Pancreatic Abscess Misdiagnosed and Treated as Pancreatic Cancer
By Deng-Yong Zhang, Zheng LuAffiliations
doi: 10.29271/jcpsp.2021.04.472ABSTRACT
A preoperative diagnosis of pancreatic cancer is not hundred percent accurate. Because of the uncertainty in the diagnosis of pancreatic tumours, some benign pancreatic diseases have been misdiagnosed as pancreatic cancer and treated with surgical resection. This approach has a significant negative impact on the physical and psychological well-being of the patients. Herein, we report a case of a pancreatic abscess misdiagnosed as pancreatic cancer. The patient recovered well after total pancreaticoduodenectomy, without any postoperative complications. However, total pancreaticoduodenectomy has possible future adverse consequences. Therefore, our case findings highlight the need that clinicians should be aware of the differential diagnosis of pancreatic cancer and consider the possibility of a pancreatic abscess preoperatively, especially in patients with diabetes. Laparoscopic exploration is recommended to avoid the trauma caused by an open surgery.
Key Words: Pancreatic cancer, Abscess, Surgery.
INTRODUCTION
Pancreatic cancer has a poor prognosis and is the third leading cause of mortality worldwide.1 Its diagnosis is dependent on the presence of obstructive jaundice, raised blood carbohydrate antigen 19-9 (CA 19-9) levels, and computed tomography (CT) findings. Some patients with a tumour of the pancreatic head or uncinated process may present with obstructive jaundice. On CT, it often manifests as an enhancing lesion. An elevated postoperative CA 19-9 level may predict poor survival in the perioperative and postoperative periods.2 Some patients with pancreatic cancer are complicated with diabetes and often have a worse prognosis than those without diabetes.3 However, the gold standard for diagnosing a pancreatic lesion is the pathological examination. Thus, some patients with typical clinical symptoms and findings may not have a pancreatic carcinoma. Herein, we describe a case of a pancreatic abscess misdiagnosed as pancreatic cancer.
CASE REPORT
A 27-year male visited our Department for a pancreatic tumour found on ultrasonic examinations, when he visited the hospital for diabetes two weeks ago. He had no fever, abdominal pain, or jaundice.
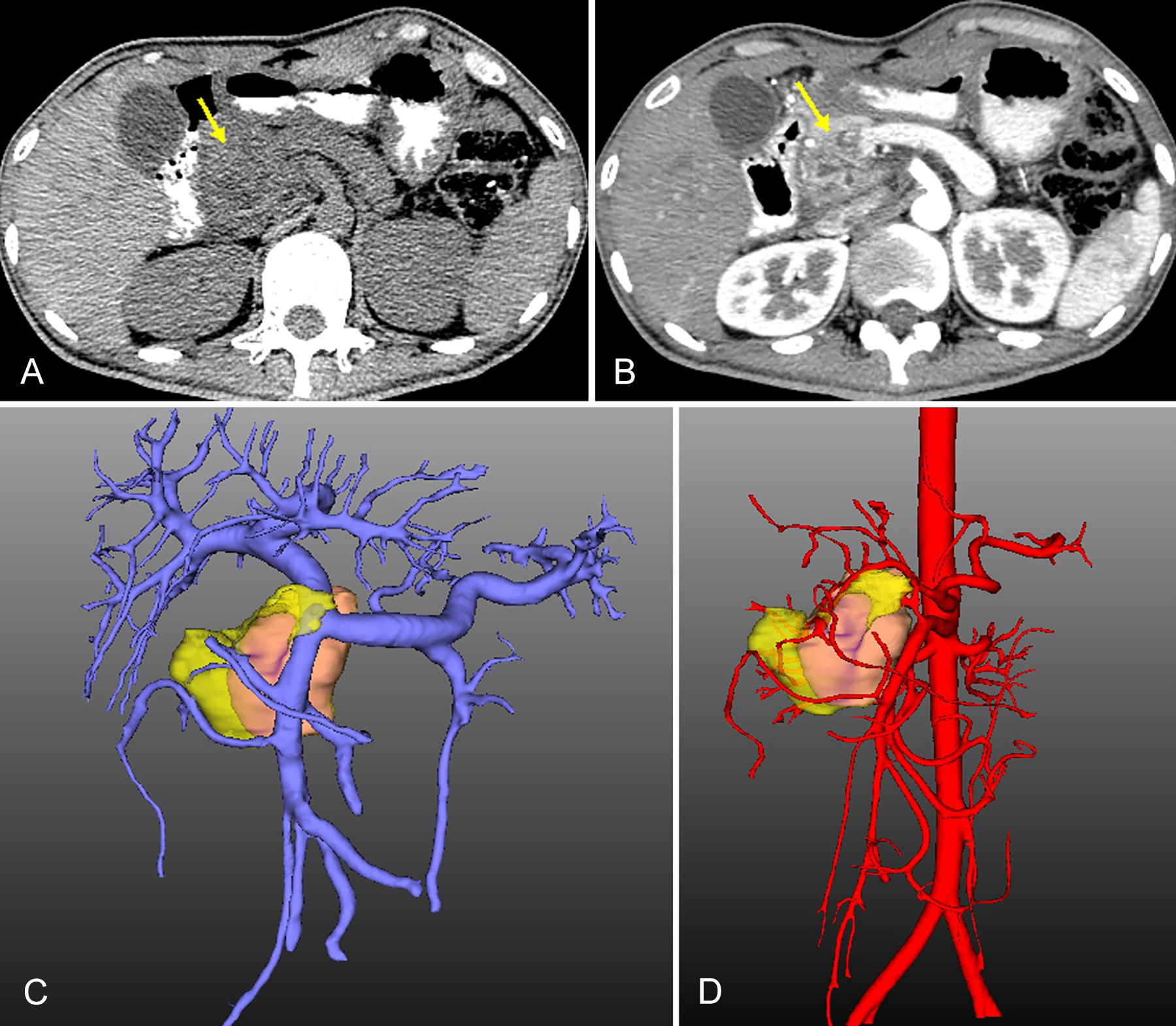 Figure 1: Preoperative computed tomography (CT) and three-dimensional reconstruction. (A and B) CT scan shows the mass (yellow arrow) located in the head of the pancreas with heterogeneous enhancement. (C and D) The three-dimensional reconstruction shows the anatomical positional relationships between the tumour (pink), pancreas (yellow), portal vein, and hepatic artery.
Figure 1: Preoperative computed tomography (CT) and three-dimensional reconstruction. (A and B) CT scan shows the mass (yellow arrow) located in the head of the pancreas with heterogeneous enhancement. (C and D) The three-dimensional reconstruction shows the anatomical positional relationships between the tumour (pink), pancreas (yellow), portal vein, and hepatic artery.
