Cutaneous Metastasis from Transitional Cell Carcinoma of Urinary Bladder
By Goknur Kalkan1, Hilal Ahsen2, Bulent Yalcin3Affiliations
doi: 10.29271/jcpsp.2022.04.58ABSTRACT
Cutaneous metastases with a prevalence of 5.3% in all malignancies are rarely observed phenomena in dermatology. Bladder cancers constitute 0.84% of cutaneous metastases; and 90% of these are transitional cell carcinomas (TCCs), the commonest bladder malignancy. However, these metastatic cutaneous lesions are notorious for mimicking many dermatological disorders and show poor prognosis. Herein, we report a 51-year male patient who presented with fibrotic or sclerodermoid type lesions on his both legs and trunk due to cutaneous metastases of bladder urothelial carcinoma. We would like to call attention to these rarely observed skin lesions to prevent delayed diagnosis; and emphasise the use of immunohistochemical staining for the determination of the primary origin of the tumour.
Key Words: Cutaneous metastasis, Bladder, Urothelial carcinoma.
INTRODUCTION
Cutaneous metastases with a prevalence of 5.3% in all malignancies are rarely observed phenomena in dermatology. Bladder cancers constitute 0.84% of cutaneous metastases; and 90% of these are transitional cell carcinomas (TCCs), the most common type of bladder cancer, also called urothelial carcinoma. However, these metastatic cutaneous lesions are particularly notorious for mimicking many sorts of dermatological disorders and show poor prognosis.1-3 Here, we report a 51-year male patient who presented with fibrotic or sclerodermoid-type lesions on his both legs and trunk due to cutaneous metastases of bladder urothelial carcinoma.
