Clinical Efficacy of Single Vidian Neurectomy in Chronic Rhinosinusitis with Nasal Polyps and Allergic Rhinitis
By Hedi Zhuo, Yanjie Wang, Xueping Qi, Jinmei Xue, Yunfang An, Changqing ZhaoAffiliations
doi: 10.29271/jcpsp.2022.05.618ABSTRACT
Objective: To investigate the clinical efficacy of single Vidian neurectomy (sVN) in the treatment of chronic rhinosinusitis with nasal polyps and allergic rhinitis (CRSwNP &AR).
Study Design: Descriptive study.
Place and Duration of Study: Otolaryngology-Head &Neck Surgery, Shanxi Medical University Second Affiliated Hospital, Taiyuan, China, February 2016 to February 2019.
Methodology: Patients meeting the diagnostic criteria for AR and CRSwNP confirmed after assessment by an ENT physician; moderately severe and persistent AR, aged ≥18 years to ≤70 years; and testing positive for sIgE and were regularly treated with medications for three months or more before surgery with unsatisfactory symptom control. Exclusion criteria were patients with acute exacerbations of sinusitis or fungal sinusitis combined with nasal polyps, intolerant to aspirin, acute infection or sinus tumours; contraindications to general anaesthetic surgery or oral corticosteroids; and those who have received allergen immunotherapy, corticosteroids and antihistamines within one year. The relevant epidemiological data were collected, including IgE level, VAS, RQLQ, and the Lund-Kennedy scores, to assess patients' clinical symptoms and quality of life before and after surgery.
Results: Fifty-five patients were followed up for two years after surgery, and statistical analysis was performed using SPSS version 25.0. It was found that VAS scores, RQLQ scores, and Lund-Kennedy scores of the patients who underwent sVN were significantly lower at six months (all p <0.01), one year (all p <0.01, and two years all p <0.01) after surgery compared with those before surgery.
Conclusion: sVN has better efficacy in patients with CRSwNP&AR, has the potential to reduce its recurrence rate, and seems to be a safe and effective treatment.
Key Words: Chronic rhinosinusitis with nasal polyps, Allergic rhinitis, Eosinophilic chronic rhinosinusitis with nasal polyps, Single Vidian neurectomy, Clinical efficacy.
INTRODUCTION
Chronic rhinosinusitis with nasal polyps (CRSwNP) is a common inflammatory disease of the upper airways in the middle and top of the nasal cavity, septal sinuses, and sieve bubbles. It can descend from the middle nasal tract to the nasal cavity and nasopharynx, causing symptoms such as nasal congestion and decreased sense of smell.1,2 The nasal mucosa of patients with allergic rhinitis (AR) is characterised by high mucus secretion and airway tissue remodelling, which are risk factors for the development of nasal polyps.3
Patients with chronic rhinosinusitis with nasal polyps and allergic rhinitis (CRSwNP&AR, hereinafter referred to as R) have more pronounced clinical symptoms and more severe disease than those with either AR alone or with CRSwNP alone.4 According to domestic and international clinical guidelines, patients with R are often treated with a combination of surgery and drugs: surgical removal of nasal polyps and control of AR symptoms with nasal and systemic glucocorticoids and antihistamines.5,6
The Vidian nerve is a mixed nerve that includes sympathetic and parasympathetic nerves, of which the parasympathetic nerve is the main one that governs most of the glandular secretion and vasoconstriction of the nasal cavity and sinuses. The clinical symptoms of upper and lower airway hyperresponsiveness, including persistent asthma, are effectively controlled after Vidian Neurectomy (VN).7 VN is based on severing the parasympathetic nerve, then the main mechanism of action lies in the involvement of the sensory nerves, the conduction and modulation of signals from the vagus nerve after central integration, and their role in the inflammation of the upper and lower airways.
