Contralateral Recurrence of a Lumbar Juxtafacet Cyst Following Spontaneous Resolution
By Can Sarica1, Furkan Kucuk2Affiliations
doi: 10.29271/jcpsp.2022.04.85ABSTRACT
We present a patient who had spontaneous resolution of a right L3/4 lumbar juxtafacet cyst (LJFC); and in whom, 2.5 years after regression of the previous cyst, a new contralateral L3/4 LJFC developed. Furthermore, with an extensive review, we discuss the selection criteria for patients for conservative treatment. A 44-year woman presented with right leg pain for two months. Neurological examination findings were normal; however, hypoesthesia was observed in right L4. There was no medical history of any trauma or a specific condition. Magnetic resonance imaging (MRI) revealed a right L3/4 LJFC and L4/5 spondylolysis. The patient refused surgical treatment and was referred to a physical therapy department. A non-steroidal anti-inflammatory drug was administered for four weeks. At two months’ follow-up, her leg pain was relieved. After 2.5 years, she was readmitted due to radiating left leg pain. The MRI showed regression of the previous right L3/4 LJFC and a newly formed left L3/4 LJFC. Thus, cyst excision and posterior fusion were performed. The symptoms were resolved immediately following the surgery and the patient continued to be symptom-free at a one-year follow-up. In the setting of significant instability, conservative treatment for LJFCs can still be beneficial; however, its role in preventing recurrence of LJFCs may be inadequate. In such patients, early surgical correction of instability may result in better long-term outcomes.
Key Words: Degeneration, Juxtafacet cyst, Recurrence, Spinal instability, Spontaneous resolution.
INTRODUCTION
Spontaneous resolution of lumbar juxtafacet cysts (LJFCs) with conservative treatment (non-steroidal anti-inflammatory drugs, physical therapy, and brace) is well known; however, optimum selection criteria for patients for conservative treatment are still debatable. Several studies on the spontaneous resolution of LJFCs lack long-term follow-up data, indicating that we do not have any clue whether and in which condition these spontaneously resolved cysts recur.1-7 Therefore, we proposed that severe degenerative and unstable spines are poor candidates for such treatment strategies; and have presented it as a case report.
Here, we present a patient who had spontaneous resolution of a right L3/4 LJFC, which was associated with L4/5 degenerative spondylolisthesis, and in whom, 2.5 years after regression of the previous cyst, a new contralateral L3/4 LJFC developed, which was then surgically treated. Furthermore, with an extensive review of cases of spontaneously resolved cysts, we further discuss the treatment strategies for LJFCs.
CASE REPORT
A 44-year woman presented with progressively increasing pain in the right hip and leg for two months. Physical and neurological examination findings were normal; however, hypoesthesia was observed in the right L4. There was no medical history of any trauma or a specific condition. Magnetic resonance imaging (MRI) revealed a right L3/4 LJFC and L4/5 Meyerding grade 1 spondylolisthesis (Figure 1a-b). For personal reasons, the patient refused surgical treatment and was referred to the physical therapy department of the same hospital. A non-steroidal anti-inflammatory drug was administered for four weeks. At two months’ follow-up, leg pain was relieved; however, back pain persisted intermittently despite the administration of analgesics. After 2.5 years, the patient was readmitted due to radiating left leg pain. The MRI showed regression of the previous right L3/4 LJFC and a newly formed left L3/4 LJFC (Figure 1c-d). Surgical excision of the cyst was planned. Preoperative computed tomography revealed bilateral L4 pars interarticularis defect (Figure 2a). The cyst wall was not calcified, and there was minimal bone erosion adjacent to the cyst (Figure 2b). Cyst resection and posterior fusion with transpedicular screws were performed (Figure 2e-f). Intraoperatively, the facet was hypertrophic, and the cyst was macroscopically non-differentiable from the surrounding bony and ligamentous structures. Additionally, the cyst was strongly attached to the dura mater. The pathology was consistent with that of a synovial cyst.