CASE REPORT
A 51-year male patient with metastatic bladder carcinoma was hospitalised in the Department of Oncology for further examination and treatment. Dermatological examination revealed firm, indurated, widespread, purple-violaceous colour plaque lesions on both the lower limbs and abdomen of the patient (Figures 1 and 2). The lesions were firm in consistency on palpation.
 Figure 1: Firm, indurated, livedoid lesions on the lower limb.
Figure 1: Firm, indurated, livedoid lesions on the lower limb.
 Figure 2: Firm, infiltrated plaque on the abdomen.
Figure 2: Firm, infiltrated plaque on the abdomen.
The patient also described concurrent limited mobility in his legs. The lesions had appeared several months back. Histopathology of the lesions was consistent with urothelial carcinoma metastasis (Figure 3). Immunohistochemical studies revealed that neoplastic cells were stained diffusely positive with CK7 (Figure 4), CK20, HMW-CK and GATA3, and focally positive with p63 (Figure 5).
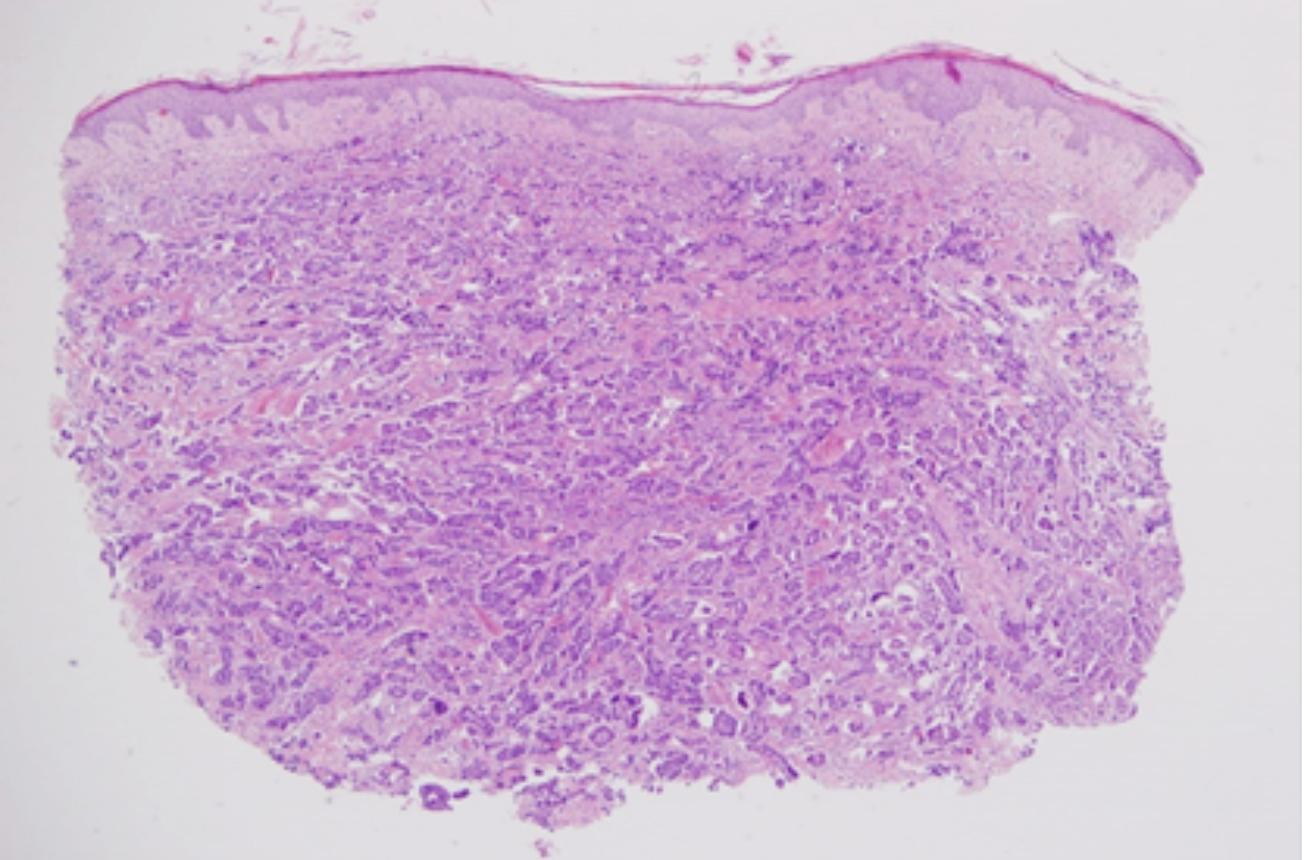 Figure 3: Histopathological examination of the lesions consistent with urothelial carcinoma metastasis (H&E, ×4).
Figure 3: Histopathological examination of the lesions consistent with urothelial carcinoma metastasis (H&E, ×4).
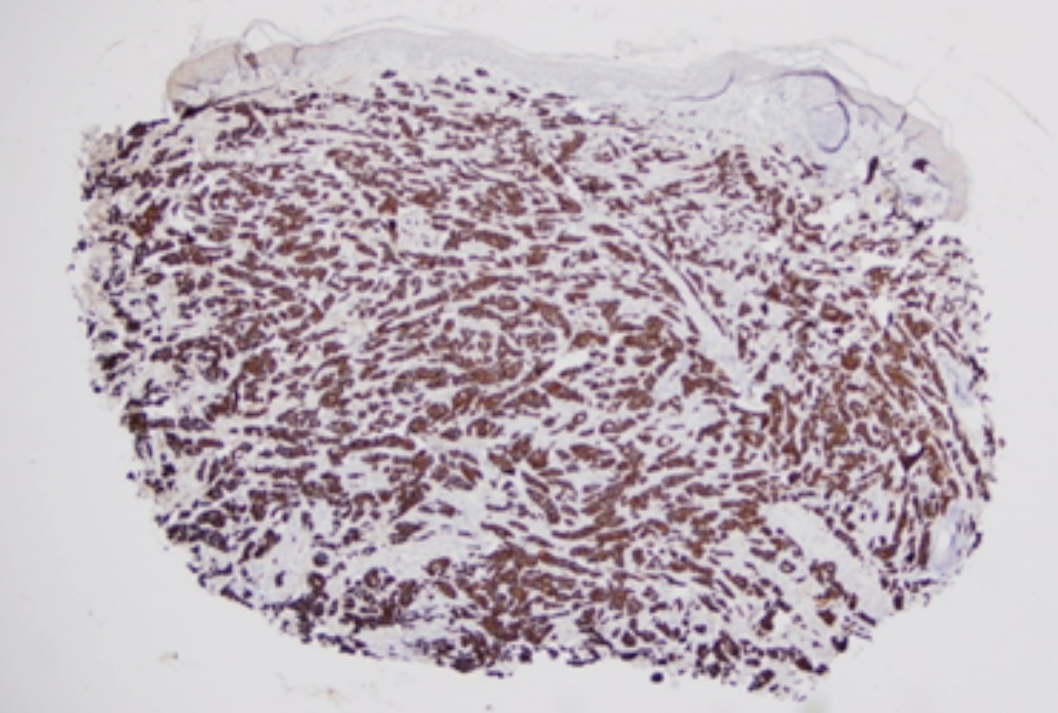 Figure 4: Immunohistochemical staining showing diffuse positivity with CK7.
Figure 4: Immunohistochemical staining showing diffuse positivity with CK7.