Table I: The clinical variable of patients with R.
|
Clinical variable |
Group A (n=38) |
Group B (n=17) |
p-value |
||
|
Age (years) |
43.59±10.92 |
42.63±9.23 |
0.554 |
||
|
Male:Female |
18:20 (47%:52.6%) |
12:5 (70.6%:29.4%) |
0.11 |
||
|
Nasal sinusitis |
|
||||
|
Single sinuses |
3 (7.9%) |
2 (11.8%) |
0.899 |
||
|
Multiple sinuses |
28 (73.7%) |
12 (70.6%) |
|||
|
All sinuses |
7 (18.4%) |
3 (17.6%) |
|||
|
EOS count |
A1 |
A2 |
B1 |
B2 |
|
|
7.37±13.63 |
25.52±15.94 |
11.8±15.7 |
25.49±18.1 |
0.001/0.141PA/PB) |
|
|
Data conforming to normal distribution were expressed by x ± s. Independent samples t-test and Chi-square test were used for comparison between two groups. |
|||||
Table II: Comparison of rating scales for patients undergoing sVN surgery.
|
|
VAS score |
Lund-Kennedy score |
RQLQ score |
|
Pre-operative |
31.68±5.94 |
7 [5.75, 8] |
54.95±17.76 |
|
6 months after surgery |
3 [0, 5] |
2[2, 3] |
12.03±6.67 |
|
1 year after surgery |
5 [2.75, 8.5] |
1[0, 2] |
15.82±8.14 |
|
2 years after surgery |
7 [4.75, 13.5) |
1[0.75, 2] |
21.03±11.50 |
|
P(preoperative- 6 months after surgery) |
<0.01 |
<0.01 |
<0.01 |
|
P(preoperative-1 year after surgery) |
<0.01 |
<0.01 |
<0.01 |
|
P(preoperative - 2 years after surgery) |
<0.01 |
0.002 |
<0.01 |
|
P(6 months after surgery - 1 year after surgery) |
<0.01 |
0.002 |
<0.01 |
|
P(1 year after surgery - 2 years after surgery) |
<0.01 |
0.953 |
<0.01 |
|
Wilcoxon signed rank-sum test and pair simples test were used to compare between different times assessment of postoperative outcome of sVN surgery |
|||
From a neuroimmune perspective, unilateral surgery can be performed with results close to those of bilateral surgery and more in line with the minimally invasive concept.
A recent study, analysing lung function in patients with R, found that VN was effective in relieving patients' nasal symptoms and improving lung function.8 This suggests the effectiveness of VN for R. As the action of the nerve is bilateral, unilateral surgery may be more beneficial for central regulation and its recovery, given the dry eye that may occur after VN surgery. Based on this conjecture, sVN has some efficacy in patients with R.
The aim of this study was to investigate the efficacy of sVN on R, with a view to providing a safe and effective surgical treatment for R.
METHODOLOGY
Fifty-five patients with R, who had attended the Second Affiliated Hospital of Shanxi Medical University from February 2016 to February 2019, were selected. The diagnostic criteria were referred to the guidelines for diagnosis and treatment of R.5,6 Preoperative nasal endoscopy, 3D CT of the sinuses and pterygoid nerve reconstruction films were performed in all patients. The patients were followed up for two years after surgery. Inclusion criteria were meeting diagnostic criteria for AR and CRSwNP confirmed after assessment by an ENT physician; moderately severe and persistent AR that had failed to respond to medication; aged between ≥18 years and ≤70 years; positive sIgE, and were regularly treated with medications for three months or more before surgery but had unsatisfactory symptom control. Exclusion criteria were patients with acute exacerbations of sinusitis or fungal sinusitis combined with nasal polyps, intolerance to aspirin, acute infection or sinus tumours; contraindications to general anaesthetic surgery or oral corticosteroids; and patients who have received allergen immunotherapy, corticosteroids and antihistamines within one year.
