Comparative Effects of Focused and Radial Extracorporeal Shock Wave Therapies on Lateral Epicondylitis: A Randomised Sham-controlled Trial
By Seyhmus Kaplan1, Volkan Sah1, Sezai Ozkan2, Cihan Adanas2, Veysel Delen3Affiliations
doi: 10.29271/jcpsp.2023.05.554ABSTRACT
Objective: To evaluate and compare the effects of radial and focused types of extracorporeal shock wave therapy (ESWT) on lateral epicondylitis.
Study Design: A randomised sham-controlled trial.
Place and Duration of the Study: Department of Sports Medicine, Yuzuncu Yil University Hospital, Van, Turkiye, from August 2019 to April 2020.
Methodology: Patients with acute lateral epicondylitis were randomised into focused, radial, and sham ESWT groups. The ESWT was applied for three sessions at 2-4 days intervals. All the subjects were evaluated at baseline (week 0), week 5, and 13. Patient-rated tennis elbow evaluation (PRTEE) scores were used as outcome measures.
Results: At weeks 5 and 13, all PRTEE scores (pain, function, and total) were remarkably improved in the focused and radial groups (p<0.001), but not in the sham group (p>0.05). Focused ESWT was superior to radial ESWT for the change of pain scores from baseline to week 5 (18.8±13.9 vs. 11.8±9.1; p=0.026) and week 13 (17.8±13.1 vs. 11.7±10.5, p=0.084). Focused ESWT was more effective than radial ESWT for the change of function scores from baseline to weak 5 (17.9±12.5 vs. 11.2±9.5; p=0.025) and week 13 (16.9±11.6 vs. 10.7±10.1; p=0.032). Focused ESWT was superior to radial ESWT for the change of total scores from baseline to week 5 (36.7±25.9 vs. 23.0±17.2; p=0.021) and week 13 (34.7±24.3 vs. 22.4±18.5; p=0.044).
Conclusion: Focused and radial ESWT are effective in lateral epicondylitis. The focused ESWT is superior to the radial ESWT. Thus, focused ESWT should be preferred in lateral epicondylitis.
Key Words: Lateral epicondylitis, Shock wave, Randomised sham-controlled trial.
INTRODUCTION
Lateral epicondylitis is the most common reason for painful lateral elbow caused by degeneration and inflammation of the extensor tendons on the lateral forearm. It is associated with female gender, smoking, dominant hand, diabetes mellitus, and older age.1 It can be diagnosed clinically with a physical examination, including painful lateral elbow and pain reproduction with resisted wrist dorsiflexion, and radiologically by ultrasonography and magnetic resonance imaging.2 Non-operative treatment options include nonsteroidal anti-inflammatory drugs, extracorporeal shock waves, physiotherapy and activity modification, bracing, acupuncture, and biotherapies such as autologous blood and platelet-rich plasma.3
Extracorporeal shock wave therapy (ESWT), a commonly used alternative treatment option for lateral epicondylitis, is a non-invasive, drug-free, and effective method in musculoskeletal disorders.3,4 In managing lateral epicondylitis, ESWT is usually used as a supplement to exercise programs or is recommended when the other conservative treatments fail.5 However, many ESWT parameters like types of used waves need to be investigated to determine the most appropriate protocol.6
There are three types of waves (focused, planar, and radial) that are created in ESWT generators.7 They are different from each other in terms of penetration depth and working principles.8 For instance, energy flux density (acoustic pressure) reaches the maximum level at the tip of the applicator with radial waves, while it is highest at the targeted deep tissue with focused waves (Figure 1).7,8 However, it is not clear which of these waves is more efficacious in the clinical practice.
To date, both the focused and radial types of ESWT have been used in lateral epicondylitis. However, reviews findings on the effectiveness of ESWT and ESWT types in cases with the lateral epicondylitis are conflicting.4,9,10 Moreover, reports addressing the comparative effects of ESWT types for the management of lateral epicondylitis are limited and have contradictory results.11,12 For these reasons, in this study, the authors wanted to test two hypotheses. Firstly, ESWT can improve participants’ pain and function scores in lateral epicondylitis. Secondly, ESWT types' effectiveness can differ from each other in the lateral epicondylitis. Accordingly, the study's objective was to evaluate and compare the effectiveness of radial and focused ESWT types on lateral epicondylitis.
