A Rare Case of Female Bladder Outlet Obstruction: Severe Introital Stenosis
By Muhammed Fatih Simsekoglu, Oktay Ozman, Mehmet Hamza Gultekin, Bulent CetinelAffiliations
doi: 10.29271/jcpsp.2022.08.S130ABSTRACT
Herein, we report a rare case of severe introital stenosis in a 22-year female who presented with obstructive voiding symptoms and inability to have sexual intercourse. Introital stenosis had been caused by the emergency primary closure after major vulvoperineal trauma 15 years ago. To our knowledge, this is the first case report in the literature that describes a very long time from primary closure to dilation and reconstruction. A detailed systematic evaluation and pelvic examination were performed. The dilation procedure was performed and the patient was closely followed up. Reconstructive surgery, which involved the removal of the granulation tissue and approximation of healthy vaginal mucosal edges in several sessions, was performed after the initial dilation procedure. Follow-up was performed with the clinical assessment of the symptoms, physical examination, and uroflowmetry. Our technique was effective and did not lead to any complications. The sexual dysfunction and voiding complaints of the patient completely resolved within a post-operative period of 11 months.
Key Words: Introital stenosis, Bladder outlet obstruction, Dilation, Female, Reconstruction.
INTRODUCTION
Introital stenosis is a rare urological entity caused by the congenital and acquired conditions. It may develop due to the various factors such as vulvar lichen sclerosis, radiotherapy, vulvoperineal trauma, caustic vaginal burns, birth injury, vulvoperineal surgery, and vaginal atresia (Mayer-Rokitansky-Kuster-Hauser syndrome).1,2 Pelvic and vulvoperineal traumas lead to the high morbidity and mortality rates due to their severity and other anatomical factors. These injuries are frequently accompanied by the additional organ damage.3 Primary closure is suggested in the emergency cases presenting with the multiple traumas and hemodynamic instability.4,5
Herein, we report a rare case of introital stenosis in a 22-year female who presented with obstructive voiding symptoms and inability to have sexual intercourse. It was determined that introital stenosis had been caused by the emergency primary closure after major vulvoperineal trauma in her childhood. To our knowledge, this is the first case report in the literature describing a very long time from primary closure to dilation and reconstruction. This report may help to increase awareness of introital stenosis as a late complication of vulvoperineal trauma primary repair.
CASE REPORT
A 22-year married woman presented with the obstructive voiding symptoms and inability to have sexual intercourse with her husband. Although her menstruation cycle was regular, menstrual bleeding was painful and in the form of dribbling. She had also been experiencing severe obstructive voiding symptoms for many years since the vulvoperineal trauma she incurred in a non-vehicle traffic accident, when she was seven years old. Her medical history revealed that the emergency primary closure had been performed to treat vulvoperineal trauma with the multiple bone fractures caused by the accident. Although she began to have disturbing voiding and menstrual symptoms after this event, she was not refered to any health care unit due to the socio-economic factors before her presentation to our department. She had no medication use or known allergies. Urinary ultrasonography revealed bilateral minimal hydronephrosis with the normal bladder morphology. Her blood creatinine level was normal, and urine culture was sterile. The pelvic examination revealed a closed introitus with a dense fibrotic tissue (Figure 1a). The uroflowmetric analysis showed that the maximum flow rate was 2.4 ml/sec with a total volume of 168.7 ml, and post-void residual was 25 ml (Figure 1b).
A detailed examination under general anaesthesia revealed a 1 mm hole through which only a stylet could pass. A 0.035-inch guidewire was inserted through this hole (Figure 1c). Dilation was performed using 6 Fr, 8 Fr, 10 Fr, and 12 Fr Amplatz dilators. Then the hole was expanded to 30 Fr using Hegar’s dilators (Figure 1d). The introital area was evaluated using cystoscopy, but the urethral meatus could not be visualised. After the insertion of a suprapubic bladder catheter and filling the bladder up to its capacity, methylene blue was injected through the suprapubic catheter, and a guide wire was inserted through the hole where methylene blue was seen after suprapubic compression. Under the guidance of the guidewire, a 16 Fr urethral catheter was placed into the bladder. The introital hole was dilated upto 30 mm with Hegar's dilators, three times a week for three weeks. At the end of the third week, the surgical removal of granulation tissue and the approximation of healthy vaginal mucosal edges were performed in three separate sessions (Figure 2a). During this time, wound dressing was performed with potent topical steroid covered materials (betamethasone valerate) after every two days (Figure 2b).