The 55 patients were divided into two groups. Group A was operated with combined nasal polypectomy and sVN, and group B was operated with nasal polypectomy alone. According to the pathological examination results, the patients in groups A and B were divided into groups A1, A2 and B1, B2. Group A1 represents patients with non-eosinophilic chronic rhinosinusitis with nasal polyps and AR (Non- ECRSwNP &AR, hereinafter referred to as RⅠ), who had undergone sVN surgery; Group A2 represents patients with eosinophilic chronic rhinosinusitis with nasal polyps (ECRSwNP & AR, hereinafter referred to as RⅡ), who had undergone sVN surgery; Group B1 represents patients with RⅠ who did not undergo sVN surgery, and Group B2 represents patients with RⅡ,who did not undergo sVN surgery.
Pathological sections of nasal polyps and EOS counts were taken as the average of five random high magnification views. The counts were repeated twice and averaged. Based on EOS counts greater than 55 per visual field, groups A and B were divided into A1 and A2 and B1 and B2, as shown in Figure 1.
Table III: Comparison of postoperative outcomes in patients with RⅠ.
|
n |
VAS score |
Lund-Kennedy rating |
RQLQ score |
||||||||||
|
Pre-operative |
6 months after surgery |
1 year after surgery |
2 years after surgery |
Pre-operative |
6 months after surgery |
1 year after surgery |
2 years after surgery |
Pre-operative |
6 months after surgery |
1 year after surgery |
2 years after surgery |
||
|
A1 |
14 |
30 [26.5,33.25] |
4 [0,5.25] |
5.5 [4,10.25] |
7 [4.75,16] |
7 [5,8] |
2 [0.75,2] |
2 [0.75,2] |
1 [0,2] |
66 [48,73.5] |
11.5 [9.75,16.75] |
19 [11,24.25] |
23.5 [13.25,29.75] |
|
B1 |
6 |
37 [26.25,41.25] |
1.5 [0,6.75] |
3.5 [0,9.5] |
4.5 [1.5,16.25] |
7 [6,7.75] |
2 [2,3.5] |
3 [2,3.25] |
2 [1,2.5] |
34 [42,73.25] |
11 [0,23.5] |
11 [3.75,26.75] |
13.5 [7.5,34.75] |
|
Z |
|
1.322 |
-0.594 |
-1.163 |
-1.033 |
0.551 |
2.007 |
2.319 |
1.708 |
-1.485 |
-0.207 |
-0.827 |
-0.826 |
|
P |
|
0.207 >0.05 |
0.602 >0.05 |
0.274 >0.05 |
0.312 >0.05 |
0.602 >0.05 |
0.076 >0.05 |
0.026 <0.05 |
0.109 >0.05 |
0.153 >0.05 |
0.841 >0.05 |
0.441 >0.05 |
0.444 >0.05 |
|
Mann-Whitney U-test was used to compare different groups; Comparison of postoperative outcomes for patients with RⅠ |
|||||||||||||
Table IV: Comparison of postoperative outcomes in patients with RⅡ.