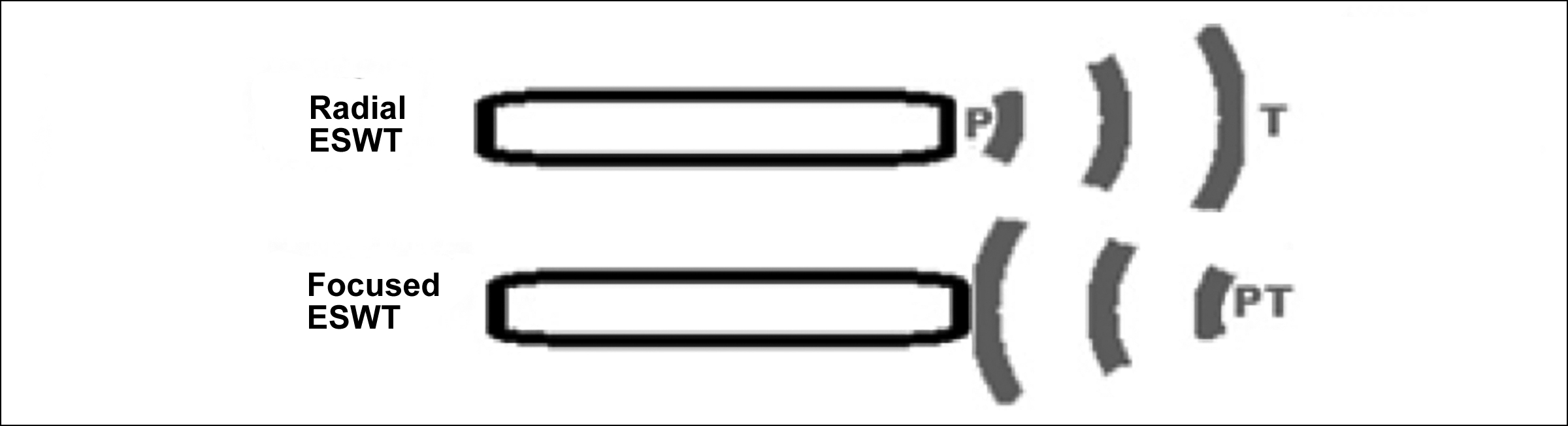 Figure 1: The main differences between radial and focused ESWT.
Figure 1: The main differences between radial and focused ESWT.
Extracorporeal shock wave therapy; P: Maximum acoustic pressure point; T: Targeted tissue.
METHODOLOGY
This study was conducted at the Department of Sports Medicine, Yuzuncu Yil University Hospital, Van, Turkiye, between August 2019 and April 2020. An investigator-blinded, prospective, randomised, and placebo-controlled trial was designed. The study obtained ethics approval from the University Ethical Review Board (Decision No: 16; Date: August 6, 2019), and the patients gave consent upon being informed. The trial followed the rules of the Declaration of Helsinki. The trial was confirmed on ClinicalTrials.gov with the data of NCT04838002.
The diagnosis of lateral epicondylitis was noted, based on clinical assessment (painful lateral elbow) and physical examination including exacerbation of the pain by resisted wrist extension.2
Patient-rated tennis elbow evaluation (PRTEE) questionnaire was used to evaluate end-point measures. This questionnaire was specifically developed for patients with lateral epicondylitis and was used to determine forearm pain and disability related to the condition. The PRTEE is a 15-item questionnaire that assesses a patient's pain (5 items) and activity difficulties (10 items; 6 items for specific activities and four items for usual activities) related to the lateral epicondylitis. These subscales (pain and function) affect the total score equally. Overall, getting a minimum of 0 and a maximum of 100 points is possible. Higher scores represent a higher level of pain and disability. The Turkish version of the PRTEE scale has been validated by Altan et al.13
Before starting the trial, a sample size was calculated based on the statisticians' advice.14 The calculations were made on the G*Power statistical program (version 3.1.9.7). For a study including three groups, power of 90%, an effect size of 0.4, and a 5% type 1 (α) error, each of the three subgroups needed a minimum of 28 cases.