However, the ultrasonic examination showed dilatation of the intrahepatic and extrahepatic bile ducts. He had a 7-year history of diabetes with poor blood sugar control at home. His blood CA 19-9 level was 45.58 U/mL, leukocyte count was 6.33×109/L, hepatitis B surface antigen and hepatitis B surface antibody were positive, and total bilirubin level was normal. CT scan showed an irregular soft tissue density lesion located in the pancreatic head with heterogeneous enhancement (Figure 1A and B), severe atrophy of the pancreatic body and tail (Figure 1C and D), and enlargement of the gallbladder and spleen. The three-dimensional reconstruction indicated that the tumour had not invaded the main artery and vein (Figure 1C and D). His fingertip blood glucose level fluctuated (1.9-27.6 mmol/L) during hospitalisation, although he received insulin regularly.
The possibility of a malignant pancreatic tumour was considered based on preoperative findings. Therefore, we conducted total pancreaticoduodenectomy. Intraoperatively, we found a firm tumour located in the head of the pancreas and atrophy of the pancreatic body and tail.
Postoperative pathology showed suppurative inflammation with abscess formation in the pancreatic head with a diameter of 3.0 cm. Fluctuation in the fingertip blood glucose level (4.1-14.9 mmol/L) also continued postoperatively even while receiving regular insulin.
The patient was cured and discharged on day 12 postoperatively. At the 12-month follow-up, his blood glucose level was controlled and stable at home.
DISCUSSION
A pancreatic abscess usually occurs as a complication of pancreatitis or secondary to tuberculosis.4 Rarely, a pancreatic abscess can also be secondary to diabetes and foreign bodies in the gastrointestinal tract.5,6 Some patients with a pancreatic abscess have diabetes, but a relationship between diabetes and the abscess is rarely illustrated. Kim et al. reported four cases of pancreatic abscess; three patients had diabetes, and three had a normal blood CA 19-9 level.7 A pancreatic abscess without fever and an elevated leukocyte count but with diabetes has been rarely reported. Our case was rare in that the patient just had an elevated CA 19-9 level. A malignant pancreatic tumour (mucus or serous) was more likely to be considered preoperatively. Preoperative distinction of pancreatic cancer from a pancreatic abscess can sometimes be difficult.8 Preoperative endoscopic ultrasound-guided (EUS) biopsy is an important tool for preoperative diagnosis and staging of pancreatic cancer. The 2017 National Comprehensive Cancer Network (NCCN) guidelines indicate that for patients with adenocarcinoma, especially pancreatic malignancies, EUS biopsy is not necessary preoperatively.9 Therefore, we did not conduct this biopsy before surgery.