|
n |
VAS score |
Lund-Kennedy score |
RQLQ score |
|||||||||
|
Pre-operative |
6 months after surgery |
1 year after surgery |
2 years after surgery |
Pre-operative |
6 months after surgery |
1 year after surgery |
2 years after surgery |
Pre-operative |
6 months after surgery |
1 year after surgery |
2 years after surgery |
|
|
24 |
34.5[28.25,36] |
3[0,5] |
5[2,8] |
7.5[4.25,12.75] |
7[6,8] |
2[2,3] |
1[0,2] |
1.5[1,2] |
49[37,58.5] |
11.5[8,15] |
16.5[9.25,21] |
15[19,31] |
|
11 |
32[22,39] |
0[0,4] |
0[0,5] |
2[0,7] |
7[5,7] |
4[2,5] |
3[2,3] |
3[2,3] |
42[32,57] |
8[0,10] |
8[0,14] |
10[0,13] |
|
|
-0.410 |
-1.446 |
-2.033 |
-2.256 |
-0.986 |
2.426 |
3.224 |
3.494 |
-0.658 |
-2.361 |
-2.407 |
-2.553 |
|
|
0.687 >0.05 |
0.174 >0.05 |
0.043 <0.05 |
0.025 <0.05 |
0.352 >0.05 |
0.018 <0.05 |
0.001 <0.05 |
<0.001 <0.05 |
0.517 >0.05 |
0.018 <0.05 |
0.015 <0.05 |
0.009 <0.05 |
|
Mann-Whitney U-test was used to compare different groups; Comparison of postoperative outcomes for patients with RⅡ. |
||||||||||||
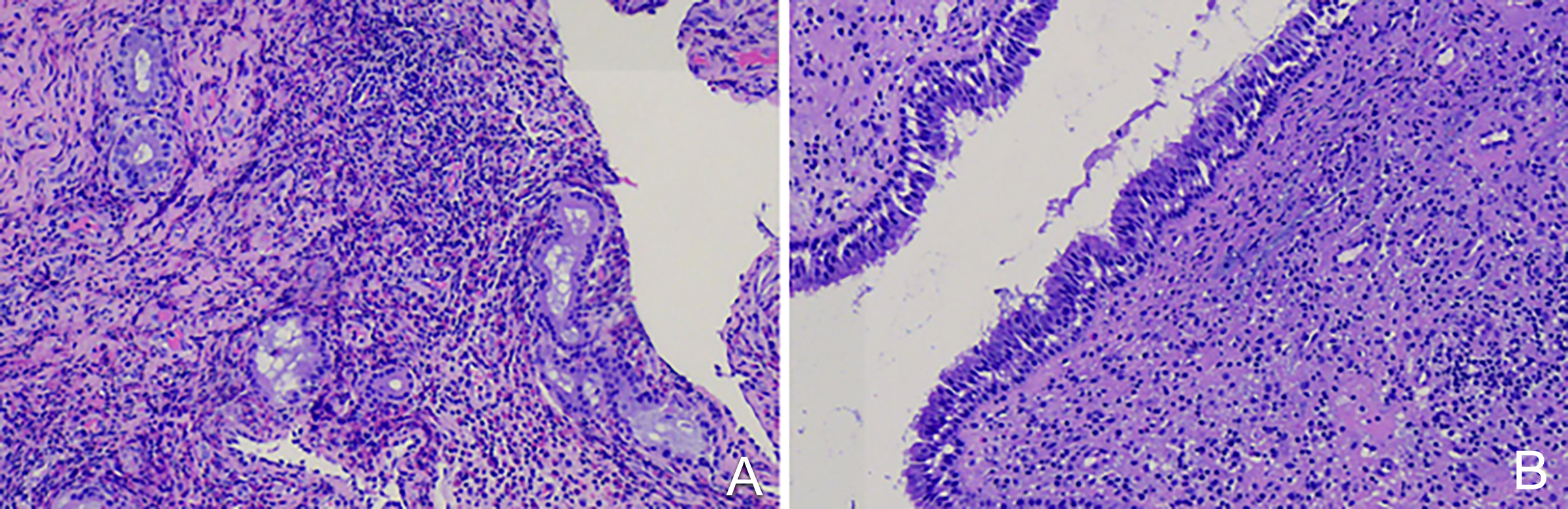
Figure 1: Illustration of histopathological findings of postoperative nasa l polyps.1A: ECRSwNP; 1B: Non-ECRSwNP.
The same operator performed all procedures under tracheal intubation with intravenous anaesthesia. The CT films were read preoperatively, the anatomical typing of the pterygoid nerve was used as a basis, the location of the nasal polyp and the need to open the sinuses were used as a reference, and the side was carefully selected.9-11
Patients are followed up two years after surgery, using outpatient follow-up and telephone follow-up as follows: collection of scores at six months, one year and two years after surgery. Visual scale score (VAS) was used to the participants, were graded on the severity of their nasal symptoms. The Lund-Kennedy score was used for the assessment of objective nasal symptoms. Rhinoconjunctivitis quality of life questionnaire (RQLQ) assessed the quality of life of the participants.
All assays were independently performed thrice. IBM SPSS software version 25.0 (IBM; USA) was used for statistical analyses. Quantitative data were first tested for normality test, using Shapiro-Wilk test. Data that did not obey normal distribution were described, using the median (P25, P75).
