Neurological Sequelae in Youngest Adult Behcet’s Disease Patient on Infliximab
By Mamoona Sultan1, Adeena Khan2, Syed Shahid Habib3, Muhammad Hayat4Affiliations
doi: 10.29271/jcpsp.2020.07.762ABSTRACT
Neuro-Behcet’s disease is a rare neurological complication of Behcet’s disease presenting between second and fourth decades of life. The etiology of Behcet’s disease is still unknown but genetic predisposition has been described to play a role. The disease is reported more in males than females. Neurological involvement could cause brain parenchymal, vascular or meningeal changes with other distinct systemic symptoms, which may include orogenital ulcers, uveitis and skin lesions. Parenchymal neuro-Behcet’s disease has a poor prognosis. MRI aids in diagnosing and differentiating it from other entities. Treatment includes anti-inflammatory drugs and immunotherapeutics. Our case is the youngest adult reported so far and is an unusual presentation of neuro-Behcet’s disease, as the patient was already in remission and on infliximab infusion.
Key Words: Neuro-Behcet’s, MRI, Infliximab.
INTRODUCTION
Behcet’s disease is a rare multisystem multivessel autoimmune relapsing remitting disorder of unknown etiology, reported most frequently in Turkey with prevalence of 20 - 602/ 100,000.1,2 Neuro-Behcet’s is also rare but serious complication of Behcet's disease seen in 5 to 50% of patients.3 Behcet’s, a Turkish dermatologist, described its triad of recurrent symptoms in 1937 for the first time, i.e., oral ulcers, genital ulcer and uveitis.2,4 The term “Neuro-Behçet’s syndrome” was first presented by Cavara and D’Ermo in 1954.5 Neurological complications are commonly due to brain parenchymal involvement.2
After the first reported case by Knapp in 1941,6 many cases have been reported in the past; but our patient is the youngest adult reported so far in literature, who developed Neuro-Behcet’s symptoms while on infliximab infusion.
CASE REPORT
An 18-year male was diagnosed 8 years ago with Behcet’s disease due to presentation with recurrent oral and genital ulcers.
Patient was followed up in King Saud University Medical City for Behcet’s uveitis and was on infliximab infusion for the past 6 years after failed response of uveitis to corticosteroids and mycophenolate mofetil as an initial immunosuppressant therapy.
He presented in ophthalmology emergency with severe headache and double vision and was referred to neurology. On 3rd day of admission, he developed right-sided hemiparesis. Examination findings were ptosis of left eye with limited adduction and elevation, sluggish pupil response and left-sided homonymous hemianopia. Power was reduced to 4/5 in right upper and lower limbs.
Blood investigations were grossly normal but cerebrospinal fluid (CSF) was positive for inflammatory changes, i.e. protein level of 0.930 g/L; white blood cells, 50/mm3; polymorphonuclear cells, 15%; lymphocytes, 85%; and glucose normal. CSF culture and herpes simplex virus 1 and 2 DNA were negative. Nerve conduction studies showed no abnormality.
Contrast enhanced MRI brain showed diffuse hyperintense T2/FLAIR signals involving the midbrain including cerebral peduncles, pons, bilateral thalami, middle cerebellar peduncles and bilateral internal capsules (Figure 1). Internal capsule and thalami involvement were explaining right hemiparesis and left homonymous hemianopia, while pons involvement was attributing to the third nerve palsy. MR angiogram was normal. Based on the clinical symptoms, CSF and radiological findings, clinical diagnosis of parenchymal Neuro-Behcet’s was made.