Taking into account possible loss to follow‐up, a total of 97 cases with the lateral epicondylitis were randomised into three groups according to the wave models to be applied. For randomisation, sequentially numbered three cards were used (one card for each group). For each patient, one of the cards was drawn. The same ESWT device was applied in all the applications (Elettronica Pagani, Italy). The instrument has electro-pneumatic equipment, and its emission modes provide both focused and radial waves.
Patients were required to; have a new diagnosis of lateral epicondylitis, acute lateral epicondylitis (symptom duration <3 months), aged ≥18 years during the diagnosis, and have filled out the pre- and post-ESWT assessment process. If a case had both elbows affected, the elbow with a higher pain level was initially accepted for the analysis.
Abnormal elbow anatomy, pregnancy, malignancy, infection, implanted devices, cooperation disorders, and clotting diseases. Moreover, cases with symptom duration >3 months, patients with any experience with ESWT, and subjects who had injective therapies before recruitment were excluded.
All patients were contacted by telephone two times a month to increase their participation. In addition, to improve the treatment adherence, a short theoretical explanation of the importance of the study was given to all groups.
The lateral epicondylitis protocol was selected by the user's manual of the device. Accordingly, applications for each session of different ESWT types were as follows: Focused ESWT (4 Hz, 1.5 Bar, 500 pulse, 0.02-0.60 mj/mm2 for 2 minutes and 5 seconds + 8 Hz, 1.7 Bar, 1800 pulse, 0.02-0.60 mj/mm2 for 3 minutes and 45 seconds); Radial ESWT (4 Hz, 1.2 Bar, 500 pulse, 0.144 mJ/mm2 for 2 minutes and 5 seconds + 8 Hz, 1.5 Bar, 1800 pulse, 0.180 mJ/mm2 for 3 minutes and 45 seconds); Sham ESWT (1 Hz, 1 Bar, 500 pulse for 2 minutes and 5 seconds + 1 Hz, 1 Bar, 1800 pulse for 3 minutes and 45 seconds).
The treatment area on the lateral elbow was determined to be the most painful localisation with palpation. The ESWT was applied for three sessions, 2-4 days intervals (excluding weekends), in a sitting position. All the cases were examined at baseline (week 0), one month after the completion of therapy (week 5), and three months after the completion of therapy (week 13).
Statistical analyses were done by the SPSS v20 program (IBM Corp., Armonk, NY, USA). The Kolmogorov-Smirnov test was used to evaluate whether variables were normally distributed. The paired t-test was used for normally distributed dependent variables. The One-Way ANOVA with the Bonferroni test was used to compare three independent variables with a normal distribution. Some change scores in the sham group were non-normally distributed: pain (baseline - week 5), function (baseline - week 5), function (baseline - week 13), and total (baseline - week 5). Therefore, the statistical comparisons used the Mann-Whitney U test for these variables. The Student t-test compared two independent variables with a normal distribution.
Categorical variables were analysed using the Pearson chi-square test, and were expressed as numbers and percentages. Continuous variables were shown as mean ± standard deviation (min-max). The value of p<0.05 values were accepted as statistically meaningful.
Table I: Statistical analyses for PRTEE pain, function and total scores.
