Carpometacarpal Joint Dislocations as a Rare Cause of Hand Pain
By Ali CelikAffiliations
doi: 10.29271/jcpsp.2022.08.S171ABSTRACT
Carpometacarpal joint dislocations represent not more than 1% of all hand injuries due to stable joint structures and high-energy trauma mechanism. Unfortunately, there are many missed cases suffering from ongoing pain and loss of function because of difficulty in diagnosis. Here we present a case of a healthy 42-year male who presented to the emergency department with hand pain after a punch injury. On physical examination, painful swelling at the dorsal side of his right hand was noted. His radiographic images showed dorsal dislocation of fourth and fifth carpometacarpal joints, and the dislocations were reduced to the anatomical position by the emergency physician without any complication. In the case of carpometacarpal joint fracture or dislocations, early diagnosis and reduction are the most critical steps to avoid severe morbidity, and it is only possible with careful evaluation of physical and radiological findings. In conclusion, as seen in our case, emergency physicians should remain vigilant in the diagnosis and treatment of rare traumatic injuries.
Key Words: Carpometacarpal joints, Dislocation, Hand injury, Pain.
INTRODUCTION
Carpometacarpal (CMC) joint dislocations account for less than 1% of all hand injuries.1 There are many late and missed cases that suffer from complications such as persistent pain, arthritis, and a decrease in grip strength. Patients usually complain of pain and swelling on the first presentation, and a careful examination with the interpretation of three-view radiographs is required as a first-line screening method. If there is a suspicion of obscure carpal bone fractures, computed tomography (CT) scans should be ordered. Non-surgical follow-up after closed reduction and splinting could be satisfactory for some patient groups that have stable joints without neurovascular complications.2 In terms of complex injuries such as dislocation combined with carpal bone fractures linked to the joint surface, surgical interventions are needed for saving patients from severe morbidity. Herein, we present a case of a healthy 42-year male who presented to the emergency department with hand pain after a punch injury. He was managed conservatively by an emergency physician without any need for surgery.
CASE REPORT
A healthy 42-year male presented to our emergency department with right-hand pain after a punch injury. His physical examination revealed a painful swelling on the dorsal side of the fourth and fifth CMC joints without any signs of neurovascular injury. The normal range of motions of his right wrist was preserved, but the pain was worsening with movements of the fourth and fifth fingers. The patient was sent to the radiology unit for plain radiographs, and they showed dorsal dislocation of the fourth and fifth CMC joints (Figure 1). The reduction of dislocations was performed by the emergency physician by applying traction to the ulnar side of the hand, and reexamination showed no instability or any sign of neurovascular injury. After a cast splinting procedure, repeat X-rays (Figure 2) and computed tomography (CT) scans (Figure 3) were obtained, and they confirmed normal joint anatomy with tiny avulsion fragment of the hamate bone. Keeping in view the post-reduction radiological images and physical examination findings, it was decided that the patient did not require additional intervention, and conservative follow-up was considered as an appropriate treatment option for him. The patient was discharged with instructions for orthopaedic surgery outpatient clinic follow-up within two days, and after weekly follow-up with plain radiographs, the patient’s hand was mobilized at the end of the fifth week. Six months later, he has gained almost the whole function and strength of his right hand.
 Figure 1: X-ray views (anteroposterior and oblique). The anteroposterior view shows overlapping of bones at two ulnar-sided carpometacarpal joints, loss of joint space, and in parallelism of joint lines. The dorsal dislocations are best visualised on oblique view.
Figure 1: X-ray views (anteroposterior and oblique). The anteroposterior view shows overlapping of bones at two ulnar-sided carpometacarpal joints, loss of joint space, and in parallelism of joint lines. The dorsal dislocations are best visualised on oblique view.
 Figure 2: After reduction and cast splinting, control anteroposterior and oblique views.
Figure 2: After reduction and cast splinting, control anteroposterior and oblique views.