Table I: MacNab clinical outcome score.|
Grade |
Definition |
|
Excellent |
No pain; no restriction of activity |
|
Good |
Occasional back or leg pain of sufficient severity to interfere with the patient's ability to do his normal work or his capacity to enjoy himself in his leisure hours |
|
Fair |
Improved functional capacity, but handicapped by intermittent pain of sufficient severity to curtail or modify work or leisure activities |
|
Poor |
No improvement or insufficient improvement to enable increase in activities; further operative intervention required |
Table II: Spontaneously resolved juxtafacet cysts in the literature.
|
Author |
Journal, Year |
Age, Gender |
Location |
Possible Contributing Factors |
S to A |
A to A |
Int. of MRIs |
Follow up |
Therapies |
Recur. |
|
Mercader |
Neuroradiology, 1985 |
65, F |
L4-5, Rt |
L4-5 listhesis + disc protrusion |
8 |
5 |
5 |
N/A |
NSAID, brace |
- |
|
Maezawa |
Eur Spine J, 2000 |
15, M |
L4-5, Lt |
Trauma hx |
2 |
3 |
3 |
24 |
Brace |
- |
|
Swartz |
Am J Neuroradiol, 2003 |
58, F |
L5-S1, Rt |
L5-S1 listhesis + disc protrusion |
1 |
12 |
18 |
N/A |
PT, NSAID, brace |
- |
|
Houten |
J Neurosurg Spine, 2003 |
64, M |
L4-5, Rt |
N/A |
7 |
1 |
3 |
N/A |
N/A |
- |
|
|
|
57, F |
L4-5, Lt |
N/A |
5 |
1 |
4 |
N/A |
NSAID, narcotics, gabapentin |
- |
|
|
|
58, F |
L4-5, Lt |
L3-4 fusion surgery |
18 |
4 |
4 |
N/A |
N/A |
- |
|
Illerhaus |
Fortschr Röntgenstr, 2005 |
50, F |
L4-5, Rt |
- |
12 |
7 |
7 |
N/A |
PT, NSAID |
- |
|
Ewald |
Zentralbl Neurochir, 2005 |
65,F |
L4-5, Rt |
L4-5 listhesis + disc degen. |
5 |
3 |
4 |
N/A |
PT, NSAID |
- |
|
Colen |
J Neurosurg Spine, 2006 |
58,F |
C7-T1, Rt |
- |
6 |
6 |
6 |
N/A |
N/A |
- |
|
Lee |
Kor J Spine, 2010 |
59,M |
L4-5, Rt |
L4-5 listhesis + disc degen. |
6 |
N/A |
72 |
N/A |
Facet block |
- |
|
Pulhorn |
Br J Neurosurg, 2012 |
72, F |
L4-5, Rt |
disc degen. |
N/A |
18 |
18 |
N/A |
N/A |
- |
|
Mattei |
Medical Hypotheses, 2012 |
56, F |
S1-2, Rt |
L5-S1 listhesis + disc degen. |
N/A |
1 |
13 |
N/A |
PT, NSAID |
- |
|
Kim |
J Korean Neurosurg Soc, 2015 |
58, M |
L3-4, Lt L3-4, Rt (recur) |
L3-4 listhesis |
48 |
1 |
50 |
12 |
PT, NSAID |
+
|
|
Cannarsa |
Nagoya J Med Sci, 2015 |
36, M |
L2-3, M L3-4, Rt (recur) |
Trauma hx + L3-4 listhesis |