Table I: Types of neuro-behcet’s and their clinical presentations.|
|
Area / type of involvement with their clinical symptoms |
|||
|
Types (%) |
Cerebral hemisphere |
Spinal cord |
Cerebellum |
Less common |
|
Parenchymal (77% TO 87%) |
Hemiparesis (uncrossed) Speech difficulties visual field defects |
Spastic paraparesis flaccid paraparesis sphincter disturbances |
Vertigo nystagmus ataxia |
Stroke epilepsy cranial nerve involvement |
|
|
Venous: Dural venous sinus thrombosis |
Arterial: Intracranial HTN |
Intracranial aneurysm |
|
|
Non parenchymal (vascular) (13% to 23%) |
Severe headache Ophthalmoplegia |
Headache vision loss papilledema |
Severe headache in case of dissecting aneurysm |
|
|
|
Guillain-barre’syndrome |
Sensorimotor neuropathy |
Autonomic neuropathy |
|
|
Peripheral nervous system (0.8%) |
Ascending weakness areflexia, decreased vital capacity |
Loss of pain, touch and temperature weak / flaccid muscles |
Hypothermia, postural hypotension |
|
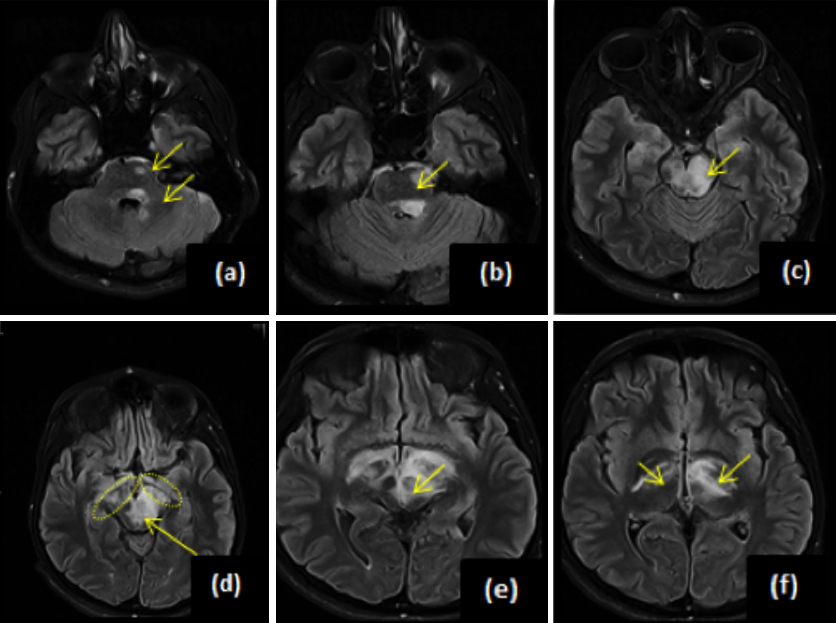 Figure 1: MRI brain (axial, flair sequence showing hyperintensities in pons, left middle cerebellar penduncle (a,b,c), midbrain including cerebral peduncles (d,e), bilateral thalami and bilateral internal capsules (f).
Figure 1: MRI brain (axial, flair sequence showing hyperintensities in pons, left middle cerebellar penduncle (a,b,c), midbrain including cerebral peduncles (d,e), bilateral thalami and bilateral internal capsules (f).
The patient was given high dose corticosteroids and infliximab infusion. Symptomatically, the patient started improving on follow up with near complete resolution of symptoms.
DISCUSSION
Neuro-Behcet’s disease is a rare and morbid secondary complication of the Behcet’s disease presenting few years after the onset of Behcet’s disease. It has been found more in males than in females with male to female ratio of 2.8:1 and is more prevalent in Middle East and Far East regions. The common age of presentation is between second to fourth decade.2,7,8 To best of our knowledge, the youngest adult age reported so far in previous studies is 25 years;2,9 whereas, our patient presented at 18 years.
Though the exact etiology of Behcet’s disease, and now neuro-Behcet’s disease is unknown but genetic predisposition to HLA B51 and heat shock proteins have been suggested to play some role, which were not tested in our patient.2,10 Its pathogenesis has been described as upregulation of proinflammatory tumor necrosis factor (TNF), which, in turn, leads to inflammatory reaction; and heat shock proteins are autoantigens that can induce inflammatory reaction in individuals who are genetically predisposed to HLA-B51.1,3,11
The clinical manifestations of neuro-Behcet’s disease could be related to parenchymal and non-parenchymal involvement (Table I).3,12
Parenchymal neuro-Behcet’s disease is the commonest presentation of neuro-Behcet’s (77% to 87%) as seen in our patient as unilateral hemiparesis. MRI is the investigation of choice to diagnose and differentiate neuro-Behcet’s from other mimics. MRI is also considered as an additional help for monitoring the course of neurologic deficits. The parenchymal signal changes depict edema and demyelination in acute phase and gliosis, and atrophy in chronic. These changes are most common in brainstem, especially around the cerebral peduncles and pons, followed by thalamus, basal ganglia and cerebral hemispheres.8,13 Our patient’s MRI findings were also in agreement with previous studies.
Despite having previously described diagnostic criteria for neuro-Behcet’s disease, there is no specific test to diagnose it; and management is all based on clinical manifestations with laboratory and MRI findings as supporting tools.1,2 MRI and CSF analysis play an important role to support the clinical diagnosis. CSF is altered in 70-80% of patients with brain parenchymal involvement.2 It shows inflammatory changes including raised proteins and cells count with normal or reduced glucose.1,2 Similar inflammatory CSF changes were seen in our patient as well.
