Morel-Lavallée Lesion in a 35-year Female
By Amir Humza Sohail1, Muhammad Talha Liaquat2, Mohammed Sachal Sohail2, Muhammad Salman Khan3, Hazim Hakmi1Affiliations
doi: 10.29271/jcpsp.2021.03.342ABSTRACT
Morel-Lavallée lesion is a post-traumatic degloving cyst, usually filled with blood, lymph or necrotic tissue, which mostly develops in the area around greater trochanter. Early diagnosis and prompt treatment is essential to prevent further complications, such as compression of surrounding structures. X-rays have limited use and magnetic resonance imaging (MRI) is the modality of choice in diagnosing the lesion. We report a case of a 35-year female presenting with left thigh pain after a fall from motorcycle almost 21/2 years ago. Ultrasound and MRI confirmed the presence of Morel-Lavallée lesion involving the left pelvis and upper thigh. Given the chronicity of lesion and extensive tissue involvement, the patient underwent surgical excision of the lesion with favourable long-term outcomes. In this case report and literature review, we discuss the pathophysiology, clinical presentation, radiological findings and management options for Morel-Lavallée lesion.
Key Words: Morel-Lavallée lesion, Post-traumatic cyst, Degloving Injury, Tangential cyst.
INTRODUCTION
Morel-Lavallée lesion or post-traumatic tangential cyst is a closed degloving injury manifesting as a sequel to blunt trauma.1 A cavity is created as a result of shearing force between subcutaneous tissue and the underlying fascia, followed by filling of this space with necrotic fat, blood and lymph due to damaged blood and lymphatic vessels.2 Chocolate-colour fluid with interspersed cholesterol crystals is mostly found in such cavities.3 The presentation of Morel-Lavallée lesion is variable depending on the area involved and the extent of the lesion.3 To prevent complications, such as abscess formation, pseudo-capsule formation and cosmetic deformities, timely diagnosis and proper management is crucial.3 Physicians should be cognizant of the possibility of this condition in blunt trauma patients.
CASE REPORT
A 35-year female presented to the clinic with gradual pain and swelling in the upper part of left leg after a fall from motorcycle almost 21/2 years ago. There were no associated symptoms. Past medical and surgical history was unremarkable as were review of systems and systemic examinations.
An ultrasound of the swelling was performed, which showed an elongated anechoic area with thick internal septations, measuring approximately 20.3 x 8.4 cm, starting from the area just below the left sacroiliac joint and extending along the lateral part of gluteus maximus up to middle of the thigh laterally (Figure 1). Mild vascularity was seen within the septations.
After the ultrasound, magnetic resonance imaging (MRI) pelvis was performed, which showed a well-encapsulated, lobulated abnormal intensity lesion, measuring 9.2 x 11.1 x 0.2 cm, in the left side of the pelvis and upper thigh in the subcutaneous soft tissues superficial to the underlying muscles, abutting the left gluteus medius, maximus and tensor fascial lata (Figure 2). Posteromedially, a loculus in the gluteus medius muscle was present, which had its component lying posterior to the left sacroiliac joint while superiorly it also extended and abutted the erector spinae muscle up to L4-L5 level (Figures 2 to 4). Within this lesion, there were multiple internal septations and fluid levels. It showed variable signal intensities, appearing predominantly hyperintense on T2-weighted images (Figures 2 and 3), isointense to hypointense on T1-weighted images (Figure 4), and did not show fat suppression (Figure 5). No post-contrast enhancement was identified within the lesion (Figure 6). Bones and flow voids were normal while there was no infiltration into underlying muscle. A bilobed fluid signal intensity cyst, measuring 4.4 x 4.0 cm, was identified in the pelvis, which was likely present within the cul-de-sac. Given the chronicity of lesion and the extensive involvement of tissues, patient underwent surgical intervention with complete excision of the lesion. There was no recurrence reported at a 12-month follow-up.
