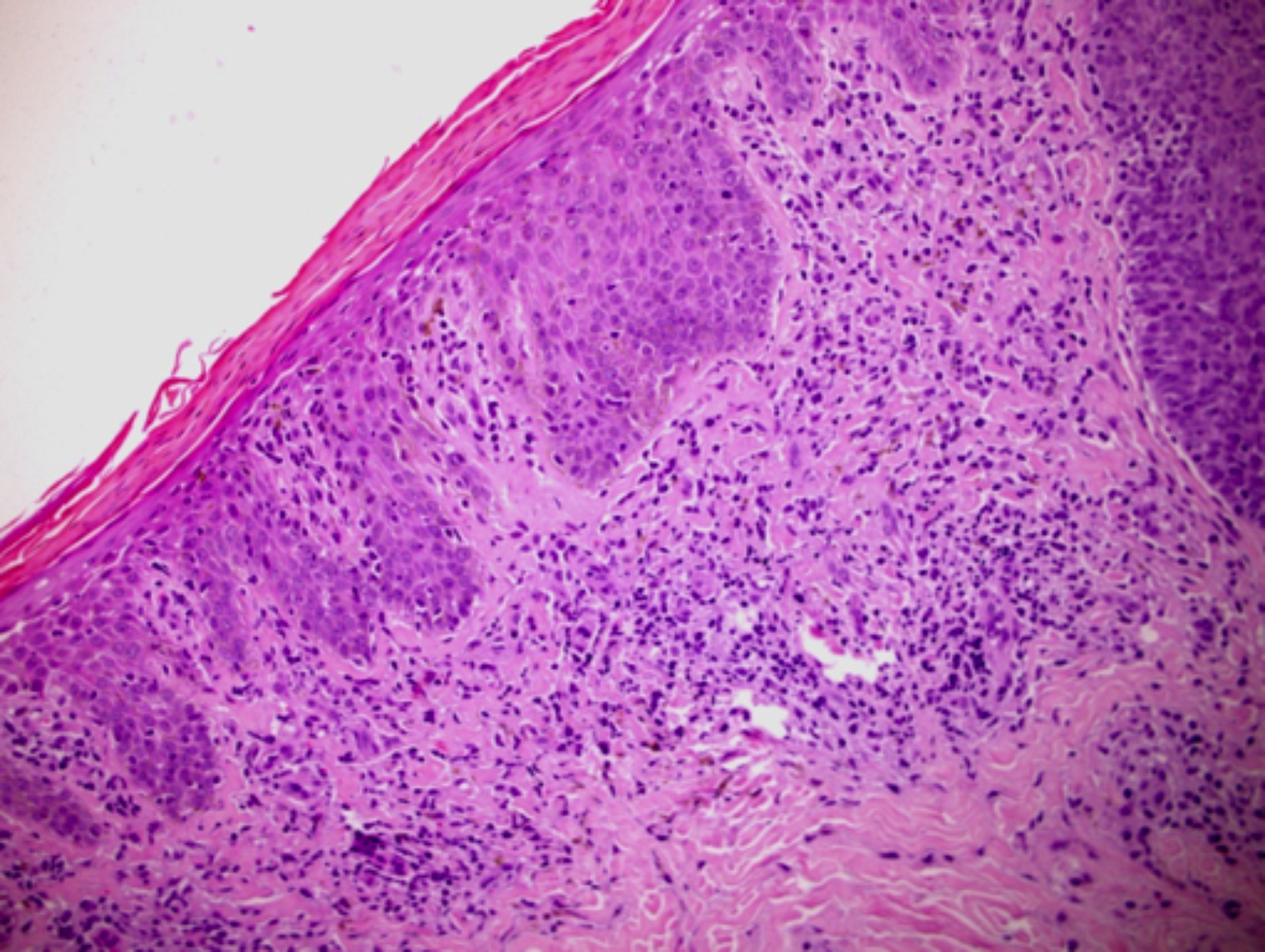 Figure 1: Skin biopsy of the patient showing changes suggestive of cutaneous T-cell lymphoma.
Figure 1: Skin biopsy of the patient showing changes suggestive of cutaneous T-cell lymphoma.
