A Rare Presentation of Extramedullary Hematopoiesis: Perirenal Masses
By Selahattin Durmaz1, Cennet Sahin2, Muzaffer Basak2, Sukru Mehmet Erturk1Affiliations
doi: 10.29271/jcpsp.2022.04.28ABSTRACT
Extramedullary hematopoiesis (EMH) is a physiological compensatory mechanism that develops in response to ineffective or insufficient hematopoiesis. Although the liver and spleen are the most common sites, EMH may occur anywhere in the body. Peri-renal involvement in EMH is quite rare and mimics tumoral lesions. To our knowledge, 12 peri-renal EMH cases have been reported in the literature so far.
A 57-year woman was admitted to our hospital with non-specific abdominal pain. She had a history of chronic renal failure. On physical examination, diffuse abdominal tenderness and mild rigidity were detected. Blood tests revealed bicytopenia and elevated acute phase reactants. On non-contrast abdominal computed tomography (CT) scan, two peri-renal mass lesions of 4.5 cm and 4 cm were detected incidentally on the right side. Tumoral lesions were considered in the differential diagnosis, and magnetic resonance imaging (MRI) and positron emission tomography-computed tomography (PET-CT) were performed. Lesions showed mild hypermetabolic activity (SUVmax: 4,68) on PET-CT images. For the definitive diagnosis, an ultrasound-guided core needle biopsy was performed. The histopathological examination was consistent with EMH.
This case aims to highlight the peri-renal involvement of EMH, which mimics renal and peri-renal malignancies.
Key Words: Extramedullary hematopoiesis, Kidney, Computed tomography, Magnetic resonance imaging.
INTRODUCTION
Extramedullary hematopoiesis (EMH) is defined as the production and maturation of blood elements outside the medullary cavity.1 After birth, hematopoiesis only occurs in the bone marrow, and any extramedullary site of hematopoiesis is considered abnormal. EMH frequently develops due to bone marrow suppression or hematologic diseases, such as idiopathic myelofibrosis and hemoglobinopathies. Besides this, it may also develop without chronic anemia, and some malignant processes may be the cause of this entity.2,3 Although the clinical presentation of EMH is generally asymptomatic and detected incidentally, patients may also present with involved organ-specific symptoms including neurological symptoms with nervous system involvement, acute renal failure with renal involvement, or dyspnea with lung involvement. The liver and spleen are the most common sites of EMH; however, it may also occur in the retroperitoneum and kidneys. Based on radiologic appearance, renal and peri-renal involvement of EMH generally mimics primary renal malignancies and metastasis. This similarity may lead to unnecessary nephrectomies. A biopsy is frequently warranted for the definitive diagnosis.4
Herein, we report a quite rare case of EMH manifesting as peri-renal masses. We aim to emphasise renal and peri-renal involvement of EMH, which can easily be mistaken for renal and peri-renal malignancies.
CASE REPORT
A 57-year woman was admitted to our hospital with fever and abdominal pain. She had a history of chronic renal failure and was treated with erythropoietin because of chronic anemia. On physical examination, diffuse abdominal tenderness and mild rigidity were detected. Blood tests revealed bicytopenia (Red blood cells: 3.12×1012/L, hemoglobin: 9.2 g/dL, hematocrit: 30.4%, platelets: 108×109/L), elevation of acute phase reactants (C-reactive protein: 256.6 mg/L, procalcitonin: 16 ug/L, and white blood cells: 6.24×109/L). Non-contrast abdominal computed tomography (CT) was performed to rule out acute abdominal pathologies. Intravenous (IV) contrast medium was not administered because of the known contrast medium allergy of the patient. On CT scan, two well-circumscribed, peri-renal lesions of 4.5 cm and 4 cm were detected. The patient was asked if she had any previous imaging studies. On review of CT images (Figure 1) acquired one year ago, two lesions measuring 1.5 cm and 0.9 cm were detected. Considering appearances, locations, and the increase in the size of the lesions, primary renal malignancies, including renal cell cancer and renal lymphoma, were considered in the differential diagnosis. Magnetic resonance imaging (MRI) and positron emission tomography-CT (PET-CT) were performed.