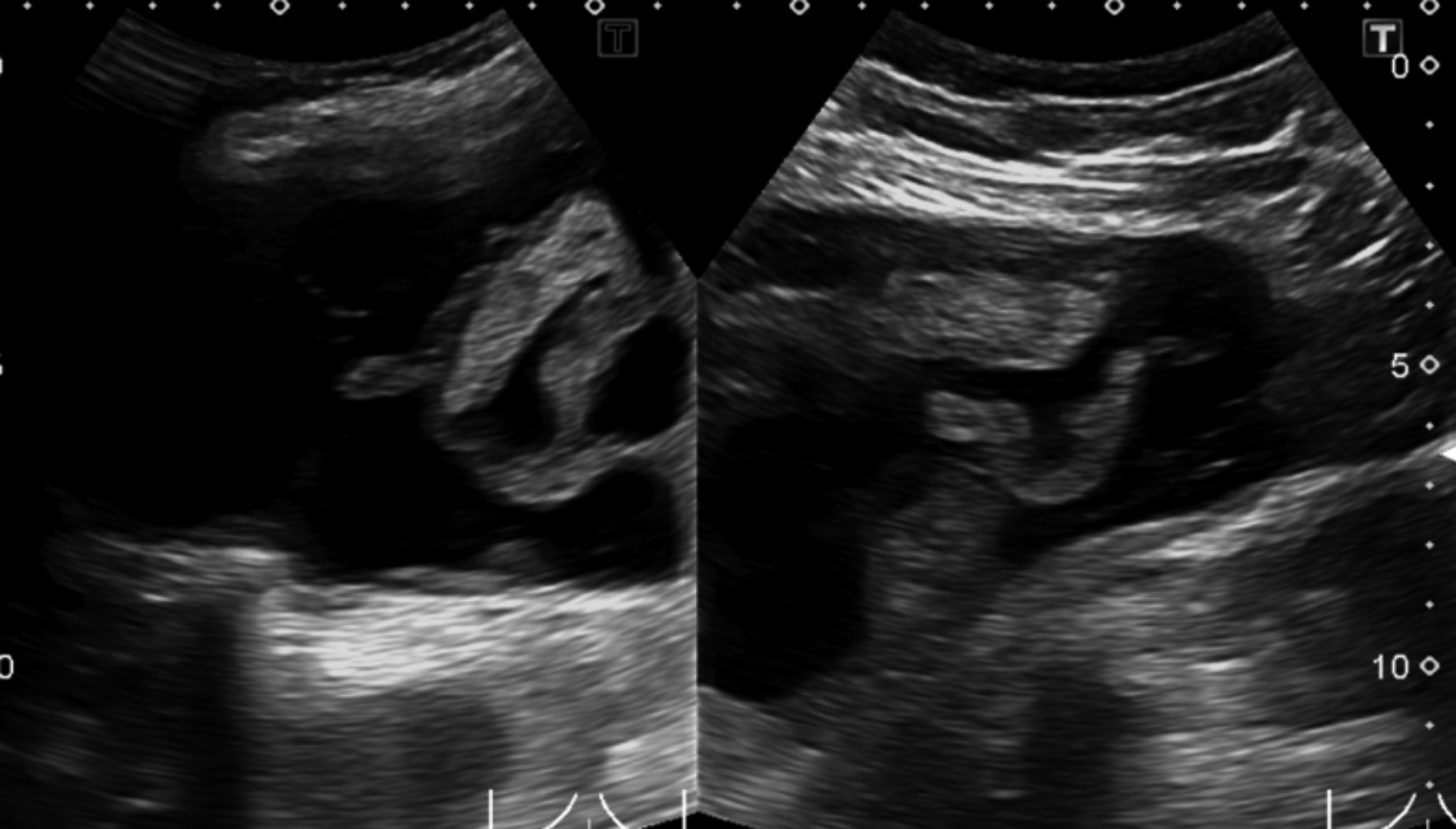 Figure 1: Ultrasound image showing an elongated anechoic area with thick internal septations and mild internal vascularity starting just below the left sacroiliac joint and extending along the lateral part of the gluteus maximus upto the mid-thigh laterally.
Figure 1: Ultrasound image showing an elongated anechoic area with thick internal septations and mild internal vascularity starting just below the left sacroiliac joint and extending along the lateral part of the gluteus maximus upto the mid-thigh laterally.