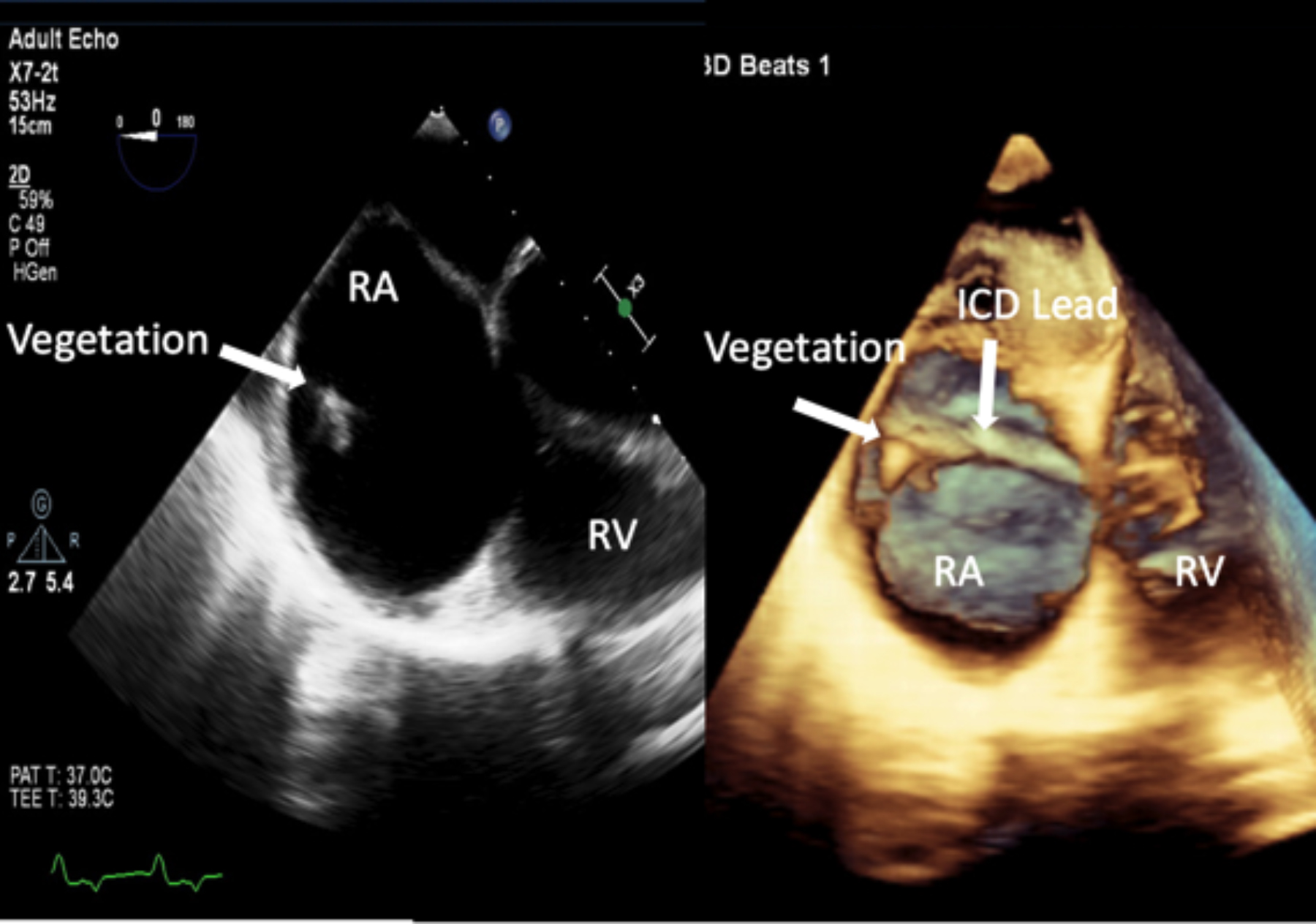 Figure 2: Trans-esophageal 2-D (left) and 3-D live (right) echocardiography at 0 degrees showing a mass (vegetation) attached to the implantable cardiac device lead in the right atrium.
Figure 2: Trans-esophageal 2-D (left) and 3-D live (right) echocardiography at 0 degrees showing a mass (vegetation) attached to the implantable cardiac device lead in the right atrium.
Transthoracic echocardiography showed the left ventricle to be severely dilated with an ejection fraction of 20%. Three consecutive blood cultures showed MRSA. The patient was started on vancomycin (1 gram, twice a day) and rifampicin (300 mg, twice a day IV) based on sensitivity, and the dose was adjusted later according to the drug levels. Transesophageal echocardiography was done which showed vegetation attached to the ICD lead in the right atrium (Figure 2). ICD was removed as per the recommendation of the infectious disease team.