5 |
- |
3 |
3w |
N/A |
+
|
|
Sinha |
J Surg Case Rep, 2016 |
66, M |
L5-S1, Lt |
disc degen. |
12 |
6 |
18 |
N/A |
N/A |
- |
|
Ucler |
Neurol India, 2017 |
36, F |
L4-5, Rt |
- |
10 days |
2 days |
2 days |
3 |
N/A |
- |
|
Downs |
World Neurosurg, 2018 |
60, F |
L4-5, Rt |
- |
N/A |
19 |
19 |
N/A |
Steroid Inj., RFN, Pregabalin |
- |
|
Nordmann |
World Neurosurg, 2019 |
51, F |
L4-5, Rt |
disc degen. |
N/A |
8,5 |
8 |
N/A |
PT, meloxicam, steroid |
|
|
Our Case |
2019 |
44, F |
L3-4, Rt L3-4, Lt (recur) |
L3-4 listhesis + disc degen. |
2 |
2 |
52 |
12 |
PT, NSAID |
+ |
| Degen: Degeneration; Hx: History; Listhesis: Spondilolisthesis; Rt: Right; Lt: Left; M: Middle; Inj: Injection; RFN: Radiofrequency neurotomy; NSAID: Non-steroid anti-inflammatory drugs; MRI: Magnetic resonance imaging; S to A: Interval between symptomatic to admission (months); A to A: Interval between admission to asymptomatic (months); Int of MRIs: Interval between MRI with synovial cyst to MRI without synovial cyst (months); Recur: Recurrence; PT: Physical therapy. | ||||||||||
The postoperative MRI at two months revealed that the cyst was almost totally excised except for an extremely small residue on the far lateral side of the facet joint (Figure 2c-d). The symptoms resolved immediately following the surgery, and the patient had a MacNab clinical outcome score of “Excellent” at one-year follow-up (Table I).8
DISCUSSION
We presented a case of late recurrence of LJFC on the contralateral side following spontaneously resolved right-sided LJFC. This case is clinically important because it shows that the cyst may recur even after spontaneous resolution, especially if the etiology of the cyst is not temporary but continual.
Destabilisation of the facet joints due to degenerative and/or traumatic changes seems to be a major mechanism underlying LJFC development. Most patients with LJFC have an unstable spine with abnormally excessive movements; and exhibit spondylolisthesis, accounting for 31% of all the cases. The treatment for these cysts includes conservative, percutaneous, and surgical (with/without fusion) methods. Spontaneous resolution of cysts with conservative treatments has previously been shown; and can be a viable treatment option in selected cases (Table II). We want to emphasise that the treatment options must be considered with respect to the probable etiology of the cyst. For example, conservative treatment for spontaneous resolution of a LJFC in a young patient with a recent history of trauma and without any radiological evidence of degeneration may be reasonable.9 In contrast, proposing this treatment to an LJFC patient with apparent spinal degeneration and spondylolisthesis may result in poor long-term outcomes, similar to that of our case.
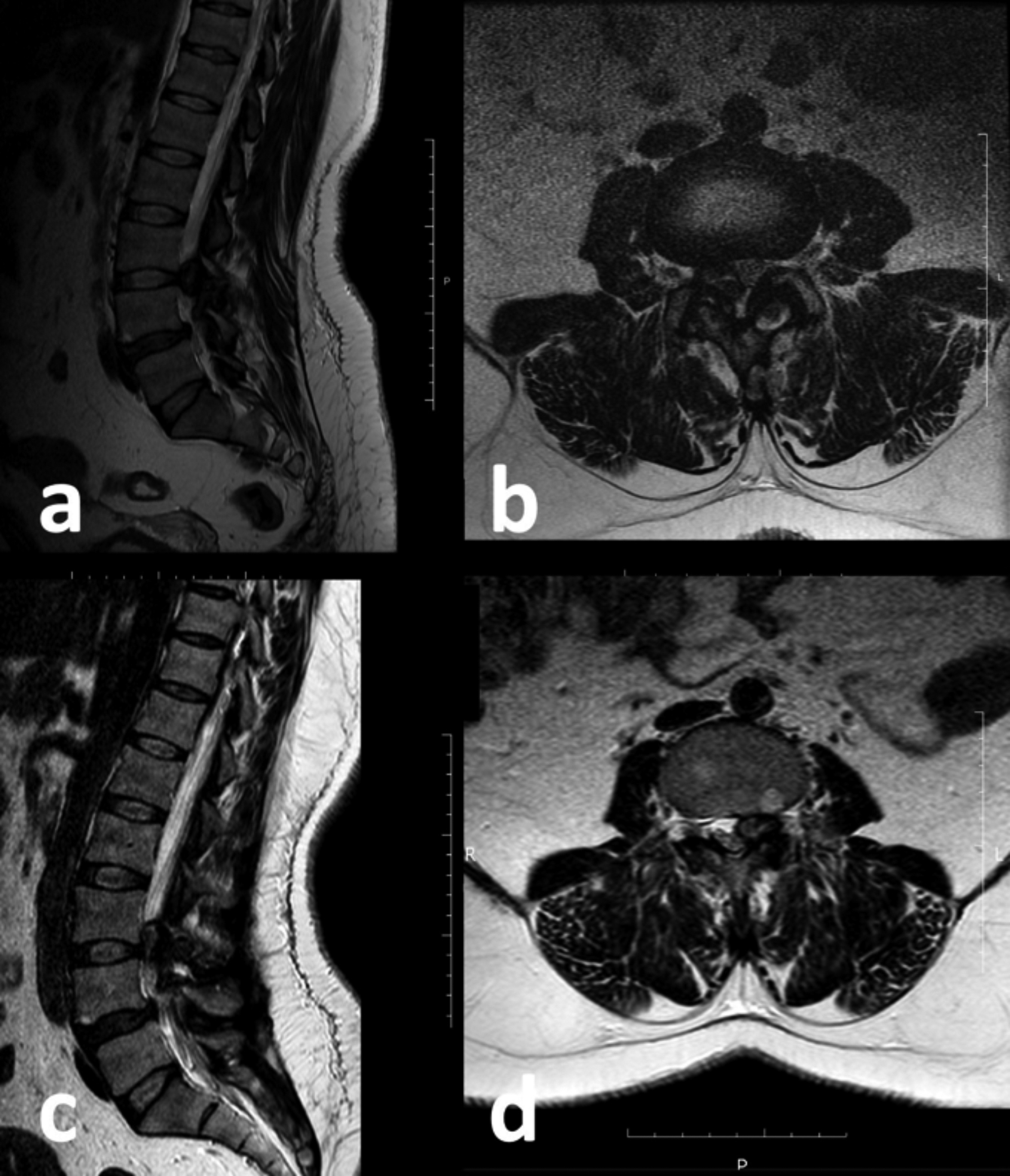 Figure 1: Sagittal (A) and axial (B) T2-weighted views of MRI at first admission showing a right L3/4 LJFC and L4/5 spondylolysis, sagittal (C) and axial (D) T2-weighted views of MRI at second admission revealing resolution of the previous right L3/4 LJFC and newly formed left L3/4 LJFC.
Figure 1: Sagittal (A) and axial (B) T2-weighted views of MRI at first admission showing a right L3/4 LJFC and L4/5 spondylolysis, sagittal (C) and axial (D) T2-weighted views of MRI at second admission revealing resolution of the previous right L3/4 LJFC and newly formed left L3/4 LJFC.
LJFC: Lumbar juxtafacet cyst; MRI: Magnetic resonance imaging.
We performed a literature review to analyse the characteristics of patients with spontaneous resolution of juxtafacet cysts (Table II).1-7,9-11 We identified 16 patients with spontaneous resolution and additional three patients with spontaneous resolution and late recurrence, including our patient. One of the most notable findings of our review was that majority of the reported cases (14/16, 87%) lacked a reported follow-up period, indicating that we know a LJFC may spontaneously resolve; however, we do not have any clue whether and when it will recur. We calculated from the studies, which clearly stated the duration of symptoms in patients with spontaneous resolution, that the interval between the onset and relief of symptoms was 13.6 ± 12.3 months (range: 12 days to 49 months); and the interval between the first admission and relief of symptoms was 5.7 ± 5.7 months (range: 2 days to 18 months). So far, three studies showed recurrence after spontaneous resolution, and all three patients in those studies had spinal degeneration; and spondylolisthesis to some extent.