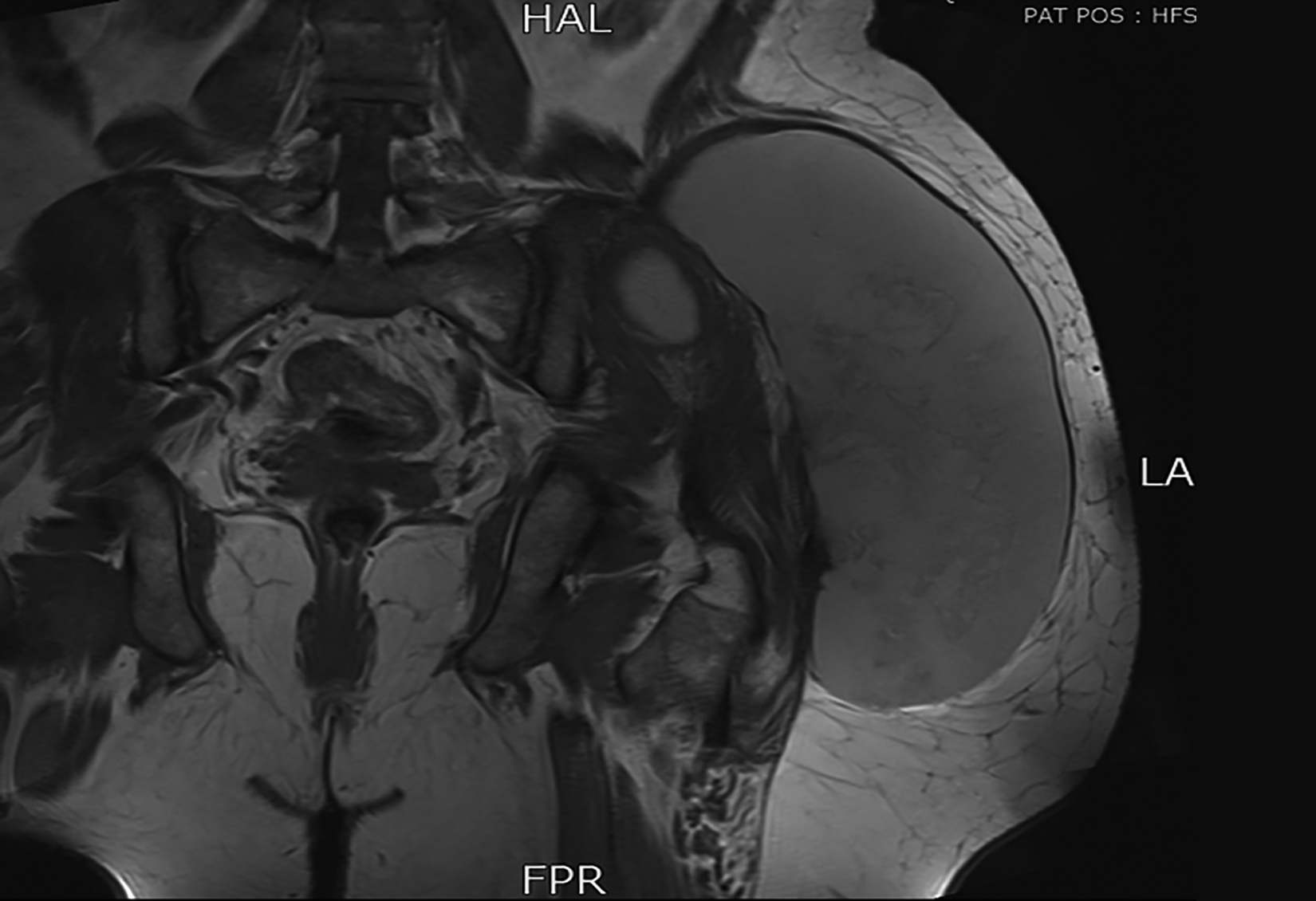 Figure 2: MRI T2 coronal shows well encapsulated, lobulated predominantly hyperintense lesion in the left side of pelvis and upper thigh in the subcutaneous soft tissues superficial to the underlying muscles. It is majorly abutting the left gluteus medius, maximus, and tensor fascial lata. Posteromedially, it has a loculus in the gluteus medius muscle; and a component, which is lying posterior to the left sacroiliac joint. Multiple internal septations within this lesion are also seen.
Figure 2: MRI T2 coronal shows well encapsulated, lobulated predominantly hyperintense lesion in the left side of pelvis and upper thigh in the subcutaneous soft tissues superficial to the underlying muscles. It is majorly abutting the left gluteus medius, maximus, and tensor fascial lata. Posteromedially, it has a loculus in the gluteus medius muscle; and a component, which is lying posterior to the left sacroiliac joint. Multiple internal septations within this lesion are also seen.