In non-enhanced MRI (Figure 2), lesions appeared slightly hyperintense on T1-weighted images (WIs) and slightly hypointense on T2-WIs. No fat content was detected on chemical shift imaging and fat-suppressed images. On PET-CT images (Figure 2), lesions showed mild hypermetabolic activity (SUVmax: 4,68). An ultrasound-guided core needle biopsy was performed to rule out malignancy. In the histopathological examination, hematopoietic elements of all three cell lineages, including megakaryocytes, erythroid cells, and maturing myeloid cells, were observed (Figures 3 and 4). Further, immunohistochemical analysis showed CD61, glycophorin A and myeloperoxidase (MPO) positivity (Figures 5 and 6). Overall, the histopathological findings were consistent with EMH.
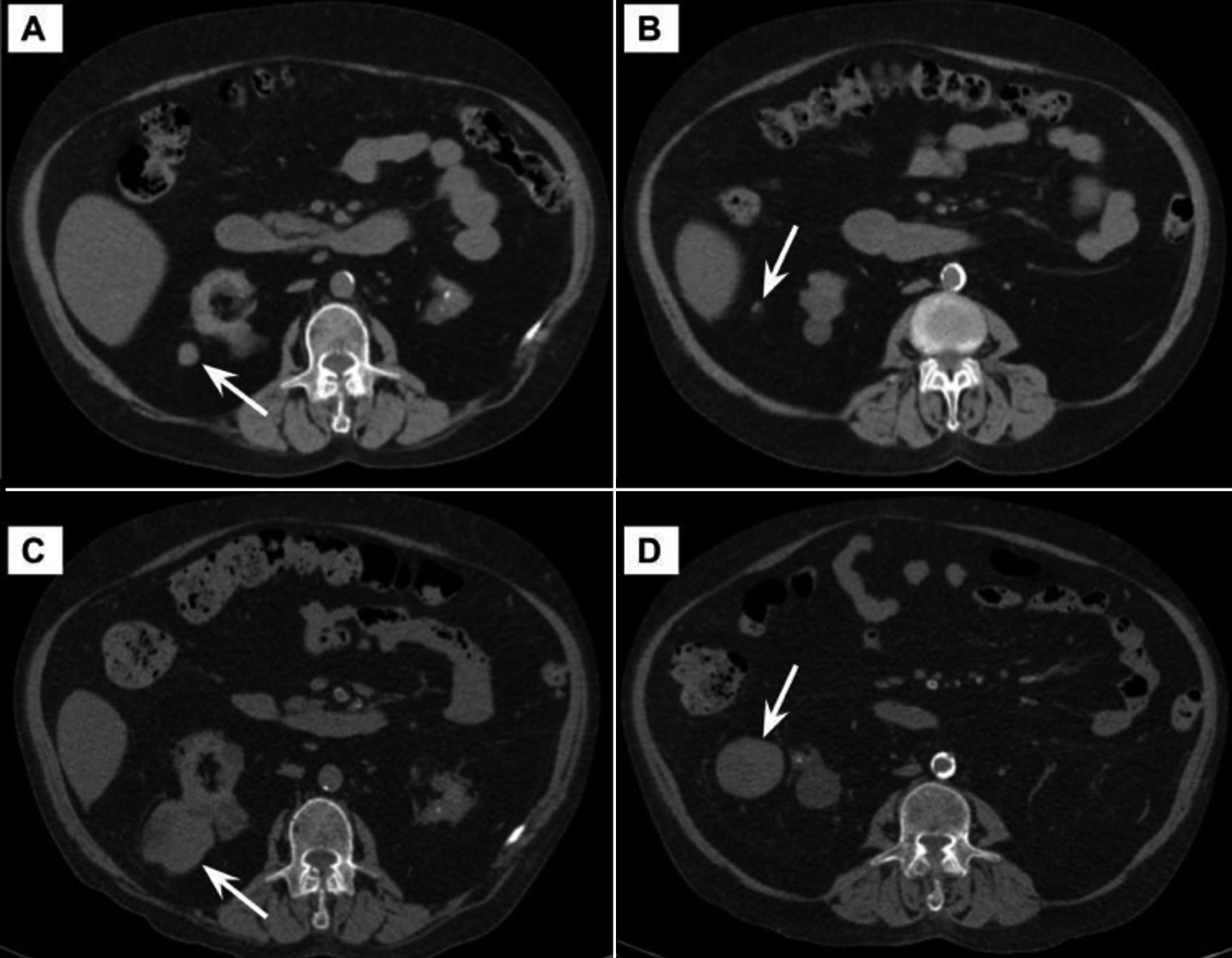 Figure 1: Non-contrast CT images (A,B) show two perirenal nodular lesions (arrows) of 1.5 cm and 1 cm in size. Note the sharp increase in size on CT images (C,D) obtained one year later (arrows).