|
The PRTEE Scores |
Focused ESWT (n=30) |
Radial ESWT (n=29) |
Sham ESWT (n=28) |
p |
|
Pain (baseline) |
37.6±9.3 (18 – 50) |
38.3±7.8 (23 – 50) |
36.5±11.3 (17 – 50) |
0.755 |
|
Pain (week 5) |
18.8±11.1 (5 – 48) |
26.6±8.9 (7 – 43) |
35.1±12.0 (13 – 50) |
|
|
Pain (week 13) |
19.8±10.5 (5 – 49) |
26.6±9.6 (5 – 44) |
35.5±12.0 (10 – 50) |
|
|
p (baseline vs. week 5) |
<0.001 |
<0.001 |
0.330 |
|
|
p (baseline vs. week 13) |
<0.001 |
<0.001 |
0.442 |
|
|
Function (baseline) |
37.5±9.0 (16 – 50) |
35.6±11.0 (10 – 50) |
35.6±13.7 (5 – 50) |
0.769 |
|
Function (week 5) |
19.6±11.0 (5 – 48) |
24.5±10.1 (5 – 43) |
33.8±14.6 (5 – 50) |
|
|
Function (week 13) |
20.6±10.0 (8 – 47) |
25.0±10.6 (5 – 45) |
35.1±14.2 (5 – 50) |
|
|
p (baseline vs. week 5) |
<0.001 |
<0.001 |
0.243 |
|
|
p (baseline vs. week 13) |
<0.001 |
<0.001 |
0.678 |
|
|
Total (baseline) |
75.1±18.0 (34 – 100) |
74.0±17.7 (39 – 100) |
72.1±24.2 (29 – 100) |
0.846 |
|
Total (week 5) |
38.5±22.0 (10 – 96) |
51.0±18.6 (12 – 86) |
69.0±26.1 (23 – 100) |
|
|
Total (week 13) |
40.4±20.4 (13.5 – 96.5) |
51.6±19.3 (10 – 89) |
70.6±25.6 (27 – 100) |
|
|
p (baseline vs. week 5) |
<0.001 |
<0.001 |
0.245 |
|
|
p (baseline vs. week 13) |
<0.001 |
<0.001 |
0.498 |
|
|
PRTEE: Patient-rated tennis elbow evaluation; ESWT: Extracorporeal shock wave therapy; Data were expressed as mean±SD (min. – max.). Paired t-test was used to compare two dependent variables. The One-Way ANOVA was used to compare three independent variables. |
||||
Table II: Comparison of the groups for the changes in the PRTEE scores.
|
The PRTEE scores |
Focused ESWT (n=30) |
Radial ESWT (n=29) |
Sham ESWT (n=28) |
p |
|
Pain (baseline - week 5) |
18.8±13.9 (-9 – 43) |
11.8±9.1 (-2 – 30) |
1.3±7.1 (-6 – 22) |
0.026ST,* <0.001MWU,†,§ |
|
Pain (baseline - week 13) |
17.8±13.1 (-9 – 43) |
11.7±10.5 (-3 – 34) |
1.0±6.5 (-12 – 19) |
0.084OWA,* <0.001OWA,†,§ |
|
Function (baseline - week 5) |
17.9±12.5 (-10.0 – 44.5) |
11.2±9.5 (-3.5 – 32.5) |
1.8±7.9 (-13 – 27) |
0.025ST,* <0.001MWU,†,§ |
|
Function (baseline - week 13) |
16.9±11.6 (-7.5 – 37) |
10.7±10.1 (-13.0 – 33) |
0.5±6.8 (-10.5 – 21) |
0.032ST,* <0.001MWU,†,§ |
|
Total (baseline - week 5) |
36.7±25.9 (-19 – 87.5) |
23.0±17.2 (-2 – 57.5) |
3.1±13.8 (-14 – 49) |
0.021ST,* <0.001MWU,†,§ |
|
Total (baseline - week 13) |
34.7±24.3 (-16.5 – 75) |
22.4±18.5 (-5 – 58) |
1.5±11.6 (-20.5 – 40) |
0.044OWA,* <0.001OWA,†,§ |
|
ST: The Student t-test; MWU: The Mann-Whitney U test; OWA: The One-Way ANOVA with the Bonferroni test; *: Focused vs. Radial; †: Focused vs. Sham; §: Radial vs. Sham; PRTEE: Patient-Rated Tennis Elbow Evaluation; ESWT: Extracorporeal shock wave therapy; Data were expressed as mean±SD (min. – max.). |
||||
RESULTS
Figure 2 is a flow diagram demonstrating the distribution of patients between the groups. Due to the insufficient effect of the applied treatments and using other treatment options separate from those in the study, five drop-outs occurred in the groups. In addition to the drop-outs, five patients were removed from analyses due to a lack of follow-up (Figure 2). Thus, data from 87 patients were included in the statistical analyses (30, 29, and 28 from the treatment groups, respectively).