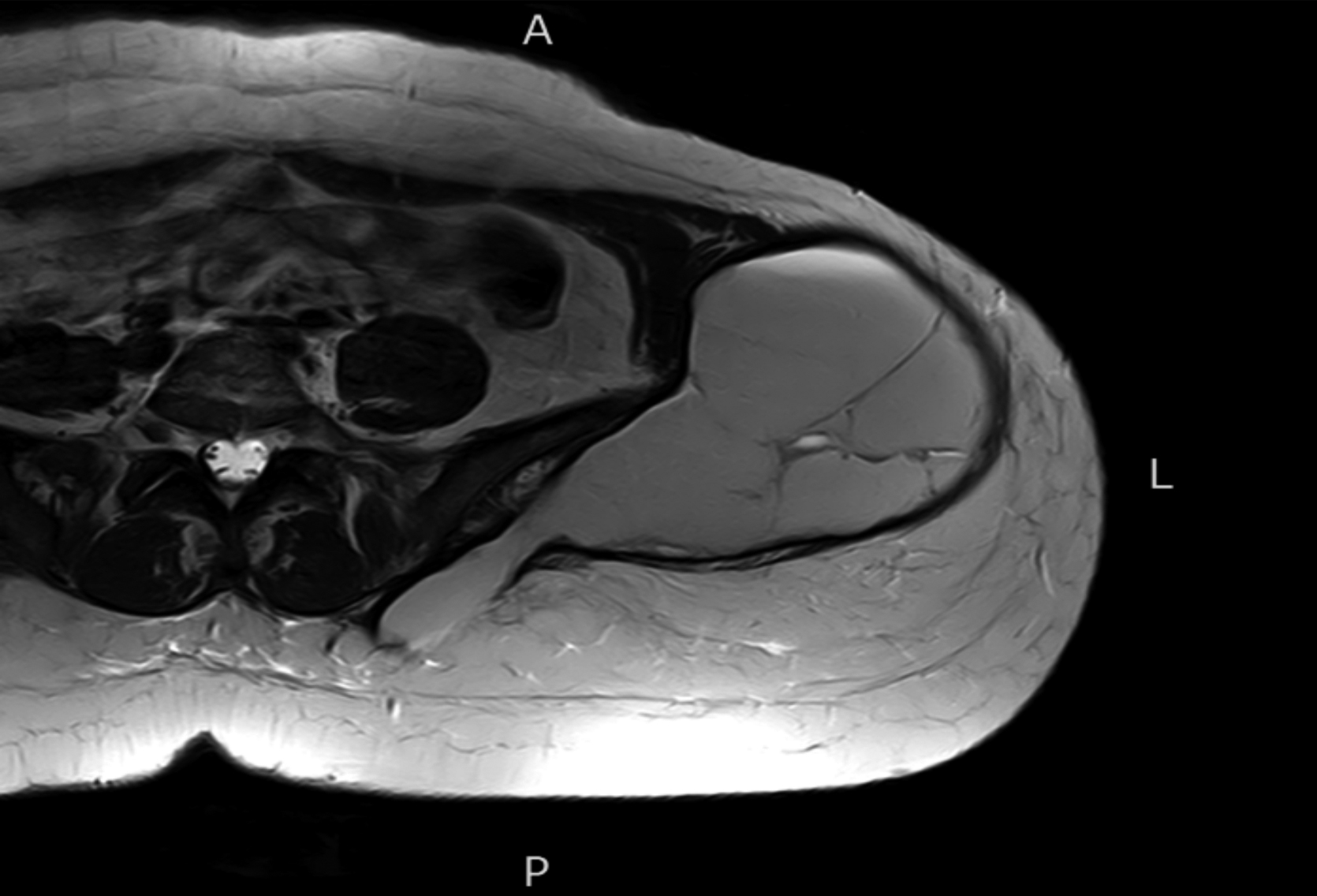 Figure 3: MRI T2 axial shows well encapsulated, lobulated predominantly hyperintense lesion in the left side of pelvis and upper thigh in the subcutaneous soft tissues superficial to the underlying muscles. Multiple internal septations within this lesion.
Figure 3: MRI T2 axial shows well encapsulated, lobulated predominantly hyperintense lesion in the left side of pelvis and upper thigh in the subcutaneous soft tissues superficial to the underlying muscles. Multiple internal septations within this lesion.
DISCUSSION
The French physician Maurice Morel-Lavallée was the first to describe this lesion in 1853.4 Trauma is the most common cause of Morel-Lavallée lesion (our patient had a history of trauma) but systemic diseases such as erythema nodosum, necrobiosis lipoidica, sclerosing panniculitis, and nodular vasculitis can also produce this lesion.4
 Figure 4: MRI T1 axial shows well encapsulated, lobulated iso to low intensity lesion in the left side of pelvis and upper thigh in the subcutaneous soft tissues superficial to the underlying muscles. Multiple internal septations within this lesion.