Figure 1: Non-contrast CT images (A,B) show two perirenal nodular lesions (arrows) of 1.5 cm and 1 cm in size. Note the sharp increase in size on CT images (C,D) obtained one year later (arrows).
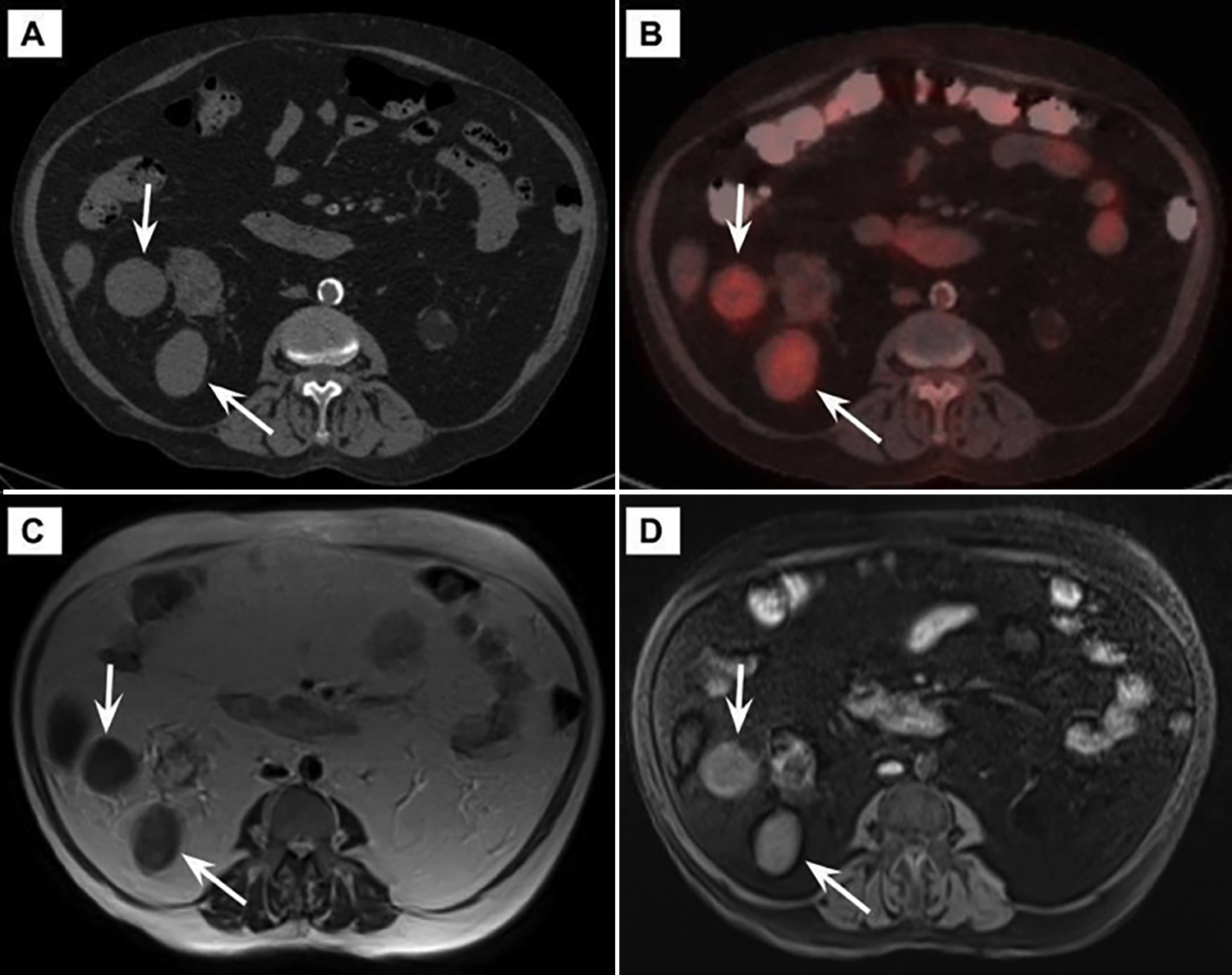 Figure 2: CT (A), PET-CT (B), and MR images (T2-WI (C), fat-suppressed pre-contrast T1-WI (D)) of two well-circumscribed, perirenal solid lesions (arrows) diagnosed with EMH.
Figure 2: CT (A), PET-CT (B), and MR images (T2-WI (C), fat-suppressed pre-contrast T1-WI (D)) of two well-circumscribed, perirenal solid lesions (arrows) diagnosed with EMH.
