Anthropometric and Clinical Analyses of the Distal Tibia, Posterior Tibial Tendon, and Flexor Digitorum Longus Tendon on MRI
By Emre Emekli1, Ugur Toprak2Affiliations
doi: 10.29271/jcpsp.2022.09.1110ABSTRACT
Objective: To determine the gender and age differences in posterior tibial tendon (PTT), flexor digitorum longus tendon (FDLT), medial malleolar groove (MMG), and posterior, anterior, and total posterior malleolus (PMP, APM, and TPM, respectively) and evaluate the use of these parameters for posterior malleolus plating.
Study Design: Descriptive study.
Place and Duration of Study: Department of Radiology, Etimesgut Şehit Sait Ertürk State Hospital, Ankara, Turkey, from January to December 2020.
Methodology: The magnetic resonance images (MRI) of the ankle were evaluated. PTT and FDLT thickness and width, MMG depth, width, length, and groove opening angle, and APM, TPM, and PPM length were measured. Receiver operating characteristic analysis was conducted to determine whether the variables differed between gender and age.
Results: The study included 103 patients (61 women, 42 men). For gender discrimination, the sensitivity, specificity, and cut-off values were 78.6%, 72.1%, and 7.48 mm, respectively. For the PTT width: 76.2%, 77%, and 3.88 mm, respectively; for the PTT thickness: 85.7%, 86.9%, and 40.41 mm, respectively; and for the APM length, the APM, TPM, and PPM length measurements were statistically and significantly differed between the genders (p<0.001). The APM/PPM ratio was 0.47±0.057 mm in women and 0.47±0.060 mm in men, and TPM/PPM was determined as 0.55±0.604 mm and 0.56±0.657 mm. There was a statistically significant weak positive correlation among the age, MMG length, and FDLT width.
Conclusion: The groove depth and width, PTT and FDLT width and thickness, and TPM, PPM, and APM length can be used in gender prediction. The APM/PPM ratio can be calculated to determine the plating length in posterior malleolus fractures.
Key words: Medial malleolar groove, Posterior tibial tendon, Flexor digitorum longus tendon, posterior malleolus, MRI.
INTRODUCTION
There are two prominences in the distal of the tibia, called the medial malleolus (MM) and the posterior tibial protrusion [posterior malleolus (PM)]. The MM part of the tibia is longer and joins the ankle by forming a joint with the medial talus of the foot. The lateral tibial face is concave and creates a groove for the distal fibula. Immediately posterior to the MM is the medial malleolar groove (MMG), which has also been given other names, including the malleolar sulcus, posterior tibial tendon (PTT) groove, and retromalleolar groove.1 PM is an important structure to which the posterior tibiofibular ligament adheres and stabilises the ankle joint.2
The ankle fractures are very common in clinical practice, constituting approximately 3.9% of all the fractures. Approximately 7-44%,3,4 of the ankle fractures are accompanied by the PM fractures. The isolated PM fractures are rarer, observed in 0.5-1% of all the fracture cases.5,6 The plating of PM is a common procedure mainly used in fixing or supporting the PM fractures.7 The studies have shown that plating has better clinical results compared to screw fixation.8,9 PM plating shows better biomechanical strength and achieves better anatomic reduction compared to the anteroposterior screw fixation.10,11 However, understanding of PM anatomy is important in choosing the appropriate plate fixation method.
PTT subluxation and dislocation, secondary to the high energy traumas or the anatomical structure of MMG, have been previously reported. In such patients, diagnosis may be delayed, and the tendon can move anteriorly and medially over MM.1,12,13 Cases presenting with dislocation due to the presence of bilateral convex MG have also been previously described.14 MMG deepening is a surgical procedure recommended in the literature, although there is no complete consensus on its use in PTT dislocation.15 In daily magnetic resonance imaging (MRI) experience, PTT and the flexor digitorum longus tendon (FDLT) are generally oval in shape and extend into the groove. In addition, the MMG depth and length differ among the individuals.
The aim of this study was to investigate the width and thickness of PTT and FDLT; the depth, width and length of MMG; and the groove angle and the length of PM at the different levels in order to determine the difference in age and gender in patients without any joint or tibial anomalies for planning fracture plating.
METHODOLOGY
Ethical approval was waived by the local Ethics Committee of Yildirim Beyazit University Yenimahalle Education and Research Hospital (date: 26 May 2021, approval No. 2021-07-01) in view of the retrospective nature of the study and all the procedures performed being the part of routine patient care. MRI images were retrospectively screened from the hospital image archive. Among the patients, who presented between January and December 2020, 108 cases that underwent an ankle MRI were identified. Patients with congenital malformations in the foot or ankle, a known history of trauma, and fractures or inflammatory diseases involving the medial of joints, those professionally involved in sports, and those aged below 18 years, were excluded from the study. All the MRI scans that had been performed due to non-traumatic pain, were included.