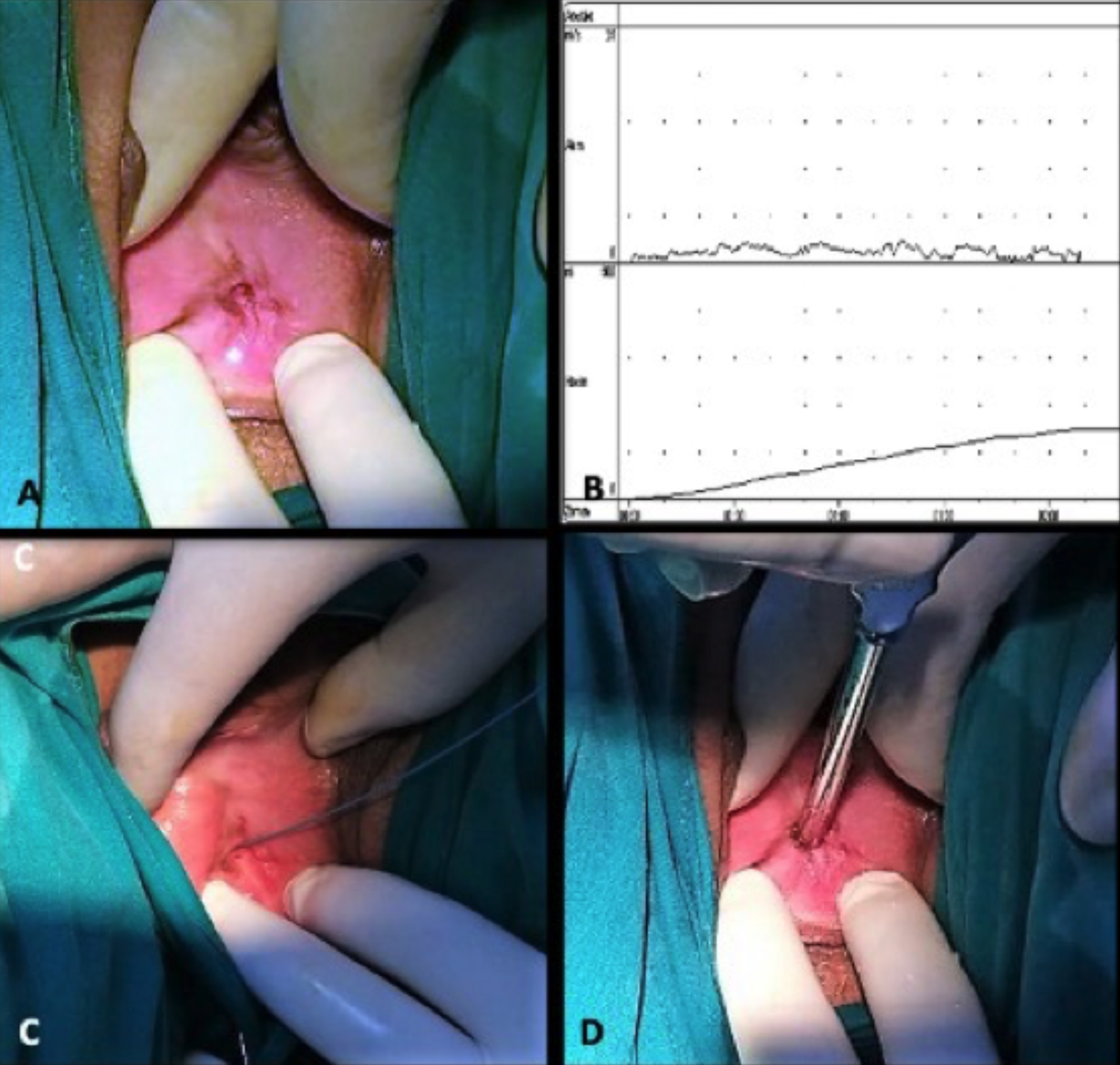 Figure 1: (a) Preoperative physical examination. (b) preoperative uroflo-wmetry, (c) insertion of guidewire, and (d) dilatation with Hegar’s dilators.