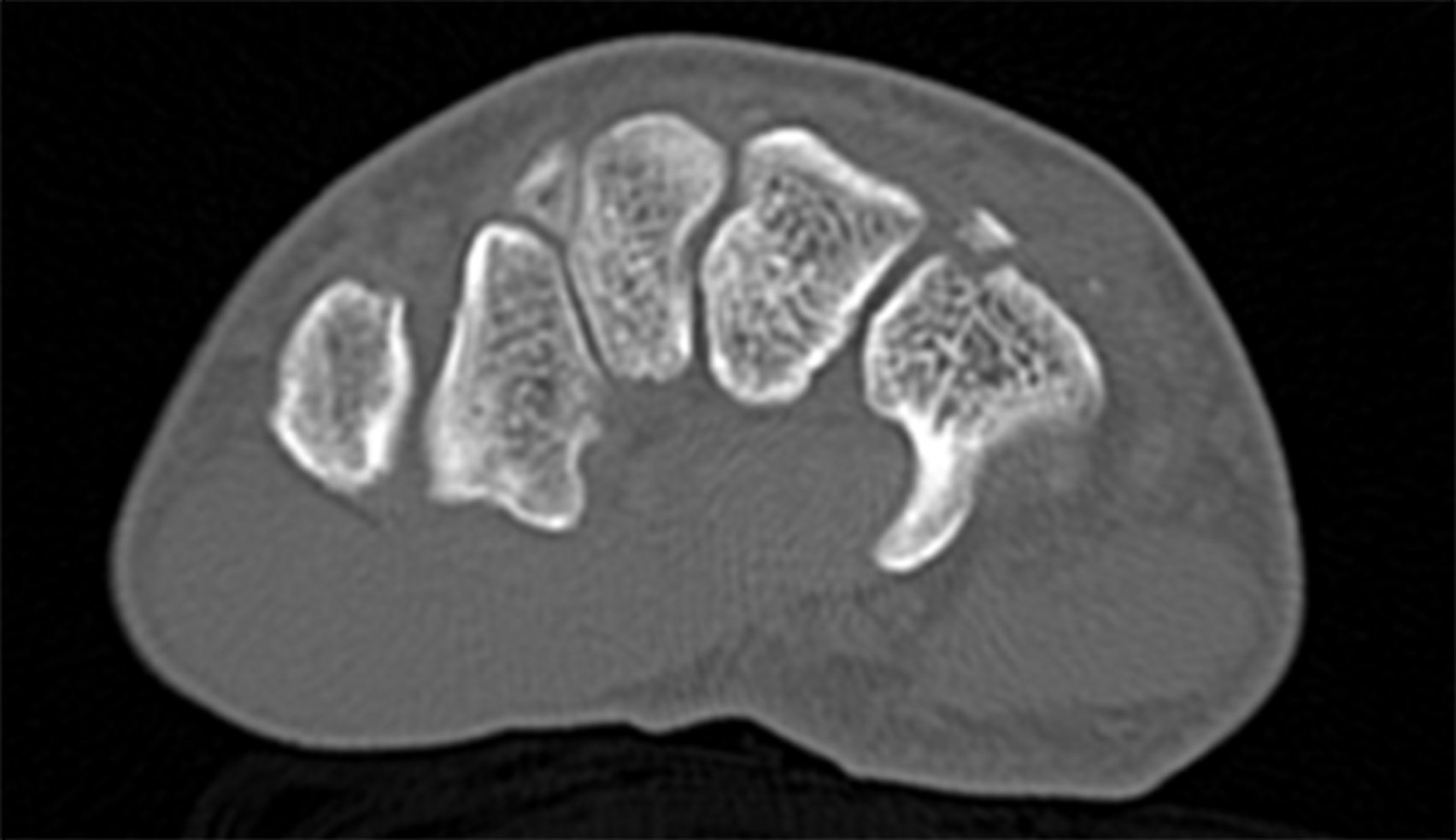 Figure 3: Computed tomography image in axial plane shows a tiny avulsion fracture of hamate bone.
Figure 3: Computed tomography image in axial plane shows a tiny avulsion fracture of hamate bone.