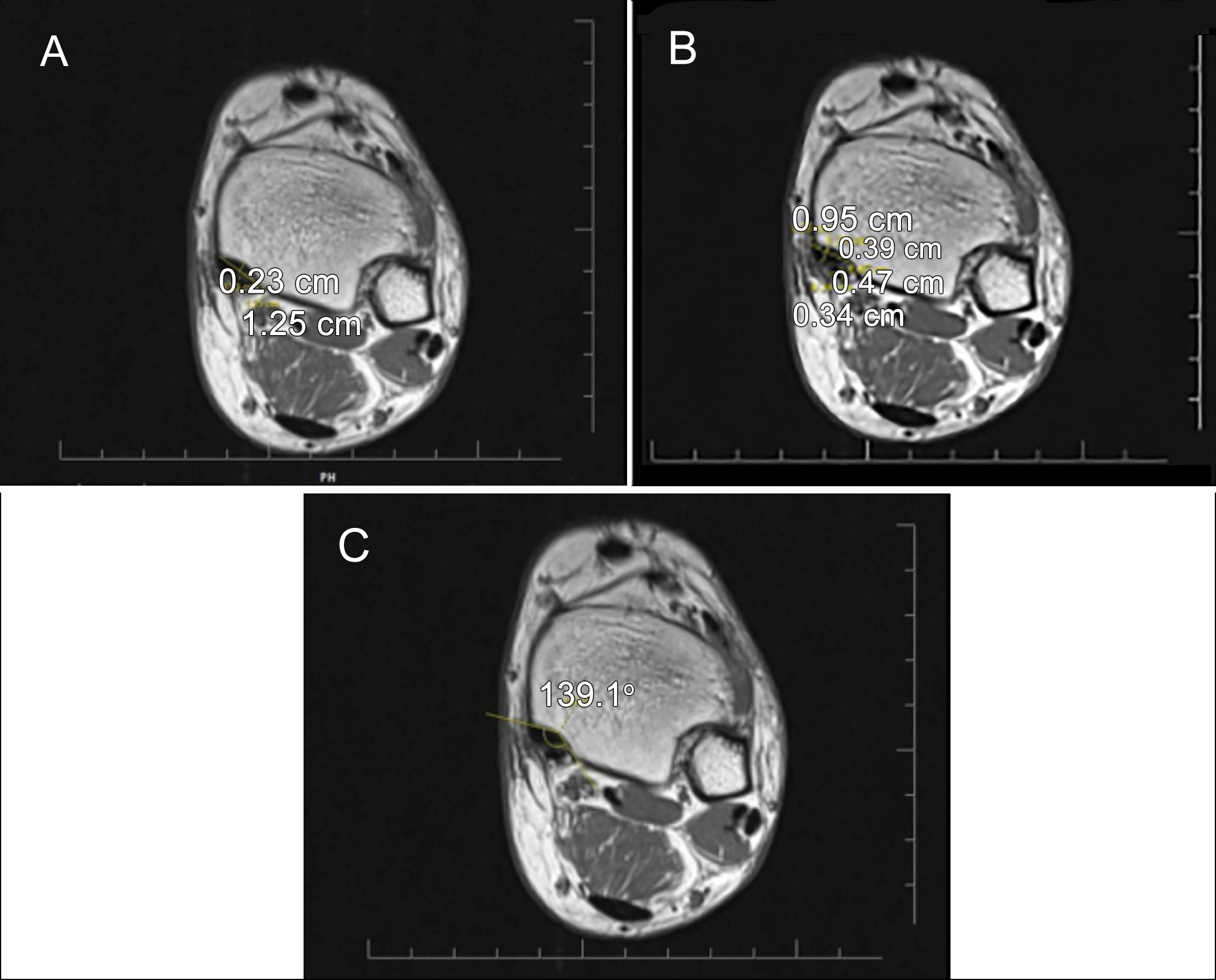 Figure 1: Medial malleolar, posterior tibial tendon (PTT), and flexor digitorum longus tendon (FDLT) measurements from the level where the groove is most prominent. (A) groove depth and width measurement. (B) PTT and FDLT width and depth measurement. (C) groove opening angle measurement.
Figure 1: Medial malleolar, posterior tibial tendon (PTT), and flexor digitorum longus tendon (FDLT) measurements from the level where the groove is most prominent. (A) groove depth and width measurement. (B) PTT and FDLT width and depth measurement. (C) groove opening angle measurement.