The focused, radial, and sham groups were similar for age (49.3±14.0, 44.2±13.3, and 46.0±16.9 years; p=0.408), gender [female: 16 (53.3%), 15 (51.7%), 15 (53.6%), male:14 (46.7%), 14 (48.3%), and 13 (46.4%), respectively; p=0.988)], body mass index (kg/m2: 26.3±2.7, 25.9±3.3, 26.2±2.1; p=0.912), and occupational features [house wife: 13(43.3%), 11(37.9%), 11(39.9%), employed: 12(40%), 14(48.3%), 11(39.9%), unemployed: 5(16.7%), 4(13.8%), 6(21.4%), respectively; p=0.918)]. Also, the three groups were comparable regarding baseline PRTEE scores for pain, function, and total points (Table I).
Compared with baseline (week 0), all PRTEE scores (pain, function, and total) were remarkably decreased in focused and radial ESWT groups at weeks 5 and 13 (p <0.001). However, the scores obtained from the follow-up examinations were similar to the baseline in the sham ESWT group (p >0.05, Table I).
Both focused and radial ESWT groups were seen as remarkably better than the sham ESWT group in all PRTEE scores (pain, function, and total) (p <0.001), for the change from first admission to interval examination times (weeks 5 and 13, Table II).
The focused ESWT was seen as better than the radial ESWT based on the change in the PRTEE pain scores from baseline to weeks 5 (18.8±13.9 vs. 11.8±9.1; p=0.026) and 13 (17.8±13.1 vs. 11.7±10.5; p=0.084) (Table II). Importantly, focused ESWT was found to be significantly more effective than radial ESWT in the PRTEE function scores for the changes from baseline to weeks 5 (17.9±12.5 vs. 11.2±9.5; p=0.025) and 13 (16.9±11.6 vs. 10.7±10.1; p=0.032) (Table II). Focused ESWT was superior to radial ESWT for the change of PRTEE total scores from baseline to weeks 5 (36.7±25.9 vs. 23.0±17.2; p=0.021) and 13 (34.7±24.3 vs. 22.4±18.5; p=0.044, Table II).
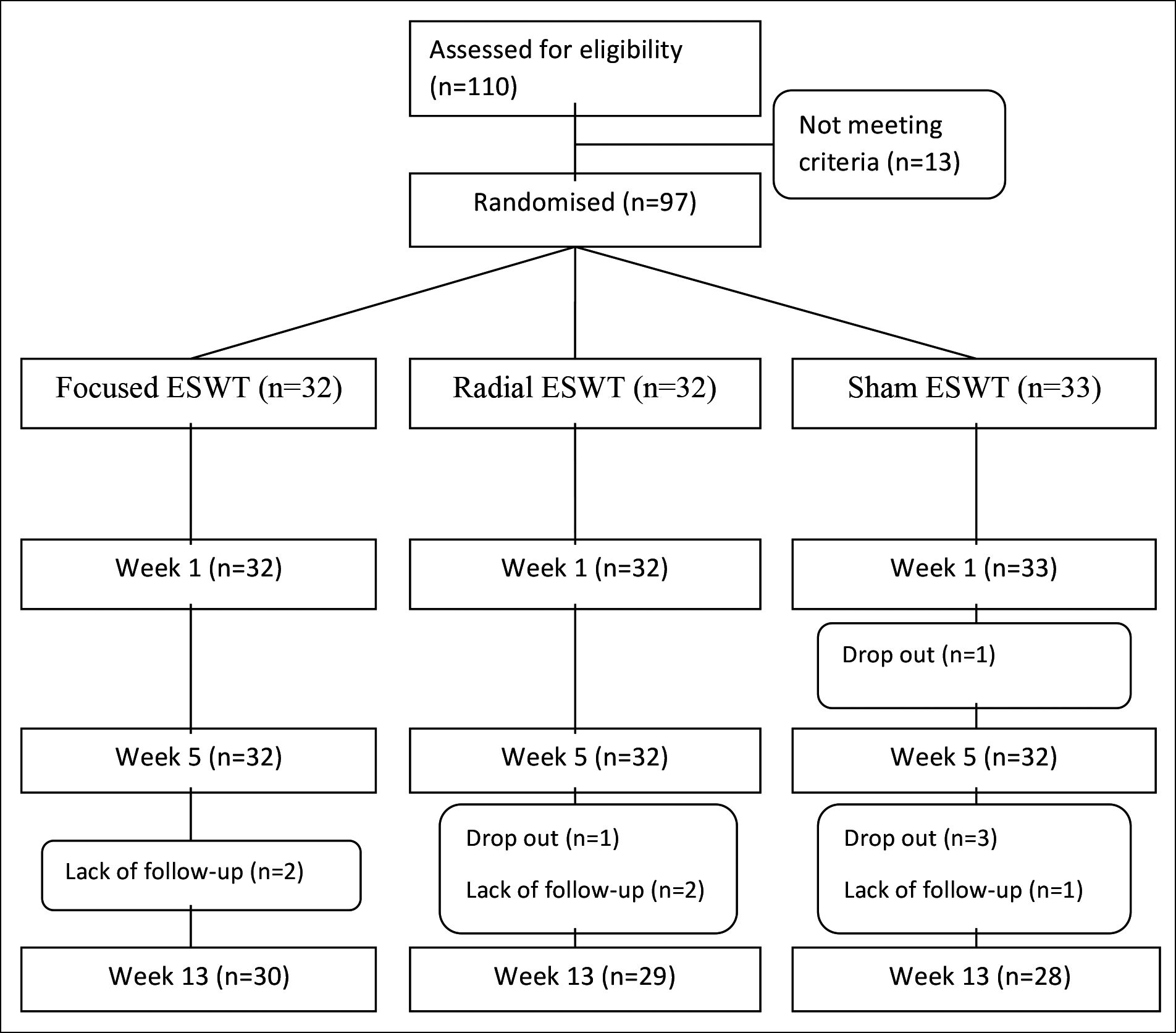 Figure 2: Flow diagram of study participants.
Figure 2: Flow diagram of study participants.
DISCUSSION
In this prospective, assessor-blind, sham-controlled, randomised trial, the authors conducted the study to see the clinical effects of focused and radial ESWT applications on lateral epicondylitis. The authors found that both focused ESWT and radial ESWT improved pain and functional status. Additionally, the degree and continuity of these effects (change from the start of therapy to the subsequent examinations) demonstrated that the focused ESWT was significantly more effective than the radial ESWT.