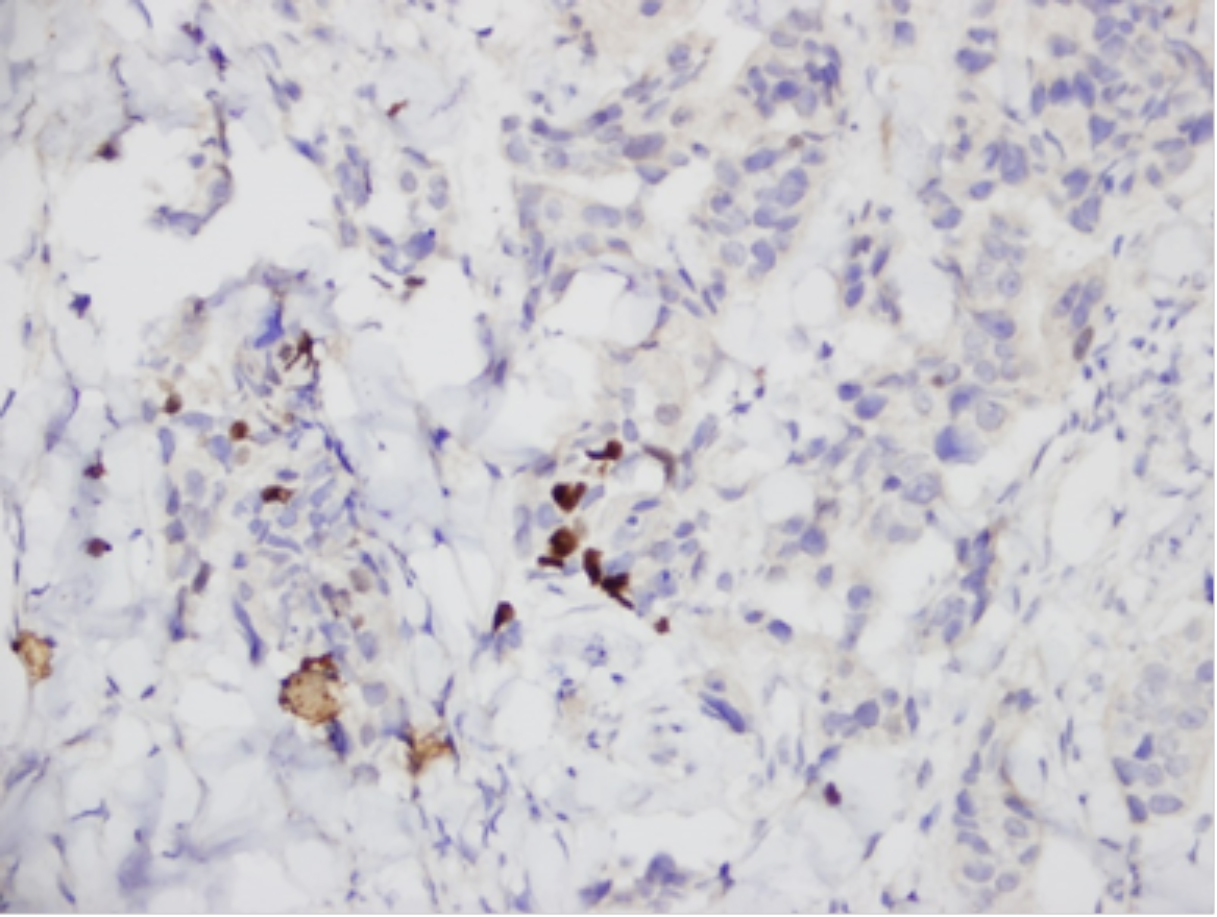 Figure 5: Immunohistochemical staining showing focal positivity with p63.
Figure 5: Immunohistochemical staining showing focal positivity with p63.
The patient was previously diagnosed with urothelial carcinoma on excisional biopsy of the lymphadenopathy detected in the right inguinal region that was reported consistent with urothelial carcinoma metastasis. The patient was treated with a total of 6 cycles of carboplatin + gemcitabine. The patient had no family history of cancer.
DISCUSSION
Clinical diversity of cutaneous urothelial carcinoma metastases makes it difficult to make a correct diagnosis. Firstly, the clinician should suspect the diagnosis of metastasis and then confirm it by histopathologic evaluation. In cases of unknown primary, immunohistochemical panel for urothelial carcinoma; CK7, CK20, HMW-CK, GATA3 and p63 should be performed.4-6 In our case, immunohistochemical studies showed neoplastic cells diffusely staining positive with CK7, CK20, HMW-CK and GATA3, and focally positive with p63.
Cutaneous metastases may clinically resemble the primary tumour. However, they are often poorly differentiated.2,4 These metastatic cutaneous lesions are grouped as nodular type, inflammatory type and fibrotic or sclerodermoid type by Mueller et al., according to the clinical appearances.1 Besides, these metastatic lesions can also resemble furuncles, erysipelas, cellulitis, herpes zoster and sebaceous cysts and mimic many common dermatologic disorders.2,4,7 The metastatic cutaneous lesions of our patient were grouped as fibrotic/sclerodermoid type because of the firm, infiltrated, purple-violaceous colour plaque-like appearance on both lower limbs and abdomen.