All the images were obtained using a MRI device i.e. 1.5T 16 channel foot-ankle coil (Avanto system; Siemens, Erlangen, Germany). T1-weighted axial [repetition time (TR)/echo time (TE): 654/11 ms, slice thickness: 3 mm], sagittal (TR/TE: 500/9.2 ms, slice thickness: 3 mm), T2-weighted fat-suppressed sagittal (TR/TE: 3990/29 ms, slice thickness: 3 mm), fat-suppressed proton-density coronal (TR/TE: 4120/32 ms, slice thickness: 3.5 mm), and axial (TR/TE: 4120/32 ms, slice thickness: 3 mm) sequences were acquired.
The measurements were performed by the experienced radiologist in musculoskeletal radiology. All the measurements were taken twice and averaged. In ten patients, the measurements were repeated at one-week intervals to investigate intra-observer agreement. In addition, the measurements of 30 patients were also made by a second observer to investigate inter-observer agreement. The MMG depth and width measurements were performed in the axial plane at the level where the groove was the most prominent. The farthest distance between the both edges of the groove was defined as the width, and the vertical distance drawn from this line to the deepest part of MMG was recorded as the depth (Figure 1A). The PTT and FDLT width (transverse measurement) and thickness (anteroposterior length) measurements were undertaken in the same plane (Figure 1B). The groove length was determined on the axial plane images by first determining the MMG start and end levels, and then measuring the distance between the two levels on the sagittal images. The groove opening angle (GOA) was measured as the angle between the two ends of the groove width and its deepest part in the axial plane (Figure 1C). The shortest distance from the posterior border of MMG to the level of syndesmosis articulation in the lateral was recorded as the posterior PM (PPM) length. The total PM (TPM) length was measured from the anterior border of MMG as the shortest distance from the lateral syndesmosis articulation. The measurement performed from the middle part of the tibia, where it was the thickest, was noted as the anterior PM (APM) length. All the three measurements are shown in Figure 2.
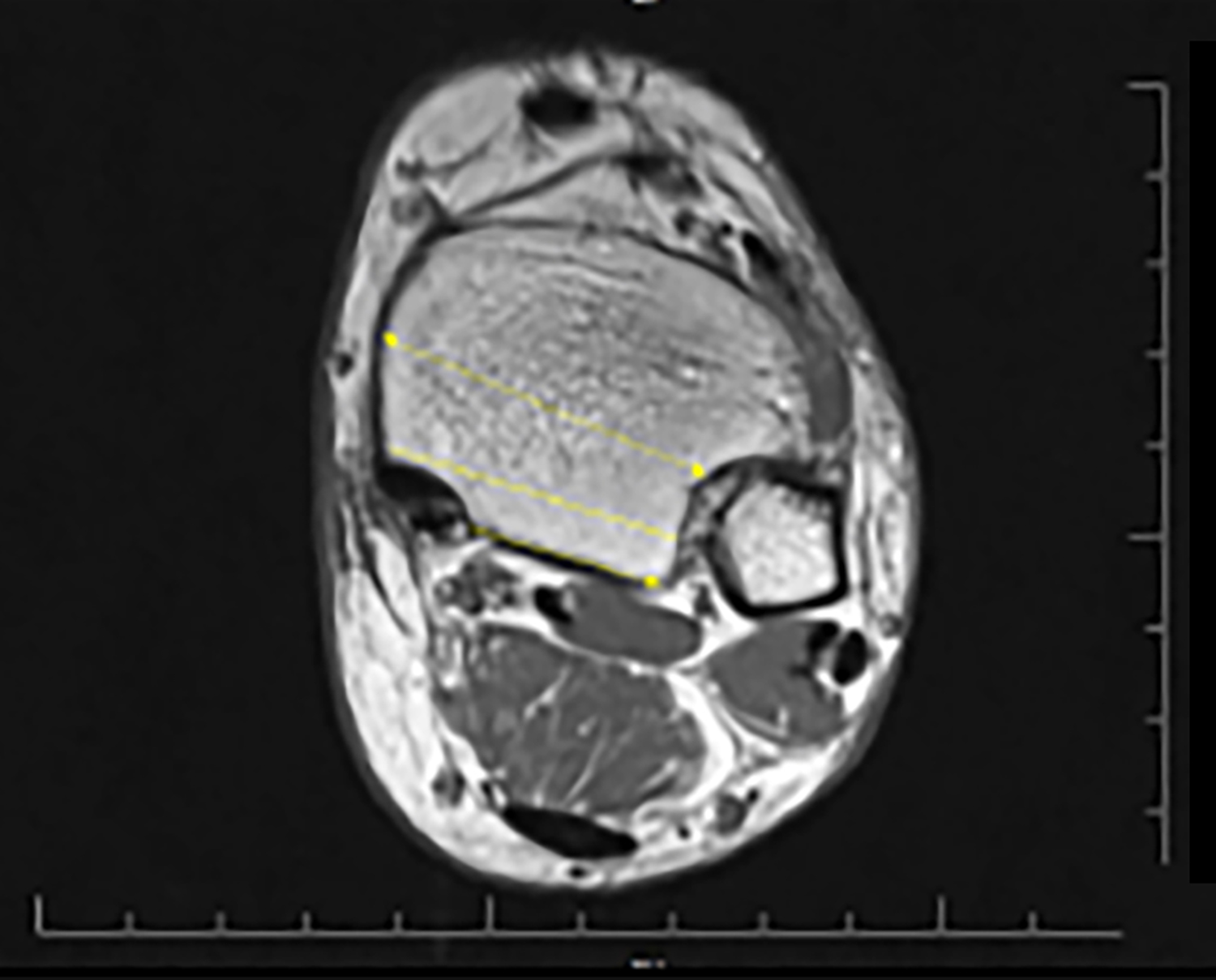 Figure 2: Posterior malleolus (PM) measurements. Anterior (single arrow) measurement from the level of the syndesmosis, total PM length measured from the midline (straight line), and posterior PM length measured as the distance from the groove to syndesmosis (double arrow) in the posterior.
Figure 2: Posterior malleolus (PM) measurements. Anterior (single arrow) measurement from the level of the syndesmosis, total PM length measured from the midline (straight line), and posterior PM length measured as the distance from the groove to syndesmosis (double arrow) in the posterior.