DISCUSSION
EMH is a physiological compensatory mechanism that develops in response to ineffective or insufficient hematopoiesis.5 It occurs in tissues and organs, in which, physiological hematopoiesis occurs in fetal life. It is often a diffuse process and tumor-like presentation is quite rare. The liver and spleen are the most common locations of EMH, and hepatosplenomegaly is the most frequent presentation of this entity.6 Non-hepatosplenic EMH, which is rarely encountered, may develop in almost all tissues and organs, and mimics tumoral lesions.1
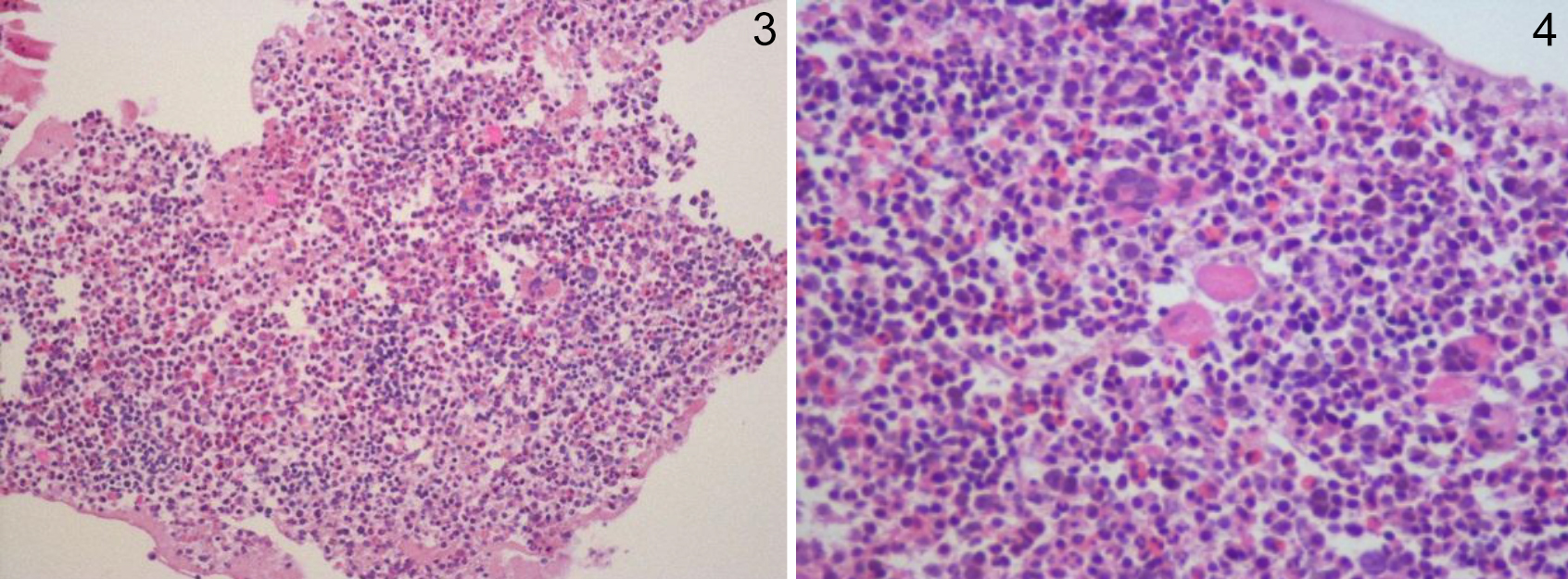 Figures 3 & 4: Sections of core needle biopsy demonstrating hematopoietic cells, including megakaryocytes, erythroid cells, and maturing myeloid cells (H&E, ×200,×400).
Figures 3 & 4: Sections of core needle biopsy demonstrating hematopoietic cells, including megakaryocytes, erythroid cells, and maturing myeloid cells (H&E, ×200,×400).
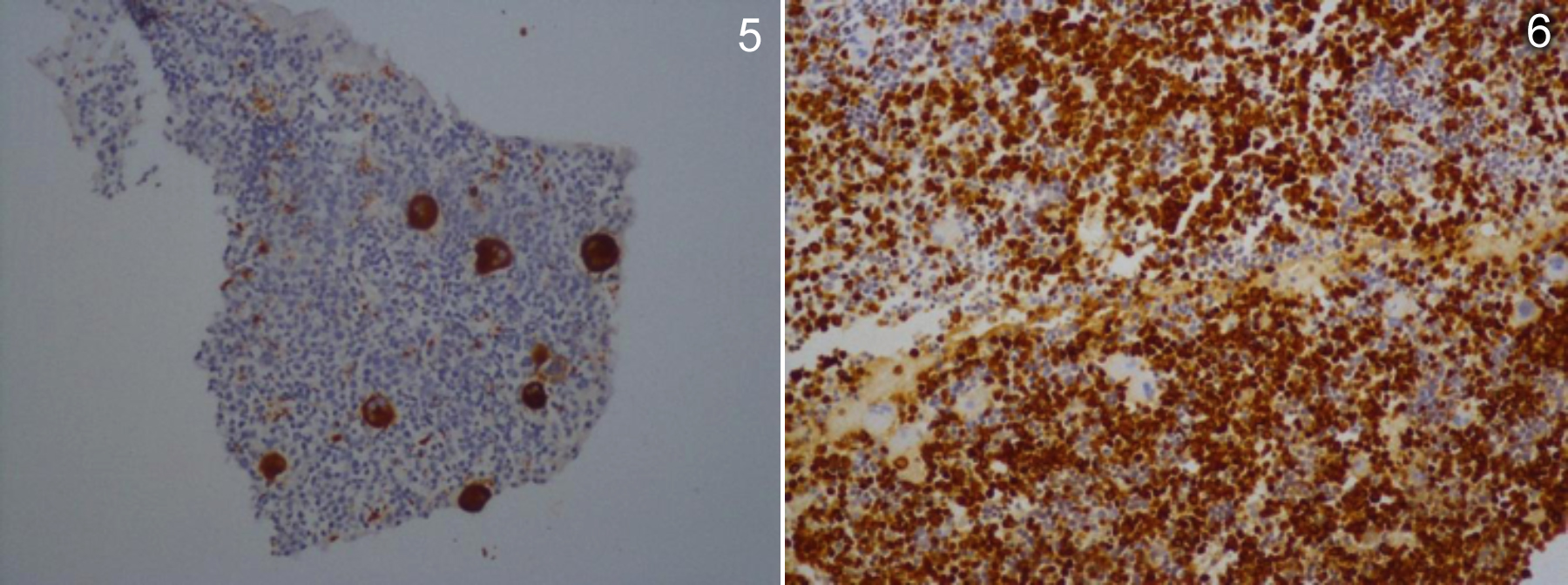 Figures 5 & 6: Maturing myeloid cells as confirmed by immunohistochemistry for myeloperoxidase (MPO, ×400), and megakaryocytes, as confirmed by immunohistochemistry for CD61 (CD61, ×400).