Among non-parenchymal changes, dural venous sinus thrombosis is the commonest and seen in 5-25 % of cases, but our patient’s MR angiogram was normal. Other rare findings could be aseptic meningitis, cerebral arterial aneurysm, occlusion and dissection.13
Peripheral nervous system involvement is the rarest complication but subclinical nerve conduction abnormalities can be seen. In this patient, nerve conduction studies were normal.
Since neuro-Behcet’s disease is a complication of Behcet’s disease, which stands at the juncture of autoinflammatory and autoimmune processes; hence, the treatment includes anti-inflammatory agents (e.g. NSAIDS, colchicine and cortico-steroids), and immunotherapeutics, which are further classified as immunosuppressants (e.g. cyclosporine, myco-phenolate, mofetil and azathioprine) and immunomodulators (e.g. interferon alpha and TNF alpha). The role of anticoagulants is controversial in neuro-Behcet’s disease.12 Our patient developed neurological symptoms while he was in remission and on immunomodulator (i.e. infliximab), which had never been reported before.
Parenchymal neuro-Behcet’s disease is associated with poor prognosis and about 50% of them present with severe disabilities within 10 years of diagnosis. Other poor prognostic markers are disseminated neurological involvement, spinal symptoms, more than 2 attacks in a year and inflammatory CSF changes at the time of presentation.1,2,12
Early recognition and management of neuro-Behcet’s disease may help in preventing grave disabilities and irreversible neurological damage. We could expect it in an adult even before second decade.
We had our limitations in conducting visual evoked potentials for visual field defects due to unavailability in our hospital.
PATIENT'S CONSENT:
Patient was informed about the publication. The images and information shared in the manuscript are anonymised.
CONFLICT OF INTEREST:
Authors have no conflict of interest to be declared.
AUTHORS' CONTRIBUTION:
MS: Principal investigator, reported idea and design, literature review and manuscript writing.
AK: Writing of manuscript, literature review, report review and final review of the manuscript.
SSH: Report writing assistance, literature review and final approval.
MH: Report review and assistance in final review.
REFERENCES
- Kalra S, Silman A, Akman-Demir G, Bohlega S, Borhani-Haghighi A, Constantinescu C, et al. Diagnosis and management of neuro-Behçet's disease: International consensus recommendations. J Neurol 2014; 261(9): 1662-76.
- Al-Araji A, Kidd D. Neuro-Behçet's disease: Epidemiology, clinical characteristics, and management. The Lancet Neurol 2009; 8(2):192-204.
- Venna N, Siva A, Miller J. Neuro-Behcet's disease and autoinflammatory disorders. Semin Neurol 2014; 34(04): 437-43.
- Behcet H. Uber rezideivierende, aphtose, durch ein virus veursachte Geschure am Mund, Am Auge und an den Genitalien. Dermatol Wachenschr 1937; 105:1152-57.
- Cavara V, D’Ermo E. A case of Neuro-Behcet’s syndrome. Acta XVII Concili Ophtalmologici 1954; 3:1489.
- Knapp P. BeitragzurSymptomatologie und Therapie der rezidiverendenHypopyoniritis und der begleitendena-pthösenSchleimhauterkrankungen. Shweiz Med Wochenschr 1941; 71: 1288-90.
- Otsuka Y, Yumoto T, Ihoriya H, Matsumoto N, Sato K, Abe K, et al. Acute agitation as an initial manifestation of neuro-Behçet’s disease. Case Rep Emerg Med 2018; 2018:1-3.
- Mehdipoor G, Davatchi F, Ghoreishian H, Arjmand A. Imaging manifestations of Behcet’s disease: Key considerations and major features. Eur J Radiol 2018; 98: 214-25.
- Fabiani G, Almeida S, Germiniani F, Teive H, Nóvak E, Scola R, et al. Neuro-Behçet’s: Report of three clinically distinct cases. Arquivos de Neuro-Psiquiatria 2001; 59(2A):250-54.
- Sahebari M, Hashemzadeh K, Mahmoudi M, Saremi Z, Mirfeizi Z. Diagnostic yield of heat shock protein 70 (HSP-70) and anti-HSP-70 in Behcet-induced uveitis. Scand J Immunol 2013; 77(6):476-81.
- Gül A. Pathogenesis of Behçet’s disease: Autoinflammatory features and beyond. Semin Immunopathol 2015; 37(4):413-8.
- Dutra L, Povoas O. Neuro-Behcet's disease: A review of neurological manifestations and its treatment. J Vascul 2016; 2(2):112.
- Chae E, Do K, Seo J, Park S, Kang J, Jang Y, et al. Radiologic and clinical findings of Behçet disease: Comprehensive review of multisystemic involvement. Radiographics 2008; 28(5):31.