SPSS software package v. 20 was used for the statistical analyses. Mean, standard deviation, minimum, and maximum values were utilised as descriptive statistics for the continuous variables. A p-value of <0.05 was considered statistically significant. Pearson’s correlation coefficient was used to evaluate the correlation between the age and variables. The receiver operating characteristic (ROC) analysis was conducted to determine whether the variables differed between the genders. The intra-class correlation coefficient (ICC) was determined to assess intra-observer and inter-observer agreement. Based on the 95% confidence interval (CI) of the ICC result, values less than 0.5, 0.5-0.75, 0.75-0.90, and those more than 0.90 were evaluated to indicate weak, moderate, good, and excellent reliability, respectively.
RESULTS
A total of 108 patients were initially included in the sample, but since no groove was detected in five (4.6%) patients (three males, and two females), their measurements could not be performed. Of the remaining 103 patients, 61 (59.22%) were females and 42 (40.78%) were males. The mean age of the cases was calculated as 41.06±13.55 (18-81) years, the mean age of the women was 40.01±12.72 (18-73) years, and men was 42.59±14.70 (18-81) years.
The ICC value for intra-observer agreement (95% CI) was calculated as 0.97 (0.96-0.98) (p< 0.001). Good inter-observer agreement (95% CI) was found among the observers for all the parameters (p<0.001). The ICC ranged from a minimum of 0.76 (0.72–0.81) to maximum 0.87 (0.84–0.89). The distribution of the measurements of all the patients and the results of the variables according to gender is shown in Table I. In the evaluation performed according to the genders, all the parameters except GOA, showed statistically significant differences between the women and men (Table II). Among the variables analysed for gender discrimination, the PTT width had a sensitivity of 78.6% and specificity of 72.1%. When the cut-off value was taken as 7.48 mm, the PTT thickness had 76.2% sensitivity and 77% specificity at the cut-off value of 3.88 mm, and the APM length had 85.7% sensitivity and 86.9% specificity at the cut-off value of 40.41 mm.
Table III presents the age-related changes in all the measurements and the relationships between the investigated parameters. There was a statistically significant positive correlation among age, MMG length, and FDLT width; however, it was at a weak level.
The APM, TPM, and PPM length measurements and statistically significantly differed between the genders (Table II). The APM/PPM ratio was calculated as 0.47±0.057 for the women and 0.47±0.060 for the men, indicating no significant difference between the two genders (p=0.398). The TPM/PPM ratio was measured as 0.5±0.604 in the women and 0.56±0.657 in the men, with no statistically significant difference (p=0.804).