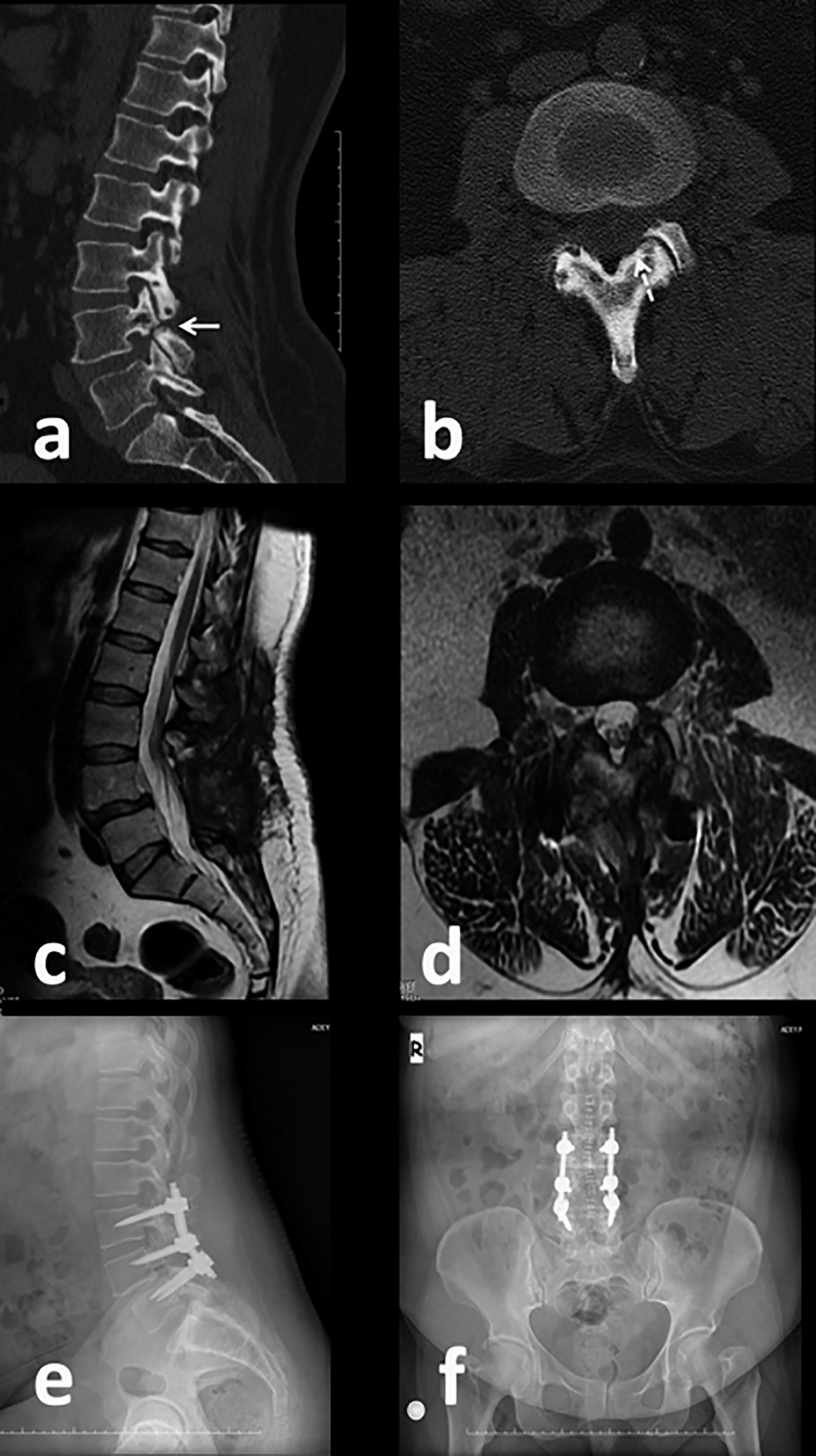 Figure 2: Sagittal (A) and axial (B) views of preoperative computed tomography showing a L4 pars interarticularis defect (arrow) with no calcification on the cyst wall and minimal bone erosion in close proximity of the cyst (dashed arrow), sagittal (C) and axial (D) T2-weighted views of postoperative MRI revealing resection of the cyst, except for a small residue on the far later side of the facet joint, lateral (E) and anteroposterior (F) spinal X-ray showing the position of the transpedicular screws.