There are some diseases that should be considered in the differential diagnosis of such a patient. Gemcitabine is a chemotherapeutic agent used for the treatment of locally advanced and metastatic TCC of the bladder. Scleroderma-like lesions on the lower extremities associated with gemcitabine are also reported; and we should consider this in the differential diagnosis. The fibrotic changes in the skin resolve after the cessation of gemcitabine in such cases.8 Gemcitabine-associated acute lipodermatosclerosis should also be included in the differential diagnosis. Clinically, erythematous and tender plaques of the lower extremities accompanied by edema; and induration are observed.9 However, scleroderma-like lesions in the skin of the case presented here, were not related to the initiation and discontinuation of gemcitabine therapy. Scleroderma-like changes in the patient's skin were present at the patient's first admission, independent of gemcitabine treatment. As a result of histopathology and immunohistochemistry, we excluded these differential diagnoses.
Paraneoplastic syndromes of ovarian carcinoma also include scleroderma-like dermatologic disorders. There are case reports of cutaneous metastases from mucinous ovarian carcinoma presenting with a morphea-like appearance on the breasts.10
Since cutaneous metastases from genitourinary cancers are rarely encountered, we present this case of an infrequently observed sclerodermoid type of cutaneous metastasis. We think that the differential diagnosis of a new-onset cutaneous lesion with a previous history of bladder cancer should include cutaneous metastasis to avoid misdiagnosis caused by patient and physician carelessness. The clinician should be particularly vigilant in evaluating these lesions that have extremely variable appearances and have poor prognosis. The use of immunohistochemical staining for the determination of the primary origin of the tumour should be kept in mind.
PATIENT’S CONSENT:
The consent of the patient was taken prior to the writing of the manuscript.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
GK, HA, BY: Contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of the data for the work; drafting the work or revising it critically for important intellectual content; and final approval of the version.
REFERENCES
- Mueller TJ, Wu H, Greenberg RE, Hudes G, Topham N, Lessin SR, et al. Cutaneous metastases from genitourinary malignancies. Urology 2004; 63(6):1021-6. doi: 10.1016/j. urology.2004.01.014.
- Pastore AL, Palleschi G, Fuschi A, Velotti G, Leto A, Yazan Al Salhi Y, et al. Unusual presentation of cutaneous metastasis from bladder tumour: Two case reports of rare implantation. Ann Surg Perioper Care 2016; 1(3):1016.
- Kerkeni W, Ayari Y, Charfi L, Bouzouita A, Ayed H, Cherif M, et al. Transitional bladder cell carcinoma spreading to the skin. Urol Case Rep 2017; 11:17-8. doi: 10.1016/j.eucr. 2016.11.028.
- Campanati A, Brisigotti V, Dusi D, Giuliodori K, Racchini S, Criante P, et al. Bladder urothelial cell carcinoma metastatic to the skin. Clin Dermatol 2013; 1(1):22-5.
- Akman Y, Cam K, Kavak A, Alper M. Extensive cutaneous metastasis of transitional cell carcinoma of the bladder. Int J Urol 2003; 10(2):103-4. doi: 10.1046/j.1442-2042.2003. 00571.x.
- McKenney JK, Amin MB. The role of immunohistochemistry in the diagnosis of urinary bladder neoplasms. Semin Diagn Pathol 2005; 22(1):69-87. doi: 10.1053/j.semdp.2005. 11.005.
- Zangrilli A, Saraceno R, Sarmati L, Orlandi A, Bianchi L, Chimenti S. Erysipeloid cutaneous metastasis from bladder carcinoma. Eur J Dermatol 2007; 17(6):534-6. doi: 10. 1684/ejd.2007.0271.
- Bessis D, Guillot B, Legouffe E, Guilhou JJ. Gemcitabine-associated scleroderma-like changes of the lower extremities. J Am Acad Dermatol 2004; 51(2 Suppl): S73-6. doi: 10.1016/j.jaad.2001.07.001.
- Mittal A1, Leventhal JS. Gemcitabine-associated acute lipodermatosclerosis like eruption: An under recognised phenomenon. JAAD Case Rep 2017; 3(3):190-5. doi: 10. 1016/j.jdcr.2017.02.014.
- McDonald HH, Moore MR, Meffert JJ. Cutaneous metastases from adenocarcinoma of the ovary. JAAD Case Rep 2016; 2(5):406-7. doi: 10.1016/j.jdcr.2016.08.010.