DISCUSSION
CMC joint dislocations are unique injuries that result in severe morbidity while they are frequently missed. They are uncommon pathologies resulting from trivial injuries such as punching. Most of the physicians will investigate fractures rather than isolated dislocations. So, it can be challenging to detect them, and sometimes these can be overlooked during the first presentation. Henderson et al. showed that more than half of the dislocations were missed in emergency departments.3 A cautious physical examination and radiography interpretation are essential steps in patients' evaluation in case of clinical suspicion. Furthermore, the examination should focus on the extent of injuries in terms of osseous and neurovascular involvements. The most common physical examination findings are tenderness, swelling, and sometimes crepitations. Firstly, three-view plain radiographs should be ordered, and lateral views are most useful for dislocations whereas oblique and anteroposterior (AP) ones can help to find out the extent of trauma such as carpal or metacarpal fractures. On the AP views, we should focus on the carpal and metacarpal bones and joint anatomy. Any overlapping of osseous structures at the joint or loss of continuity of joint lines could be important clues to dislocation and subluxation.
After the diagnosis of dislocation, the rapid reduction is crucial for normal hand functions without complication. Application of traction to ulnar-sided metacarpals is usually enough for reduction to anatomical position, but sometimes manipulations of metacarpal bases are needed. After the reduction procedure, joint stability and neurovascular status should be reexamined. Mostly ulnar, and rarely median nerve injuries, and in cases of late diagnosis, compartment and carpal tunnel syndromes could be seen as complications.1
Although there are no strict rules about permanent treatment, in case of fractures that extend to joint space, K-wire fixation or open reduction is indicated.4,5 At this point, hand and wrist CT, or magnetic resistance imaging (MRI) scans are needed for the classification of injury. A recent study regarding CT classification of CMC fracture-dislocations by Kim et al. showed that if an anatomical reduction is guaranteed in the CT scans, tiny avulsion fractures of carpal bones not linked to the intra-articular surface could be neglected and as in our case, they usually are not an indication for surgery.6 In addition to radiological findings, the timing of reduction is very crucial for successful treatment. In the study of Zhang et al., all the acute dislocations were managed conservatively without the need for open surgical interventions.7
Prompt diagnosis and early reduction are the most important steps to avoid serious morbidity in the case of CMC joint dislocations, and it would be only achievable with an accurate evaluation of physical and radiological findings. Besides, if there is a reasonable finding of complex injury, CTMRI scans should be ordered to choose the most suitable treatment approach.
PATIENT’S CONSENT:
The informed consent form had been read and signed by the patient.
COMPETING INTEREST:
The author declared no competing interest.
AUTHOR’S CONTRIBUTION:
AC: Design, literature search, discussion, and drafting.
REFERENCES
- Enajat M, de Boer L, Smit JM. A dislocation of the carpal-metacarpal joints of the index, middle and ring finger. Ame J Emerg Med 2009; 27(5):630.e1-e2. doi: 10.1016/ j.ajem.2008.08.035.
- Storken G, Bogie R, Jansen EJ. Acute ulnar carpo-metacarpal dislocations. Can it be treated conservatively? A review of four cases. Hand 2011; 6(4):420-3. doi: 10.1007/s11552-011-9347-3.
- Henderson J, Arafa M. Carpometacarpal dislocation. An easily missed diagnosis. J Bone Joint Surg Br 1987; 69(2):212-4. doi: 10.1302/0301-620X.69B2.3818751.
- Steinmetz G, Corning E, Hulse T, Fitzgerald C, Holy F, Boydstun S, et al. Carpometacarpal fracture-dislocations: A retrospective review of injury characteristics and radiographic outcomes. Hand 2021; 16(3):362-7. doi: 10.1177/1558944719852743.
- Lefere M, Dallaudière B, Omoumi P, Cyteval C, Larbi A. Rare carpometacarpal dislocations. Orthop Traumatol Surg Res 2016; 102(6):813-6. doi: 10.1016/j.otsr.2016. 04.003.
- Kim JK, Shin SJ. A novel hamatometacarpal fracture–dislocation classification system based on CT scan. Injury 2012; 43(7):1112-7. doi: 10.1016/j.injury. 2012.02.019.
- Zhang C, Wang H, Liang C, Yu W, Li Y, Shang R, et al. The effect of timing on the treatment and outcome of combined fourth and fifth carpometacarpal fracture dislocations. J Hand Surg Am 2015; 40(11):2169-75.e1. doi: 10.1016/j.jhsa.2015.07.01.