Figure 2: Sagittal (A) and axial (B) views of preoperative computed tomography showing a L4 pars interarticularis defect (arrow) with no calcification on the cyst wall and minimal bone erosion in close proximity of the cyst (dashed arrow), sagittal (C) and axial (D) T2-weighted views of postoperative MRI revealing resection of the cyst, except for a small residue on the far later side of the facet joint, lateral (E) and anteroposterior (F) spinal X-ray showing the position of the transpedicular screws.
MRI: Magnetic resonance imaging.
Conservative treatment of a LJFC can be a viable option in a relatively stable spine. However, it may be inadequate and time-consuming in unstable spines because of the probable high recurrence rates in the long-term. Thus, a decision of early surgical stabilisation should be time-saving with better long-term outcomes for both the patient and surgical team. In selected cases for conservative treatment, a treatment deadline of 6–12 months may be reasonable.
PATIENT’S CONSENT:
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
CS: Conception and design, acquisition of data, drafting the manuscript, and critical review of the manuscript.
FK: Acquisition of data, and drafting the manuscript.
REFERENCES
- Houten JK, Sanderson SP, Cooper PR. Spontaneous regression of symptomatic lumbar synovial cysts. Report of three cases. J Neurosurg 2003; 99(2 Suppl):235-8. doi: 10.3171/ spi.2003.99.2.0235.
- Colen CB, Rengachary S. Spontaneous resolution of a cervical synovial cyst. Case illustration. J Neurosurg Spine 2006; 4(2):186. doi: 10.3171/spi.2006.4.2.186.
- Pulhorn H, Murphy M. Spontaneous resolution of a symptomatic synovial cyst of the lumbar spine. Br J Neurosurg 2012; 26(1):123-4. doi: 10.1093/jscr/rjw166.
- Mattei TA, Goulart CR, McCall TD. Pathophysiology of regression of synovial cysts of the lumbar spine: the 'anti-inflammatory hypothesis'. Med Hypotheses 2012; 79(6): 813-8. doi: 10.1016/j.mehy.2012.08.034.
- Sinha P, Panbehchi S, Lee MT, Parekh T, Pal D. Spontaneous resolution of symptomatic lumbar synovial cyst. J Surg Case Rep 2016; 2016(10):rjw166. doi: 10. 1093/jscr/rjw166.
- Downs E, Marshman LAG. Spontaneous Resolution of Lumbar Facet Joint Cyst. World Neurosurg 2018; 115: 414-6. doi: 10.1016/j.wneu.2018.04.197.
- Nordmann NJ, Michael AP, Espinosa JA. Resolution of symptomatic lumbar synovial cyst after traumatic event. World Neurosurg 2019; 128:69-71. doi: 10.1016/j.wneu.2019. 04.091.
- Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am 1971; 53(5):891-903.
- Maezawa Y, Baba H, Uchida K, Furusawa N, Kubota C, Yoshizawa K. Spontaneous remission of a solitary intraspinal synovial cyst of the lumbar spine. Eur Spine J 2000; 9(1):85-7. doi: 10.1007/s005860050016.
- Kim HS, Ju CI, Kim SW, Kim SH. Contralateral juxtafacet cyst development after the spontaneous resolution of a previous facet cyst. J Korean Neurosurg Soc 2015; 58(6):563-5. doi: 10.3340/jkns.2015.58.6.563.
- Ucler N, Ozturk S, Gulkesen A, Kaplan M. Rapid spontaneous regression of a lumbar juxta-facet cyst. Neurol India 2017; 65(2):417-8. doi: 10.4103/neuroindia. NI_596_16.