To obtain optimal outcomes, the authors need to compare treatment options. Therefore, examining and providing the comparative effectivity of radial and focused ESWT in cases with lateral epicondylitis was crucial. Although ESWT is usually used as a supplement to exercise programs or recommended when other conservative treatments fail,5 more studies are required to reach the ideal type of ESWT in treating lateral epicondylitis. Therefore, the present findings will have a critical significance when choosing the kind of ESWT in the clinical practice.
Reports and reviews investigating the efficacy of ESWT in managing the lateral epicondylitis have shown conflicting findings.4,9,10 In the present study, the authors’ found that focused and radial waves are useful options in the lateral epicondylitis. Considering the degenerative and inflammatory processes of lateral epicondylitis,1 the efficiency of ESWT on the lateral epicondylitis can be due to its different actions, resulting in functional improvements and relieving of pain. These functions may include restriction of pain receptors,15 activation of anti-inflammatory cytokines,16 suppression of pro-inflammatory cytokines,17 activation of neovascularization,18 stimulation of cellular proliferation,19 and increased damaged tissue renewal.20 It may be said that due to the multiple functions mentioned, ESWT may have a long-lasting effect on lateral epicondylitis.
According to the comparative results, the focused ESWT was more efficient than the radial ESWT in all scores of PRTEE (pain, function, and total) when evaluating the change from baseline to follow-up periods. Although it was not statistically significant, the change of pain score from baseline to week 13 in the focused group was more favourable than that in the radial group. As a result, the present study demonstrated that the clinical efficacy of focused ESWT is superior to the radial ESWT. Although their mechanisms of action are not fully known, the superior effect of focused wave over radial wave in the lateral epicondylitis may be related to differences in their penetration depth and working principle. Because the energy flux density (acoustic pressure) reaches the maximum level at the tip of the applicator with the radial ESWT, while it is highest at the targeted deep tissue with focused ESWT.7,8 A deeper and more focused acoustic pressure in the painful epicondyle area might be provided more effective treatment in focused ESWT compared to in radial ESWT.