Mann-Whitney U-test was used to compare different groups, and Wilcoxon signed rank-sum test was used to compare between other times, and p <0.05 was statistically significant. Categorical variables were expressed as counts and percentages.
RESULTS
The clinical and pathological data of patients with R are described in Table I. This Table mainly compares the general data between the two groups, whose sinus (p = 0.899) and EOS counts (p = 0.001/0.141) were compared with a view to their having no effect on the surgical approach.
The results in Table II, compared with the preoperative period, the VAS scores were significantly lower at six months (p <0.01), one year (p <0.01), and two years (p <0.01) postoperatively compared with the preoperative period. The Lund-Kennedy score was statistically significantly lower at six months (p <0.01), 1 year (p <0.01) and two years (p <0.01) postoperatively compared to pre-operatively, no significant change two years after surgery compared to one year after surgery (p = 0.953). The RQLQ scores were statistically significantly lower at six months (p <0.01), one year (p <0.01) and two years (p <0.01) postoperatively compared to preoperatively.
As seen by comparing patients in groups A1 and B1, no significant differences were seen in preoperative VAS scores and RQLQ scores, no significant differences were seen in postoperative VAS scores and RQLQ scores at six months (p = 0.602 and 0.841, respectively), one year (p=0.274 and p=0.441 respectively) and two years (p = 0.312 and p=0.444, respectively) after surgery, the Lund-Kennedy scores in group A1 were significantly lower at one year postoperatively compared to group B1 (p = 0.026), the rest having no difference. It shows that there is no significant difference in efficacy between the two surgical approaches for patients in groups A1 and B1 (Table III).
For patients with RⅡ, the VAS scores were significantly lower in the A2 group 1 year (p = 0.043) and two years (p = 0.025) after surgery compared to the B2 group. The RQLQ scores and Lund-Kennedy scores were significantly lower in the A2 group at six months (p = 0.018 and = 0.018), one year (p = 0.015 and = 0.001, respectively) and two years (p = 0.009 and <0.001, respectively) after surgery compared to the B2 group. This result indicates the efficacy of sVN in RⅡcompared to nasal polypectomy alone (Table IV).
DISCUSSION
In patients with CRSwNP, the underlying allergic factors of Th2 inflammatory response increased EOS, and elevated IgE can further exacerbate nasal polyp symptoms. Mechanistically, allergic inflammation in the nasal cavity alters the integrity of the nasal mucosa, impairs nasal cilia function, and leads to worsening nasal polyp symptoms, so the two are interrelated and dependent.12,13 Lou et al. proposed a staging of nasal polyps based on the cytological level by analysing the infiltration of inflammatory cells in nasal polyps in patients with CRSwNP, where the recurrence rate at 3 years after surgery in patients with ECRSwNP was close to 100%.14,15 At present, patients with ECRSwNP are mainly treated with surgery and medication in order to achieve long-term results, but the lesions cannot be eradicated and the treatment of recurrent polyps after surgery remains a clinical problem.
It was found that sVN combined with nasal polypectomy was effective in patients with R, and the patient’s clinical symptoms were significantly reduced after surgery. In patients with RⅠ, no significant differences were seen in the efficacy of the two procedures; whereas, in patients with RⅡ, there were significant differences in VAS scores, Lund-Kennedy scores, and RQLQ scores at six months, one year, and two years postoperatively in patients undergoing sVN compared with those undergoing nasal polypectomy alone, indicating that sVN was more effective than simple of nasal polypectomy were more effective in improving patients' postoperative symptoms. With regard to postoperative complications, most patients have postoperative complications that resolve on their own.
Based on the study of the neuroimmune mechanism of AR, the team proposed the idea of ‘unilateral surgery, a bilateral benefit. The subject group examined the impact of sVN on patients with AR.