Figure 1: (a) Preoperative physical examination. (b) preoperative uroflo-wmetry, (c) insertion of guidewire, and (d) dilatation with Hegar’s dilators.
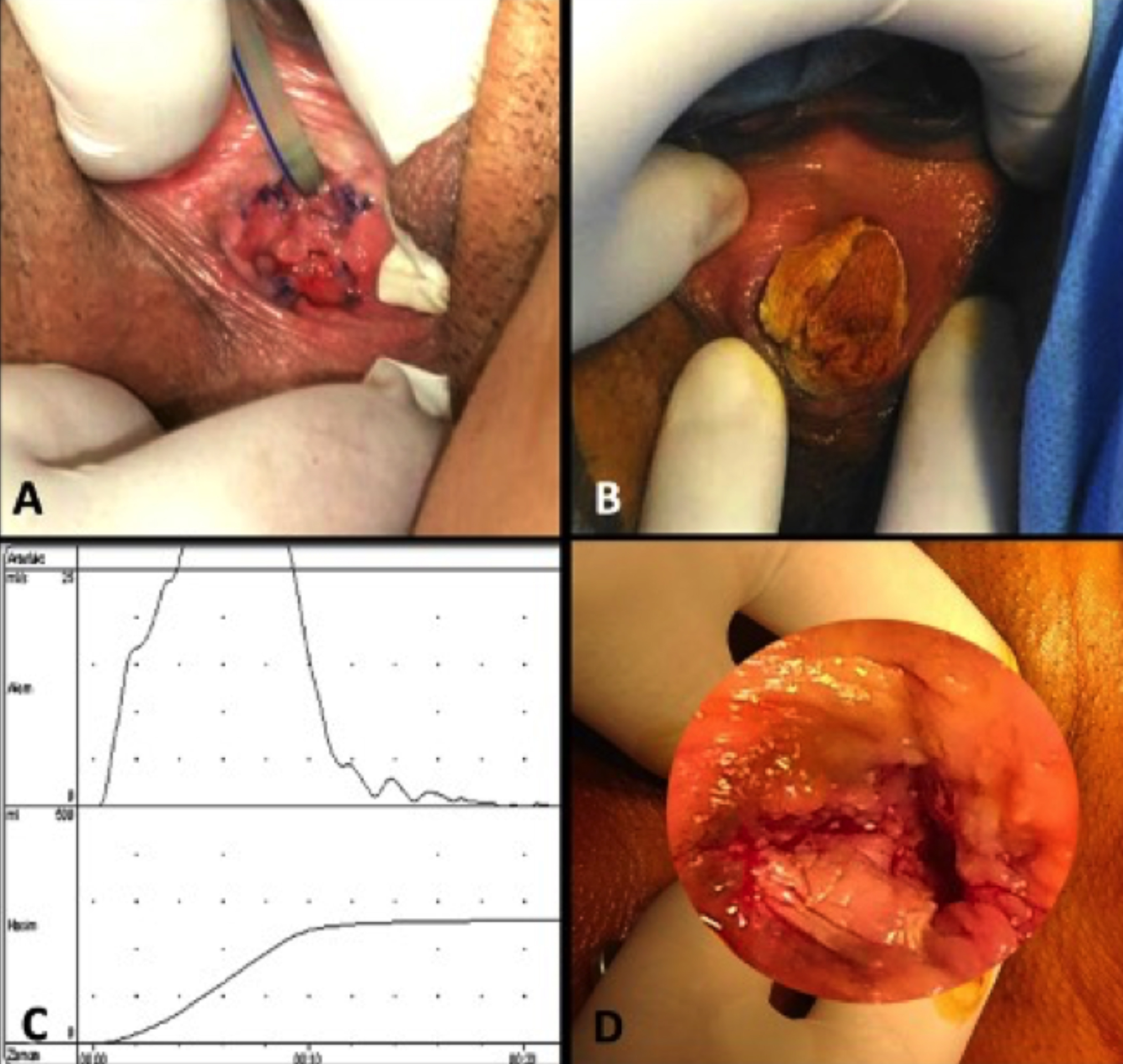 Figure 2: (a) Appearance of the introitus after reconstructive intervention, (b) wound dressing with steroid covered materials, (c) postoperative uroflowmetry, and (d) postoperative appearance of the introitus in the sixth month.