Contrary to the present findings showing that the focused type is more effective, a systematic review has concluded that the radial type is related to better results in the chronic (>six months) lateral epicondylitis.11 The presently studied patients, on the other hand, had a new diagnosis of acute lateral epicondylitis with symptom duration of <3 months. Therefore, symptom duration may be a relevant factor in the successful performance of ESWT sub-types. On the other hand, a study has reported similar effectiveness of radial and focused ESWT in both acute and chronic lateral epicondylitis.12 Unlike this study, a piezo-electric generator was used in that study,12 while the device the authors used has an electro-pneumatic system. Thus, the type of shock wave generator might be another relevant factor in the success of ESWT applications.
On the other hand, this study's possible limitations should be considered. For instance, the authors did not use an advanced radiologic tool for diagnosing the lateral epicondylitis because the medical assessment and physical examination mainly diagnose it.2 The authors chose an assessor-blind sham-controlled trial; however, this study has a limitation with the operator-informed outcome measures. As another limitation, a subgroup analysis based on more detailed grouping according to weekly symptom duration has not been made in this study. Also, the cost/benefit of the ESWT compared to other non-invasive methods of treating the lateral epicondylitis should be considered.21
CONCLUSION
Focused and radial ESWT are effective for pain relief and functional improvement in lateral epicondylitis. In addition, the focused ESWT is superior to the radial ESWT for the degree and continuity of its effectiveness. Thus, the focused ESWT should be preferred to the radial ESWT in the lateral epicondylitis management.
ETHICAL APPROVAL:
The study protocol was approved by the local ethics committee (Decision No.16; Date: August 06, 2019).
PATIENTS’ CONSENT:
Informed consent were obtained from all the participants.
COMPETING INTEREST:
The authors declared no competing interests.
AUTHORS’ CONTRIBUTION:
SK, VS, SO, CA, VD: Conceived and designed the study.
VS: Conducted the acquisition of the data.
VD: Analysed the data and provided statistical expertise.
SK, VS, SO, CA: Interpreted the data.
SK, VD: Drafted the manuscript.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Sayampanathan AA, Basha M, Mitra AK. Risk factors of lateral epicondylitis: A meta-analysis. Surgeon 2020; 18(2):122-8. doi: 10.1016/j.surge.2019.08.003.
- Speers CJ, Bhogal GS, Collins R. Lateral elbow tendinosis: A review of diagnosis and management in general practice. Br J Gen Pract 2018; 68(676):548-9. doi: 10.3399/bjgp18X6 99725.
- Ma KL, Wang HQ. Management of lateral epicondylitis: A narrative literature review. Pain Res Manag 2020; 2020: 6965381. doi: 10.1155/2020/6965381.
- Yao G, Chen J, Duan Y, Chen X. Efficacy of extracorporeal shock wave therapy for lateral epicondylitis: A systematic review and meta-analysis. Biomed Res Int 2020: 2064781. doi: 10.1155/2020/2064781.
- Stasinopoulos D. Can extracorporeal shock-wave therapy be used for the management of lateral elbow tendinopathy? World J Methodol 2018; 8(3):37-9. doi: 10.5662/wjm.v8. i3.37.
- Stasinopoulos D. Issues related to the effectiveness of extracorporeal shock wave therapy for the management of lateral elbow tendinopathy. J Clin Med 2022; 11(18):5413. doi: 10.3390/jcm11185413.
- Crupnik J, Silveti S, Wajnstein N, Rolon A, Vollhardt A, Stiller P, et al. Is radial extracorporeal shock wave therapy combined with a specific rehabilitation program (rESWT + RP) more effective than sham-rESWT + RP for acute hamstring muscle complex injury type 3b in athletes? Study protocol for a prospective, randomised, double-blind, sham-controlled single centre trial. J Orthop Surg Res 2019; 14(1):234. doi: 10.1186/s13018-019-1283-x.