It is suggested that sVN has some effect on the treatment of AR.11 It was also found that some patients with R had better postoperative recovery after sVN than those who underwent nasal polypectomy alone, and the possibility of a lower recurrence rate existed. Conventional functional nasal endoscopic surgery is effective in patients with CRSwNP. Still, about 50% of patients may recur after surgery, while the recurrence rate is higher in patients with ECRSwNP.16 In conjunction with the results of this study, it was found that sVN can provide a degree of symptom control; and reduce the likelihood of postoperative recurrence in patients with RⅡ, who have a high rate of postoperative recurrence, compared to conventional functional nasal endoscopy.
This study suggests that sVN combined with nasal polypectomy is effective in patients with R, which may be related to the neuroimmune mechanism present in patients with R. The previous study found that sVN can block the release of neuropeptides and thus reduce the nasal hyperresponsiveness caused by allergic factors in patients because the parasympathetic nerves in the pterygoductal nerve innervate most of the glandular secretion and vasoconstriction of the nasal cavity and sinuses. The neuromodulation of the upper respiratory tract is maintained by the sympathetic and parasympathetic nervous systems, which innervate and interact in the nasal mucosa. The study found that three neuropeptides released from the NANC nerve in the nasal mucosa, namely substance P, CGRP and VIP, were involved in the formation and growth of nasal polyps.17 These findings suggest that neuroimmune mechanisms play an important role in the pathogenesis of R, which in turn suggests that sVN is effective not only in patients with AR, but also in patients with CRSwNP. sVN reduces edema in the lamina propria of the nasal mucosa epithelium, while reducing mast cell degranulation and thus significantly reducing the release of inflammatory mediators.18 This nerve block may cut off the pathway by which EOS-generated mediators activate sensory nerves and thus alter the mechanical response of the airway. This partly explains the results of this study suggesting the efficacy of sVN in patients with RⅡ who had a high recurrence rate.
The limitations of this study are the 2-year follow-up period and the fact that no intra-group comparisons were made, and the long-term efficacy needs to be further investigated;in the future, further long-term follow-up will be carried out on these patients, with more comprehensive records of objective data on nasal symptoms and medication use and nasal resistance before and after surgery, to investigate more fully and effectively the treatment of patients with R.
When long-term pharmacological treatment does not control well, the symptoms of patients with R, in addition to simple nasal polypectomy, sVN can be taken at the same time, which does not have the potential to reduce the postoperative recurrence of nasal polyps and has some therapeutic effect on patients with RⅡ who have a high postoperative recurrence rate.
CONCLUSION
sVN has a certain alleviating effect on the symptoms of R patients, and has a certain controlling effect on the postoperative recurrence of R after combined nasal polypectomy, which is likely to be a preferred treatment for R in the future.
ETHICAL APPROVAL:
Ethical approval of this study was obtained from the Ethics Committee of Shanxi Medical University Second Affiliated Hospital prior to initiation of the research work.
COMPETING INTEREST:
The authors declared no conflict of interest.
FUNDING:
This project was funded by the National Natural Science Foundation of China (No: 81870707, 81970865, 82171119, 82171120).
AUTHORS’ CONTRIBUTION:
HZ, CZ: Performed to design this research.
YW, XQ: Analysed the data and worked on pictures, and forms.
JX, YA: Revised the manuscript.
CZ: Oversaw the research, monitored the data collection, and revised the draft manuscript.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Ranford D, Hopkins C. Safety review of current systemic treatments for severe chronic rhinosinusitis with nasal polyps and future directions. Expert Opin Drug Saf 2021; 20(10):1177-89. doi: 10.1080/14740338.2021.1926981.
- Teranishi Y, Jin D, Takano S, Sunami K, Takai S. Decrease in number of mast cells in resected nasal polyps as an indicator for postoperative recurrence of chronic rhinosinusitis. Immun Inflamm Dis 2019; 7(3):191-200. doi: 10.1002/iid3. 261.
- Wang W, Gao Y, Zhu Z, Zha Y, Wang X, Qi F, et al. Changes in the clinical and histological characteristics of Chinese chronic rhinosinusitis with nasal polyps over 11 years. Int Forum Allergy Rhinol 2019; 9(2):149-57. doi: 10.1002/ alr.22234.