DISCUSSION
The literature contains an anthropometric study investigating gender differences in MMG and the tendons passing through this level. One study conducted in 1987 investigated the depth and width of MMG in the 25 cadavers. In that study, the MMG width was measured to vary between 6 and 15 mm, and its depth ranged from 1.5 to 4 mm. In the present research, the MMG width was measured to vary between 9.47 and 19.10 mm, and the MMG depth range was 0.98-4.43 mm, which is in agreement with the previous study.16 One of the important contribution of this study to the literature is to reveal statistically significant differences between the genders concerning the MMG depth, width, and length; PTT and FDLT width and thickness; and PM length. Among these measurements, only GOA has not significantly differ between the genders. There are studies in the literature reporting gender-based differences in the distal measurements and gross dimensions of the tibia.17,18 In a cadaver study, Misiani et al. determined that the MM width and tibial articular surface differed between women and men.17 In this respect, the present findings indicate a significantly greater PM length in the men is in agreement with the literature. However, there is no research in the literature concerning gender determination based on the remaining measurements.
It was also determined that the PTT and FDLT width and thickness statistically and significantly differed according to the gender. Both tendons run within MMG and have an oval-fusiform rather than round shape. In the current study, the width and thickness values were measured as 7.51±1.01 mm and 3.96±0.71 mm respectively for PTT and 4.83±0.74 mm and 3.10±0.61 mm respectively for FDLT. Albano et al. reported that the PTT and FDLT thicknesses as 3.3±0.6 mm and 2.6±0.4 mm, respectively.19 This small difference may be due to the demographic differences in the samples. In addition, the same authors reported that the thickness of both tendons differed between the genders, similar to the current study.
In this study, both the thickness and size of the tendons were measured and found different from the previously available literature. Thus, the relationship between the tendon’s width/groove width and the tendon thickness/groove depth was investigated for both tendons. There was a positively significant relationship between the tendon width and groove width for both tendons. In other words, the wider the tendon was, the wider the groove was. However, contrary to the expectations, there was no statistically significant relationship between the tendon thickness and the groove depth. The PTT thickness/groove depth ratio was measured as 1.96, demonstrating that the tendon was two times thicker compared to the MMG. There was also a statistically significant strong negative relationship between the groove depth and GOA and can be predicted, as MMG got deeper, GOA became narrower. To date, no study has evaluated the MMG measurements in the literature. In case reports and reviews evaluating patients with PTT dislocation, the presence of a shallow MMG in surgical exposure has been defined and suggested to have possibly contributed to the aetiology of dislocation.20-22 A case report described a patient with bilateral convex MM, who presented with bilateral PTT and unilateral FDLT dislocations. In addition, the deepening of MMG in spontaneous dislocations was recommended as the treatment option.14 However, contrary to all these findings, in this study evaluate only asymptomatic patients, MMG was not detected in five (4.6%) cases.
Table I: Distribution of measurements across the patients.|
Total (n = 103) |
Female (n = 61) |
Male (n = 42) |
||||
|
Mean ± SD |
Min-Max |
Mean ± SD |
Min-Max |
Mean ± SD |
Min-Max |
|
|
Age |
41.06 ± 13.55 |
18-81 |
40.01 ± 12.72 |
18-73 |
42.59 ± 14.70 |
18-81 |
|
Groove Width |
14.15 ± 1.86 |
9.47-19.10 |
13.48 ± 1.66 |
9.47-16.68 |
15.11 ± 1.72 |
12.33-19.10 |
|
Groove Depth |
2.06 ± 0.62 |
0.98-4.43 |
1.96 ± 0.53 |
1.00-3.24 |
2.25 ± 0.70 |
0.98-4.43 |
|
Groove Length |
12.07 ± 3.45 |
6.39-22.90 |
11.29 ± 3.29 |
6.39-22.9 |
13.20 ± 6.38 |
7.86-21.17 |
|
Groove Opening Angle |
150.64 ± 9.04 |
131.99-171.87 |
151.04 ± 9.43 |
131.99-171.87 |
150.05 ± 8.51 |
134.16-168.89 |
|
PTT Width |
7.51 ± 1.01 |
5.28-10.14 |
7.14 ± 0.97 |
5.28-10.06 |
8.05 ± 0.82 |
6.55-10.14 |
|
PTT Thickness |
3.96 ± 0.71 |
2.72-5.85 |
3.66 ± 0.50 |
2.72-4.80 |
4.39 ± 0.75 |
2.75-5.85 |
|
FDLT Width |
4.83 ± 0.74 |
3.21-6.92 |
4.53 ± 0.57 |
3.21-5.72 |
5.27 ± 0.76 |
3.82-6.92 |
|
FDLT Thickness |
3.10 ± 0.61 |
2.00-4.99 |
2.88 ± 0.42 |
2.07-3.89 |
3.43 ± 0.69 |
2.00-4.99 |
|
Posterior malleolar Length |
19.42 ± 2.94 |
12.04-27.85 |
18.36 ± 2.45 |
12.04-24.46 |
20.96 ± 2.92 |
16.12-27.85 |
|
Total PM Length |
34.84 ± 3.43 |
28.18-42.50 |
33.07 ± 2.35 |
28.18-41.05 |
37.42 ± 3.11 |
31.24-42.50 |
|
Anterior PM Length |
40.+4 ± 4.09 |
32.71-51.17 |
38.53 ± 2.22 |
32.71-45.21 |
44.45 ± 3.63 |
39.01-51.17 |
|
PTT: Posterior tibial tendon, FDLT: Flexor digitorum longus tendon, PM: Posterior malleolus, SD: Standard deviation. |
||||||
Table II: Performance of the investigated parameters in gender differentiation.