The patient remained hypotensive and congested over the coming weeks with an increased dependency on inotropes and oxygen. The subsequent blood cultures showed growth of Enterobacter cloacae and Staphylococcus capitis. Rifampicin was given for two weeks and later replaced by Piperacillin/tazobactam (3.37 grams twice a day), and vancomycin was continued. Over the next four weeks, the patient kept on deteriorating with higher dependency on inotropic support and continued to be septic despite broad-spectrum antibiotics. His renal and liver functions started to deteriorate (Table I). Subsequently, he had a brief respiratory arrest followed by the mechanical ventilation. Inotropic support was maximized, but the patient could not recover from the shock and expired.
DISCUSSION
CTCLs are a diverse group of skin neoplasms with T-cell infiltration that varies significantly in clinical presentation, histological appearance, and prognosis. The annual incidence of CTCL is about 0.5 per 100,000, and it usually affects the adult population with the median age of 55 to 60 years.4 MF and SS are the most common clinical presentations of CTCL.1 Prognosis of CTCL is poor and opportunistic infections, and immunosuppression are linked with the disease-related death.5 Skin is the most common site of infection in CTCL and Staphylococcal aureus is the most frequent pathogen involved and rates of MRSA infections are higher in CTCL than in other skin conditions.6
Cardiac device-related IE (CDIE) is defined as the detection of valvular or lead vegetations by echocardiography or if modified, Duke criteria for IE are met.7 MRSA is becoming more prevalent (about 50%) which is making treatment of CDIE more challenging.3,8
The treatment of CDIE depends upon the clinical presentation, extent of involvement, and causative organisms and requires device explantation and prolonged use (4-6 weeks) of IV antibiotics.3,8 The need for device reimplantation should be reassessed as more than one-third of the patients might not require the second device due to the change of clinical status.9 Our patient had recurrent IE by MRSA, likely due to the persistent risk posed by CTCL.
In summary, CTCLs predispose patients to the recurrent skin infections and septicemia. The presence of ICDs and CTCL makes the patient more vulnerable to the device-related IE by MRSA. The need for reimplantation of ICD should be assessed in detail, and non-cardiac conditions should be considered while making such decisions.
PATIENT’S CONSENT:
Informed consent was taken from the patient’s family to publish anonymous data.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
MAS: The primary cardiologist and responsible for writing and editing the manuscript.
MAS: Heart failure consultant and involved inpatient care.
FA: The electrophysiologist and did overall supervision of this manuscript.
MAR: Pathologist who provided data and helped in writing the manuscript.
FAA: Helped in data collection and revision of the manuscript.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Wilcox RA. Cutaneous B-cell lymphomas: 2019 update on diagnosis, risk stratification, and management. Am J Hematol 2018; 93(11):1427-30. doi: 10.1002/ajh.25224.
- Axelrod PI, Lorber B, Vonderheid EC. Infections complicating mycosis fungoides and sézary syndrome. JAMA 1992; 267(10):1354-8. doi:10.1001/jama.1992. 03480100060031.
- Persson R, Earley A, Garlitski AC, Balk EM, Uhlig K. Adverse events following implantable cardioverter defibrillator implantation: A systematic review. J Interv Card Electrophysiol 2014; 40(2):191-205. doi.org/10.1007/s10840-014- 9913-z.
- Bagherani N, Smoller BR. An overview of cutaneous T cell lymphomas. F1000Res 2016; 5(0):1882. doi.org/10.12688/ f1000research.8829.1.
- Moyal L, Feldbaum N, Goldfeiz N, Rephaeli A, Nudelman A, Weitman M, et al. The therapeutic potential of AN-7, a novel histone deacetylase inhibitor, for treatment of mycosis fungoides/sezary syndrome alone or with doxorubicin. Plos One 2016; 11(1):e0146115. doi.org/10.1371/journal. pone.0146115.
- Tsambiras PE, Patel S, Greene JN, Sandin RL, Vincent AL. Infectious complications of cutaneous t-cell lymphoma. Cancer Control 2001; 8(2):185-8. doi: 10.1177/107327 480100800213.
- Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, et al. Proposed modifications to the duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 2000; 30(4):633-8. doi: 10.1086/313753.
- Margey R, McCann H, Blake G, Keelan E, Galvin J, Lynch M, et al. Contemporary management of and outcomes from cardiac device-related infections. Europace 2010; 12(1): 64-70. doi: 10.1093/europace/eup362.
- Sohail MR, Uslan DZ, Khan AH, Friedman PA, Hayes DL, Wilson WR, et al. Management and outcome of permanent pacemaker and implantable cardioverter-defibrillator infections. J Am Coll Cardiol 2007; 49(18): 1851-9. doi: 10.1016/j.jacc.2007.01.072.