Poor blood sugar control in patients with diabetes may lead to decreased immunity and an increased risk of infection. In our case, the pancreatic abscess may have resulted from the large fluctuation in blood sugar levels and long history of diabetes. However, our patient had no fever or elevated leukocyte count to indicate inflammation, leading to misdiagnosis. We speculate that the pancreatic abscess may have been more limited and did not spread to cause systemic symptoms in our case. Surgical resection, intravenous antibiotics, puncture drainage, and other methods can be used to treat a pancreatic abscess.6 Considering that many complications are associated with surgery, antibiotics alone or in combination with a drainage tube can achieve good results.6, 10
It is rare for patients with a pancreatic abscess to have no fever, elevated leukocyte count, or abdominal pain. Our patient was misdiagnosed as having pancreatic carcinoma and underwent total pancreaticoduodenectomy. Although, he recovered well postoperatively, the surgical trauma was an inconvenience. The possibility of a pancreatic abscess should be considered preoperatively, especially in patients with diabetes. Laparoscopic exploration is recommended for these cases, and an intraoperative biopsy can be used to easily differentiate between pancreatic cancer and an abscess. If a pancreatic abscess is found, a drainage tube can be used to help reduce the trauma caused by open surgery.
PATIENT'S CONSENT:
The patient's informed consent has been obtained.
CONFLICT OF INTEREST:
The authors report no conflict of interest in this work, and they did not use any outside assistance in preparing the manuscript.
AUTHORS' CONTRIBUTION:
DZ: Authored the original draft.
ZL: Reviewed and edited this paper.
REFERENCES
- Wu W, He X, Yang L, Wang Q, Wang Q, Bian X, et al. Rising trends in pancreatic cancer incidence and mortality in 2000-2014. Clin Epidemiol 2018; 9:789-97. doi: 10.2147/ CLEP.S160018. eCollection 2018.
- Kondo N, Murakami Y, Uemura K, Nakagawa N, Nakagawa N, Takahashi S, et al. Comparison of the prognostic impact of pre- and post-operative CA19-9, SPan-1, and DUPAN-II levels in patients with pancreatic carcinoma. Pancreatology 2017; 17(1):95-102. doi: 10.1016/j.pan.2016.10.004.
- Hui shen, Ming Zhan, Wei Wang, Yang D, Wang J. Impact of diabetes mellitus on the survival of pancreatic cancer: A meta-analysis. Onco Targets Ther 2016; 9:1679-88. doi: 10.2147/OTT.S95744. eCollection 2016.
- Singhai P, Gadhadh R, Joshi S, Krishnan S, Aparna. Isolated pancreatic tuberculosis in an immunocompetent host. J Assoc Physicians India 2017; 65(12):98-100.
- Garment AR, Schwartz MB. Foreign body-induced abscess resembling pancreatic neoplasia. J Gen Intern Med 2012; 27(11):1561-64. doi: 10.1007/s11606-012-2064-y.
- Shulik O, Cavanagh Y. Pancreatic Lesion: Malignancy or abscess? Am J Case Rep 2016; 17:337-9. doi: 10.12659/ ajcr.895621.
- Kim MJ, Seo EK, Kang ES, Kim KM, Oh YM, Cho BH, et al. Pyogenic pancreatic abscess mimicking pancreatic neoplasm: A four-case series. Korean J Gastroenterol 2015; 65(4):252-7. DOI: 10.4166/kjg.2015.65.4.252
- Bhattarai M, Bansal P, Diehl D. Pancreatic abscess: An unusual presentation of pancreatic tail cancer. J Nepal Health Res Counc 2015; 13(3):245-7.
- Tempero MA, Malafa MP, Al-Hawary M, Asbun H, Bain A, Behrman SW, et al. Pancreatic adenocarcinoma, version 2.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 2017; 15(8):1028-61. doi: 10.6004/ jnccn.2017.0131.
- Lee JY, Kim TH. Isolated pyogenic pancreatic abscess successfully treated via endoscopic ultrasound-guided drainage. Korean J Gastroenterol 2017; 69(5):321-4. doi: 10.4166/kjg.2017.69.5.321.