Figures 5 & 6: Maturing myeloid cells as confirmed by immunohistochemistry for myeloperoxidase (MPO, ×400), and megakaryocytes, as confirmed by immunohistochemistry for CD61 (CD61, ×400).
Mass-like EMH generally appears as heterogeneous, hypovascular, soft tissue lesion on CT images.6 Depending on the presence of blood products of different ages, EMH may show heterogeneous T1 and T2 signal characteristics on MRI.7 Detection of the microscopic fat component on chemical shift imaging can be beneficial to make the diagnosis.6
On PET-CT images, these lesions may show mild hypermetabolic activity, as in our case.8 Technetium-99m (Tc-99m) colloid scintigraphy is another tool that detects bone marrow components in hematopoietic foci. It may help in the diagnosis of EMH, but the probability of false negativity should be kept in mind.6,7
Peri-renal sites are active during in-utero hematopoiesis.1,6 Renal involvement of EMH can be divided into three types, including parenchymal, parapelvic, or peri-renal. In the parenchymal type, EMH may appear as either a diffuse enlargement of the kidney or a focal solid mass lesion, which is indistinguishable from malignancy. Parapelvic involvement is another manifestation, and these cases may present with acute renal failure due to obstruction. Perirenal type generally presents as bilateral soft tissue lesions that surround both kidneys but do not cause any functional or contour abnormalities.9
Parapelvic and peri-renal EMH generally show bilateral involvement, but less frequently they may also be unilateral, as in our case.5,9 The patients may be either asymptomatic or present with acute renal failure due to obstruction or extensive renal parenchymal involvement.5
The differential diagnosis of peri-renal and renal masses is quite broad; tumoral lesions such as renal cell cancer and lymphoma, inflammatory conditions like xanthogranulomatous pyelonephritis, and some proliferative disorders including EMH and retroperitoneal fibrosis can be given as examples. Although the differential diagnosis may be narrowed by the patient's clinical history and imaging features, biopsy is inevitable in many cases, especially to rule out malignancy.10 Since these lesions are rich in blood vessels and hemorrhagic, the possibility of post-biopsy bleeding should be kept in mind. Fine-needle aspiration or core-needle biopsy can be preferred depending on the location of the lesions.6,11
Compared with other locations of EMH, peri-renal involvement is quite rare and generally bilateral.5,9 The vast majority of EMH cases occur secondary to several types of hematologic disorders including idiopathic myelofibrosis, thalassemia major, sickle cell anemia, and other chronic myeloproliferative neoplasms.2,12 In the present study, two separate mass lesions located in the right peri-renal space were detected, and one of them appeared to be originating from the right kidney. Our patient did not have any hematologic disorders. Chronic renal failure was the only suspected entity that may be the cause of EMH.
To our knowledge, only 12 peri-renal EMH cases have been reported in the literature so far. Unilateral involvement, lack of any hematologic disorders, and the association with chronic renal failure make this peri-renal EMH case, to some extent, unique.
In conclusion, EMH lesions do not have specific imaging features; therefore, clinical history plays a vital role in the differential diagnosis. In patients with renal, peri-renal, or parapelvic tumor-like solid lesions, a history of chronic hematological disease or chronic renal failure should bring in mind the possibility of EMH.