Figure 2: (a) Appearance of the introitus after reconstructive intervention, (b) wound dressing with steroid covered materials, (c) postoperative uroflowmetry, and (d) postoperative appearance of the introitus in the sixth month.
The postoperative course was uneventful, and the patient was discharged on the second post-operative day after the last intervention. The urethral catheter was removed in the second postoperative week following the last intervention. The postoperative uroflowmetry revealed completely normal values. The maximum flow rate was 32.5 ml/sec with a total volume of 248.7 ml, and postvoid residual was 10 ml (Figure 2c). The patient was advised to have a regular sexual intercourse to prevent recurrent stricture. She reported that she was able to have normal sexual intercourse with her partner. Six months after surgery, the anatomical, cosmetic, and functional results were excellent with an adequate introital opening (Figure 2d). The patient gave birth to a girl through caesarean section in the 10th month. She was not able to attend follow-up sessions due to her pregnancy. In the 11th postoperative month, a phone interview was conducted which revealed that she continued to have a healthy sexual life, and she was completely satisfied with the results.
DISCUSSION
We report a rare case of severe introital stenosis caused by emergency primary closure after major vulvoperineal trauma. This is the first case in the literature in terms of the long period from primary closure to dilation and reconstruction. Primary closure of a vulvoperineal defect frequently causes disappointing cosmetic results that comprise sexual and urinary functions.6 In this regard, the patients undergoing primary closure should carefully and strongly be advised to regularly attend follow-up for the detection of any possible formation of introital stenosis. This condition has been reported in the literature primarily in the form of the case reports.6 The acquired vaginal stenosis is common in Africa due to the caustic vaginal burns, birth injury, and vulvar lichen sclerosis, and it is also a complication of vesicovaginal fistula repair. 7 In the developed countries, it has been reported to be associated with coital or non-coital trauma and radiotherapy.8 However, the aetiology of introital stenosis in our patient was inappropriate primary surgical closure to treat vulvoperineal trauma which, to our knowledge, has not been previously reported. The surgeons, who treat vulvoperineal trauma with primary surgical closure in emergency units, should be aware of the possible late-onset complication of introital stenosis and inform the patient or his/her caregivers by emphasising the importance of careful and regular follow-up in the prevention and treatment of this complication.
To date, only a few methods have been described for the surgical treatment of introital stenosis.6,9-11 The choice for treatment depends on the characteristics of wound damage, patient’s condition, and surgical experience. Skin grafts, which were used in the past, have been replaced with flap repair mainly due to the high risk of infection and poor cosmetic results after skin graft repair.12 Additionally, some perineoplasty techniques have been described in the literature to treat this challenging situation with successful long-term surgical results, but they also involve a serious risk of morbidity.9 After perineoplasty surgery, improvement in sexual function has been reported in 86% of the patients with introital stenosis.9
Minimally invasive reconstructive techniques should be considered in the patients without significant vulvoperineal tissue loss before invasive major reconstructive surgery. However, it should be taken into account that these techniques have high re-stenosis rates.13 In a retrospective study involving 21 patients with acquired vaginal stenosis, the need for surgical reconstruction was reported in 95.2% of the patients after the dilation procedures.13 In the same study, the rate of healthy coitus was 47.6%. To minimise re-stenosis events, patients should be included in an appropriate follow-up and dilation program as we did in our case. In this respect, patient compliance and socio-economic status should also be considered, and treatment decisions should be made accordingly. Major reconstructive surgery should be performed in the cases of recurrent stenosis.
A pelvic examination and detailed systematic evaluation, including urinary ultrasonography and blood creatinine level, are recommended in patients with introital stenosis.6 Although the literature contains no data regarding the upper urinary tract deterioration in patients with introital stenosis, the evaluation of the renal function of these patients is necessary since introital stenosis may cause severe bladder outlet obstruction as in the present case in which urinary ultrasonography revealed bilateral minimal hydro-nephrosis without any deterioration in renal function. After the initial clinical evaluation, we discussed optimal surgical options with a multi-disciplinary approach. After the initial dilation procedure, a reconstructive surgery, including the removal of granulation tissue and approximation of healthy vaginal mucosal edges in several sessions, was made. Postoperative regular sexual intercourse resulting in natural dilation was the advantage of this case for the prevention of recurrent stricture. Dilation and minimal reconstructive surgery, as described in this case, are a feasible options before resorting to major reconstructive surgery in the selected patients.