|
Area under the ROC curve (95%) |
Std error |
p |
Cut-off |
Sensitivity (%) |
Specificity (%) |
|
|
Groove Width |
0.742 (0.648-0.836) |
0.048 |
<0.001* |
14.47 |
64.3 |
67.2 |
|
Groove Depth |
0.636 (0.525-0.746) |
0.057 |
0.02* |
2.01 |
64.3 |
60.7 |
|
Groove Length |
0.673 (0.568-0.777) |
0.053 |
0.03* |
12.19 |
61.9 |
65.6 |
|
Groove Opening Angle |
0.465 (0.352-0.578) |
0.058 |
0.0548 |
150.6 |
47.6 |
49.2 |
|
PTT Width |
0.777 (0.688-0.866) |
0.045 |
<0.001* |
7.48 |
78.6 |
72.1 |
|
PTT Thickness |
0.789 (0.693-0.880) |
0.048 |
<0.001* |
3.88 |
76.2 |
77 |
|
FDLT Width |
0.768 (0.675-0.861) |
0.047 |
<0.001* |
4.85 |
71.4 |
70.5 |
|
FDLT Thickness |
0.755 (0.656-0.854) |
0.050 |
<0.001* |
3.01 |
76.2 |
70.5 |
|
Posterior PM Length |
0.741 (0.643-0.840) |
0.050 |
<0.001* |
19.20 |
64.3 |
63.9 |
|
Total PM Length |
0.857 (0.782-0.932) |
0.038 |
<0.001* |
34.68 |
78.6 |
78.7 |
|
Anterior PM Length |
0.930 (0.883-0.977) |
0.024 |
<0.001* |
40.41 |
85.7 |
86.9 |
|
*p<0.05; PTT: Posterior tibial tendon, FDLT: Flexor digitorum longus tendon, PM: Posterior malleolus, ROC: Receiver operating characteristic. |
||||||
Table III: Correlation among the investigated parameters.
|
|
Groove Depth |
Groove Length |
Groove Opening Angle |
PTT Width |
PTT Thickness |
FDLT Width |
FDLT Thickness |
Age |
|
|
Groove Width |
r |
0.252* |
0.069 |
0.104 |
0.541** |
0.361** |
0.282** |
0.430** |
0.052 |
|
p |
0.010 |
0.488 |
0.296 |
0.000 |
0.000 |
0.004 |
0.000 |
0.603 |
|
|
Groove Depth |
r |
0.297** |
-,546** |
0.316** |
0.118 |
0.151 |
0.086 |
0.173 |
|
|
p |
|
0.002 |
0.000 |
0.001 |
0.236 |
0.127 |
0.386 |
0.080 |
|
|
Groove Length |
r |
|
-0.243* |
0.169 |
0.045 |
0.077 |
-0.119 |
0.288 |
|
|
p |
|
|
0.013 |
0.089 |
0.651 |
0.442 |
0.230 |
0.003* |
|
|
Groove Opening Angle |
r |
|
|
-0.225* |
-0.017 |
-0.104 |
-0.029 |
0.067 |
|
|
p |
|
|
|
0.022 |
0.867 |
0.297 |
0.771 |
0.499 |
|
|
PTT Width |
r |
|
|
|
0.403** |
0.449** |
0.464** |
0.167 |
|
|
p |
|
|
|
|
0.000 |
0.000 |
0.000 |
0.091 |
|
|
PTT Thickness
|
r |
|
|
|
|
0.439** |
0.578** |
0.085 |
|
|
p |
|
|
|
|
|
0.000 |
0.000 |
0.393 |
|
|
FDLT Width
|
r |
|
|
|
|
|
0.421** |
0.218 |
|
|
p |
|
|
|
|
|
|
0.000 |
0.027* |
|
|
FDLT Thickness |
r |
|
|
|
|
|
|
|
0.013 |
|
p |
|
|
|
|
|
|
|
0.899 |
|
|
*p <0.05, **p <0.001; PTT: Posterior tibial tendon, FDLT: Flexor digitorum longus tendon, PM: Posterior malleolus. |
|||||||||
Churk-Hang et al. reported that MMG was not present in two (1.6%) of 122 patients. A flat groove is relatively rare in the general population, but non-traumatic PTT dislocation is rarely described in case reports.23 According to all these findings, low-groove depth can be considered a risk factor for dislocation, and it can be suggested that groove deepening may be beneficial in the treatment of these patients. However, in asymptomatic individuals, the MMG depth being half the thickness of PTT and a flat groove seen at a relatively higher rate compared to the dislocation cases suggest that the MMG depth is not the only factor in the aetiology of dislocation; therefore, the evaluation of groove deepening alone may not be sufficient. In future studies, further investigation of these measurements in the symptomatic patients will contribute to the literature.