ACKNOWLEDGEMENT:
We thank Kamile Gulcin Eken, for providing the photomicrographs and related figure legends.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHOR’S CONTRIBUTION:
SD: Data acquisition and interpretation, drafting, final approval.
CS: Data acquisition, critical revision and final approval.
MB: Interpretation, critical revision and final approval.
SME: Data analysis and interpretation, editing and critical revision, final approval.
REFERENCES
- Georgiades CS, Neyman EG, Francis IR, Sneider MB, Fishman EK. Typical and atypical presentations of extramedullary hemopoiesis. AJR Am J Roentgenol 2002; 179(5):1239-43. doi: 10.2214/ajr.179.5.1791239.
- Bao Y, Liu Z, Guo M, Li B, Sun X, Wang L. Extramedullary hematopoiesis secondary to malignant solid tumors: A case report and literature review. Cancer Manag Res 2018 10:1461–70. doi: 10.2147/cmar.s161746.
- Nguyen GT, Ngoc Nguyen T, Duc Vu T, Van Nguyen N, Nguyen K. Nonanemic extramedullary hematopoiesis in the posterior mediastinum. Asian Cardiovasc Thorac Ann 2019; 27(2):135-7. doi: 10.1177/0218492318818966.
- Stanchina M, Rosenbaum E, Pronko AJ, Liu Y, Lewis N, Yabe M, et al. Extramedullary hematopoiesis of the renal pelvis in a patient with myelofibrosis. J Oncol Pract 2019; 15(8): 458-9. doi: 10.1200/jop.19.00041.
- Galperin-Aizenberg M, Volchek Y, Even Sapir E, Vasserman M, Maizlin ZV, Cohenpour M, et al. Renal extramedullary haematopoiesis mimicking renal lymphoma on computed tomography. Clin Radiol 2006; 61(10):896-8. doi: 10.1016/j. crad.2006.05.013.
- Roberts AS, Shetty AS, Mellnick VM, Pickhardt PJ, Bhalla S, Menias CO. Extramedullary haematopoiesis: Radiological imaging features. Clin Radiol 2016; 71(9):807-14. doi: 10.1016/j.crad.2016.05.014.
- Mosley C, Jacene HA, Holz A, Grand DJ, Wahl RL. Extramedullary hematopoiesis on F-18 FDG PET/CT in a patient with metastatic colon carcinoma. Clin Nucl Med 2007; 32(11):878-0. doi: 10.1097/rlu.0b013e318156bc84.
- Ahad Aziz Qureshi PA, Razi M, Rehman A, Hassan A. Hodgkin lymphoma with co-existing extramedullary haematopoiesis in a Thalasaemia Major patient: Killing two birds with one stone using PET-CT. J Pak Med Assoc 2019; 69(7):1059. PMID: 31983750.
- Gupta R, Seith A, Guglani B. Renal hilar extramedullary hematopoiesis. Presenting as incidental unilateral renal hilar mass in adolescent male: A case report. Int Urol Nephrol 2009; 41(1):19-21. doi: 10.1007/s11255-008- 9398-8.
- Westphalen A, Yeh B, Qayyum A, Hari A, Coakley FV. Differential diagnosis of perinephric masses on CT and MRI. Am J Roentgenol 2004; 183(6):1697-702. doi: 10.2214/ajr. 183.6.01831697.
- Imai K, Aoi T, Kitai H, Endo N, Fujino M, Ichida S. A case of perirenal extramedullary hematopoiesis in a patient with primary myelofibrosis. CEN Case Rep 2017; 6(2):194‐9. doi: 10.1007/s13730-017-0274-1.
- Ahmad MN, Uddin N, Muzaffar S, Adil SN, Tasneem Z. Extradural extramedullary hematopoiesis: A rare MRI diagnosis with atypical features. J Pak Med Assoc 2004; 54(4):221-3. PMID: 15242004.