PATIENT’S CONSENT:
Informed consent was obtained from the patient included in the study.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
MFS: Conception, performance of work, and writing the article.
OO: Performance of work, writing the article, and interpretation of data.
MHG: Interpretation of data and writing the article.
BC: Conception.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Krapf JM, Mitchell L, Holton MA, Goldstein AT. Vulvar lichen sclerosis: Current perspectives. Int J Womens Health 2020; 12:11-20. doi: 10.2147/IJWH.S191200.
- Avino A, Raducu L, Tulin A, Gheoca-Mutu DE, Balcangiu-Stroescu AE, Marina CN, et al. Vaginal reconstruction in patients with mayer–rokitansky–küster–hauser syndrome — one centre experience. Medicina 2020; 56(7):327. doi: 10.3390/medicina56070327.
- Velazquez N, Fantus RJ, Fantu RJ, Kingsley S, Bjurlin MA. Blunt trauma pelvic fracture-associated genitourinary and concomitant lower gastrointestinal injury: Incidence, morbidity, and mortality. World J Urol 2019; 38(1):231-8. doi: 10.1007/s00345-019-02725-7.
- Agrawal A, Kumar P, Singhal R, Singh V, Bhagol A. Animal bite injuries in children: Review of literature and case series. Int J Clin Pediatr Dent 2017; 10(1):67-72. doi: 10.5005/jp-journals-10005-1410.
- Lopez HN, Focseneanu MA, Merritt DF. Genital injuries acute evaluation and management. Best Pract Res Clin Obstet Gynaecol 2018; 48:28-39. doi: 10.1016/j.bpobgyn. 2017.09.009.
- Budaa A, Confalonierib PL, Rovatib LCV. Tunneled modified lotus petal flap for surgical reconstruction of severe introital stenosis after radical vulvectomy. Int J Surg Case Rep 2012; 3(7):299-301. doi: 10.1016/j.ijscr.2012.03.024.
- Arowojolu AO, Okunlola MA, Adekunle AO, Ilesanmi AO. Three decades of acquired gynaetresia in Ibadan: Clin presentation and management. J Obstet Gynaecol 2001; 21(4):375-8. doi: 10.1080/01443610120059923.
- Damast S, Jeffery DD, Son CH, Hasan Y, Carter J, Lindau ST, et al. Literature review of vaginal stenosis and dilator use in radiation oncology. Pract Radiat Oncol 2019; 9(6): 479-91. doi: 10.1016/j.prro.2019.07.001.
- Rouzier R, Haddad B, Deyrolle C, Pelisse M, Barracco M, Paniel BJ. Perineoplasty for the treatment of introital stenosis related to vulvar lichen sclerosus. Am J Obstet Gynecol 2002; 186(1):49-52. doi: 10.1067/mob.2002. 119186.
- Pusic AL, Mehrara BJ. Vaginal reconstruction: An algorithm approach to defect classification and flap reconstruction. J Surg Oncol 2006; 94(6):515-21. doi: 10.1002/jso.20489.
- Ogliari KCM, Rios SS, Chen AC, Chen JR, Resende CN, Junior EA. An alternative approach to vaginal dilation in patients with Meyer-Rokitanski-Kuster-Hauser syndrome: Two case reports. Gynecol Endocrinol 2020; 36(8):746-8. doi: 10.1080/09513590.2020.1719061.
- Reid R. Local and distant skin flaps in the reconstruction of vulvar deformities. Am J Obstet Gynecol 1997; 177(6): 1372-83. doi: 10.1016/S0002-9378(97)70078-4.
- Se´ni K, Horo AG, Koffi A, Aka KE, Fomba M, Kone M. Acquired caustic vagina stenosis: Surgical outcomes of 21 cases. Gynecol Obstet Fertil 2016; 44(3):141-5. doi: 10.1016/j.gyobfe.2016.02.004.