In this study, the PM length was measured at three levels, and there were significant gender-based differences at all these levels. However, when the TPM/PPM and APM/PPM ratios were examined, they were similar between women and men. The APM/PPM ratio was 0.47±0.057 in the women and 0.47±0.060 in the men, and the TPM/PPM ratio was determined as 0.55±0.604 and 0.56±0.657, respectively. Based on these results, it can be stated that the APM/PPM ratio measured as 0.47 in both genders is important since the PM measurement performed at the level of syndesmosis in the anterior is equal to the total length measured by direct radiography.22 If this intraoperative measurement made on the healthy side in the PM fracture cases on direct radiography is multiplied by the constant number of 0.47, the required length for the PPM measurement for the PM plating can be found. Similarly, in the literature, Hang et al. conducted a study using computed tomography and determined this ratio as 0.49.23 The slight difference in the rates obtained from the two studies may be due to the differences in patient populations. Another ratio, TPM/PPM, can also be used to calculate plating length. However, this would require cross-sectional imaging to be performed before the surgery.
One of the main limitations of this study is the evaluation of only asymptomatic patients. A further study can be planned with both symptomatic and asymptomatic patient groups of the similar gender and age. The studies to be conducted with PTT dislocation cases will also significantly contribute to the literature on this subject.
CONCLUSION
The groove depth, width, and length; PTT and FDLT width and thickness; and TPM, PPM, and APM length can be used in gender differentiation. In addition, it will be useful to know these values in the cases of fractures and before the surgical procedures, such as groove deepening. Furthermore, using these parameters in gender discrimination will contribute to the forensic identification. Lastly, the presence of asymptomatic cases without MMG indicates that other pathologies should also be considered in addition to the depth of MMG.
ETHICAL APPROVAL:
Ethics Committee approval was waived by the Ethics Committee of Yildirim Beyazit University Yenimahalle Education and Research Hospital (Date: 26 May 2021, Approval No. 2021-07-01).
PATIENTS’ CONSENT:
Written consent was obtained from the patients before MRI examination.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
EE: Design of the research, manuscript writing, statistical analysis, and acquisition of data.
UT: Carried out the analysis and interpretation of data, drafted the manuscript, and critical revisions.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Schweitzer ME, Karasick D. MR imaging of disorders of the posterior tibialis tendon. AJR Am J Roentgenol 2000; 175(3):627-35. doi: 10.2214/ajr.175.3.1750627.
- Wang Z, Yuan C, Zhu G, Geng X, Zhang C, Huang J, et al. A Retrospective study on the morphology of posterior malleolar fractures based on a CT scan: Whether we ignore the importance of fracture height. Biomed Res Int 2020; 29:2903537. doi: 10.1155/2020/2903537.
- Klammer G, Kadakia AR, Joos DA, Seybold JD, Espinosa N. Posterior pilon fractures: A retrospective case series and proposed classification system. Foot Ankle Int 2013; 34(2):189-99. doi: 10.1177/1071100712469334.
- Palmanovich E, Brin YS, Laver L, Kish B, Nyska M, Hetsroni I. The effect of minimally displaced posterior malleolar fractures on decision making in minimally displaced lateral malleolus fractures. Int Orthop 2014; 38(5): 1051-6. doi: 10.1007/s00264-013-2224-7.
- Boraiah S, Gardner MJ, Helfet DL, Lorich DG. High association of posterior malleolus fractures with spiral distal tibial fractures. Clin Orthop Relat Res 2008; 466(7):1692-8. doi: 10.1007/s11999-008-0224-5.