- Samitas K, Carter A, Kariyawasam HH, Xanthou G. Upper and lower airway remodelling mechanisms in asthma, allergic rhinitis and chronic rhinosinusitis: The one airway concept revisited. Allergy 2018; 73(5):993-1002. doi: 10. 1111/all.13373.
- Subspecialty group of rhinology, Editorial board of chinese journal of otorhinolaryngology head and neck surgery; Subspecialty group of rhinology, society of otorhinolaryngology head and neck surgery, chinese medical association. [Chinese guidelines for diagnosis and treatment of allergic rhinitis]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2016; 51(1):6-24.
- Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S, et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinol 2020; 58 (Suppl S29): 1-464. doi: 10.4193/Rhin20.600.
- Ai J, Xie Z, Qing X, Li W, Liu H, Wang T, et al. Clinical effect of endoscopic vidian neurectomy on bronchial asthma outcomes in patients with coexisting refractory allergic rhinitis and asthma. Am J Rhinol Allergy 2018; 32(3): 139-46. doi: 10.1177/1945892418764964.
- Maimaitiaili G, Kahaer K, Tang L, Zhang J. The effect of vidian neurectomy on pulmonary function in patients with allergic rhinitis and chronic rhinosinusitis with nasal polyps. Am J Med Sci 2020; 360(2):137-45. doi: 10.1016/j.amjms. 2020.04.024.
- Zhao CQ, Zhang YT, He M. Effects of vidian neurectomy on allergic rhinitis. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2017; 52(7):484-90. doi: 10.3760/cma.j.issn.1673- 0860.2017.07.002.
- Ji YJ, An YF, Xue JM, Li QF, Suo LM, Zhang YT, et al. A preliminary study of a modified transnasal endoscopic three step vidian neurectomy. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2018; 32(20):1542-5. doi: 10.13201/j. issn.1001- 1781.2018.20.003.
- Ji YJ, An YF, Xue JM, Li QF, Hou R, Zhang YT, et al. Analysis of clinical effect of unilateral vidian neurectomy following endoscopic trans-sphenoethmoidal recess approach for allergic rhinitis treatment. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2018; 32(19):1455-8. doi: 10.13201/j.issn. 1001- 1781.2018.19.003.
- Halderman AA, Tully LJ. The role of allergy in chronic rhinosinusitis. Otolaryngol Clin North Am 2017; 50(6):1077-90. doi: 10.1016/j.otc.2017.08.003.
- Shen KC, Lin YT, Lin CF, Chang CH, Yeh TH. Allergy accelerates the disease progression of chronic rhinosinusitis. Acta Otolaryngol 2019; 139(1):75-9. doi: 10.1080/00016489. 2018.1552368.
- Lou H, Meng Y, Piao Y, Zhang N, Bachert C, Wang C et al. Cellular phenotyping of chronic rhinosinusitis with nasal polyps. Rhinology 2016; 54(2):150-9. doi: 10.1080/000 16489.2018.1552368.
- Lou H, Meng Y, Piao Y, Wang C, Zhang L, Bachert C. Predictive significance of tissue eosinophilia for nasal polyp recurrence in the Chinese population. Am J Rhinol Allergy 2015; 29(5):350-6. doi: 10.2500/ajra.2015.29.4231.
- Meng Y, Zhang L, Lou H, Wang C. Predictive value of computed tomography in the recurrence of chronic rhinosinusitis with nasal polyps. Int Forum Allergy Rhinol 2019; 9(11):1236-43. doi: 10.1002/alr.22355.
- Li XG, Shi GG, Wang XY. Expression and meaning of three neuropeptides in the initial stage of recurring nasal polyp. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2006; 41(4):303-4.
- Johnston LK, Hsu CL, Krier-Burris RA, Chhiba KD, Chien KB, McKenzie A, et al. IL-33 precedes il-5 in regulating eosinophil commitment and is required for eosinophil homeostasis. J Immunol 2016; 197(9):3445-53. doi: 10. 4049/jimmunol.1600611.