- Kiessling MC, Milz S, Frank HG, Korbel R, Schmitz C. Radial extracorporeal shock wave treatment harms developing chicken embryos. Sci Rep 2015; 5:8281. doi: 10.1038/srep08281.
- Zheng C, Zeng D, Chen J, Liu S, Li J, Ruan Z, et al. Effectiveness of extracorporeal shock wave therapy in patients with tennis elbow: A meta-analysis of randomised controlled trials. Medicine (Baltimore) 2020; 99(30):e21189. doi: 10. 1097/MD.0000000000021189.
- Karanasios S, Tsamasiotis GK, Michopoulos K, Sakellari V, Gioftsos G. Clinical effectiveness of shockwave therapy in lateral elbow tendinopathy: Systematic review and meta-analysis. Clin Rehabil 2021; 35(10):1383-98. doi: 10.1177/ 02692155211006860.
- Yoon SY, Kim YW, Shin IS, Moon HI, Lee SC. Does the type of extracorporeal shock therapy ınfluence treatment effectiveness in lateral epicondylitis? A systematic review and meta-analysis. Clin Orthop Relat Res 2020; 478(10):2324-39. doi: 10.1097/CORR.0000000000001246.
- Stania M, Król B, Franek A, Błaszczak E, Dolibog P, Polak A, et al. A comparative study of the efficacy of radial and focused shock wave therapy for tennis elbow depending on symptom duration. Arch Med Sci 2020; 17(6):1686-95. doi: 10.5114/aoms.2019.81361.
- Altan L, Ercan I, Konur S. Reliability and validity of Turkish version of the patient rated tennis elbow evaluation. Rheumatol Int 2010; 3(8):1049-54. doi: 10.1007/s00296-009- 1101-6.
- Faul F, Erdfelder E. “GPOWER: A priori, post-hoc, and compromise power analyses for MS-DOS [Computer program]”. 2004. Bonn, FRG: Bonn University, Department of Psychology.
- Maier M, Averbeck B, Milz S, Refior HJ, Schmitz C. Substance P and prostaglandin E2 release after shock wave application to the rabbit femur. Clin Orthop Relat Res 2003; 406: 237-45. doi: 10.1097/01.blo.0000030173.56585.8f.
- Iannone F, Moretti B, Notarnicola A, Moretti L, Patella S, Patella V, et al. Extracorporeal shock waves increase interleukin-10 expression by human osteoarthritic and healthy osteoblasts in vitro. Clin Exp Rheumatol 2009; 27(5):794-9.
- Moretti B, Iannone F, Notarnicola A, Lapadula G, Moretti L, Patella V, et al. Extracorporeal shock waves down-regulate the expression of interleukin-10 and tumor necrosis factor-alpha in osteoarthritic chondrocytes. BMC Musculoskelet Disord 2008; 9:16. doi: 10.1186/1471-2474-9-16.
- Ma HZ, Zeng BF, Li XL. Upregulation of VEGF in subchondral bone of necrotic femoral heads in rabbits with use of extracorporeal shock waves. Calcif Tissue Int 2007; 81(2): 124-31. doi: 10.1007/s00223-007-9046-9.
- Bosch G, de Mos M, van Binsbergen R, van Schie HT, van de Lest CH, van Weeren PR. The effect of focused extracorporeal shock wave therapy on collagen matrix and gene expression in normal tendons and ligaments. Equine Vet J 2009; 41(4):335-41. doi: 10.2746/042516409x370766.
- Zissler A, Steinbacher P, Zimmermann R, Pittner S, Stoiber W, Bathke AC, et al. Extracorporeal shock wave therapy accelerates regeneration after acute skeletal muscle ınjury. Am J Sports Med 2017; 45(3):676-84. doi: 10.1177/03635 46516668622.
- Guler T, Yildirim P. Comparison of the efficacy of kinesiotaping and extracorporeal shock wave therapy in patients with newly diagnosed lateral epicondylitis: A prospective randomised trial. Niger J Clin Pract 2020; 23(5):704-10. doi: 10.4103/njcp.njcp_45_19.