- Kukkonen J, Heikkilä JT, Kyyrönen T, Mattila K, Gullichsen E. Posterior malleolar fracture is often associated with spiral tibial diaphyseal fracture: A retrospective study. J Trauma 2006; 60(5):1058-60. doi: 10.1097/01.ta.0000 196700.74272.10.
- Gardner MJ, Streubel PN, McCormick JJ, Klein SE, Johnson JE, Ricci WM. Surgeon practices regarding operative treatment of posterior malleolus fractures. Foot Ankle Int 2011; 32(4):385-93. doi: 10.3113/FAI.2011.0385.
- Erdem MN, Erken HY, Burc H, Saka G, Korkmaz MF, Aydogan M. Comparison of lag screw versus buttress plate fixation of posterior malleolar fractures. Foot Ankle Int 2014; 35(10):1022-30. doi: 10.1177/107110071 4540893.
- OʼConnor TJ, Mueller B, Ly TV, Jacobson AR, Nelson ER, Cole PA. "A top" screw versus posterolateral plate for posterior malleolus fixation in trimalleolar ankle fractures. J Orthop Trauma 2015; 29(4):e151-6. doi: 10.1097/BOT. 0000000000000230.
- De Vries JS, Wijgman AJ, Sierevelt IN, Schaap GR. Long-term results of ankle fractures with a posterior malleolar fragment. J Foot Ankle Surg 2005; 44(3):211-7. doi: 10.1053/j.jfas.2005.02.002.
- Li YD, Liu SM, Jia JS, Zhou JL. Choice of internal fixation methods for posterior malleolus fracture in both biomechanics and clinical application. Beijing Da Xue Xue Bao Yi Xue Ban 2011; 43(5):718-23.
- Ballesteros R, Chacón M, Cimarra A, Ramos L, Gómez-Barrena E. Traumatic dislocation of the tibialis posterior tendon: A new surgical procedure to obtain a strong reconstruction. J Trauma 1995; 39(6):1198-200. doi: 10.1097/00005373-199512000-00037.
- Goucher NR, Coughlin MJ, Kristensen RM. Dislocation of the posterior tibial tendon: A literature review and presentation of two cases. Iowa Orthop J 2006; 26:122-6.
- Waldron JE, Bernhardson AS, Fellars TA. Unilateral dislocation of the posterior tibialis tendon (PTT) and flexor digitorum longus tendon with contralateral PTT subluxation in a patient with congenitally shallow flexor groove. Foot Ankle Spec 2017; 10(5):480-3. doi: 10.1177/ 1938640017699062.
- Gluck GS, Heckman DS, Parekh SG. Tendon disorders of the foot and ankle, part 3: The posterior tibial tendon. Am J Sports Med 2010; 38(10):2133-44. doi: 10.1177/036354 6509359492.
- Soler RR, Gallart Castany FJ, Riba Ferret J, Garcia Ramiro S. Traumatic dislocation of the tibialis posterior tendon at the ankle level. J Trauma 1986; 26(11):1049-52. doi: 10.1097/00005373-198611000-00016.
- Misiani MK, Amuti T, Darbar S, Mandela P, Maranga E, Obimbo M. Sex determination from dimensions of distal tibiae in adult Kenyans: A discriminant function analysis. Transl Res Anat 2020; 20:100075. doi.org/10.1016/j.tria. 2020.100075.
- Sherk VD, Bemben DA, Bemben MG, Anderson MA. Age and sex differences in tibia morphology in healthy adult Caucasians. Bone 2012; 50(6):1324-31. doi: 10.1016/j. bone.2012.03.005.
- Albano D, Cortese MC, Duarte A, Messina C, Gitto S, Vicentin I, et al. Predictive role of ankle MRI for tendon graft choice and surgical reconstruction. Radiol Med 2020; 125(8):763-9. doi: 10.1007/s11547-020-01177-z.
- Healy WA, Starkweather KD, Gruber MA. Chronic dislocation of the posterior tibial tendon. A case report. Am J Sports Med 1995; 23(6):776-7. doi: 10.1177/036 354659502300625.
- Langan P, Weiss CA. Subluxation of the tibialis posterior, a complication of tarsal tunnel decompression: A case report. Clin Orthop Relat Res 1980; 146:226-7.
- Perlman MD, Wertheimer SJ, Leveille DW. Traumatic dislocations of the tibialis posterior tendon: A review of the literature and two case reports. J Foot Surg 1990; 29(3):253-9.
- Churk-Hang CL, Cheung M-H, Ka-Kin SL, Ma C-M. Appropriate choice of plate for the posterior malleolus: Computed tomography study of 122 chinese adult patients. J Orthop Trauma Rehabil 2017; 23:25-9. doi.org/10.1016/j.jotr.2016.06.003.