Figure 4: MRI T1 axial shows well encapsulated, lobulated iso to low intensity lesion in the left side of pelvis and upper thigh in the subcutaneous soft tissues superficial to the underlying muscles. Multiple internal septations within this lesion.
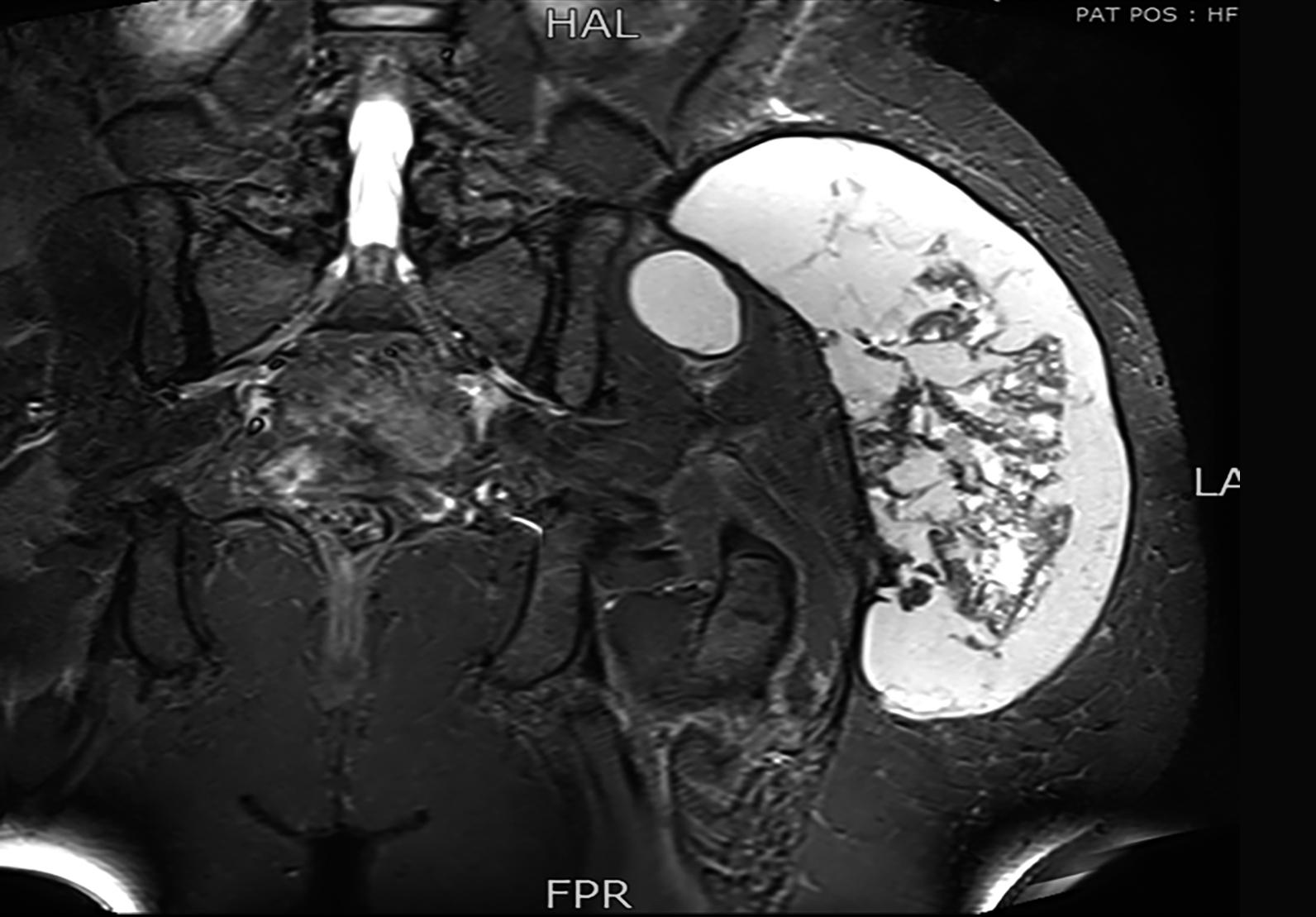 Figure 5: MRI coronal stir shows no fat suppression.
Figure 5: MRI coronal stir shows no fat suppression.
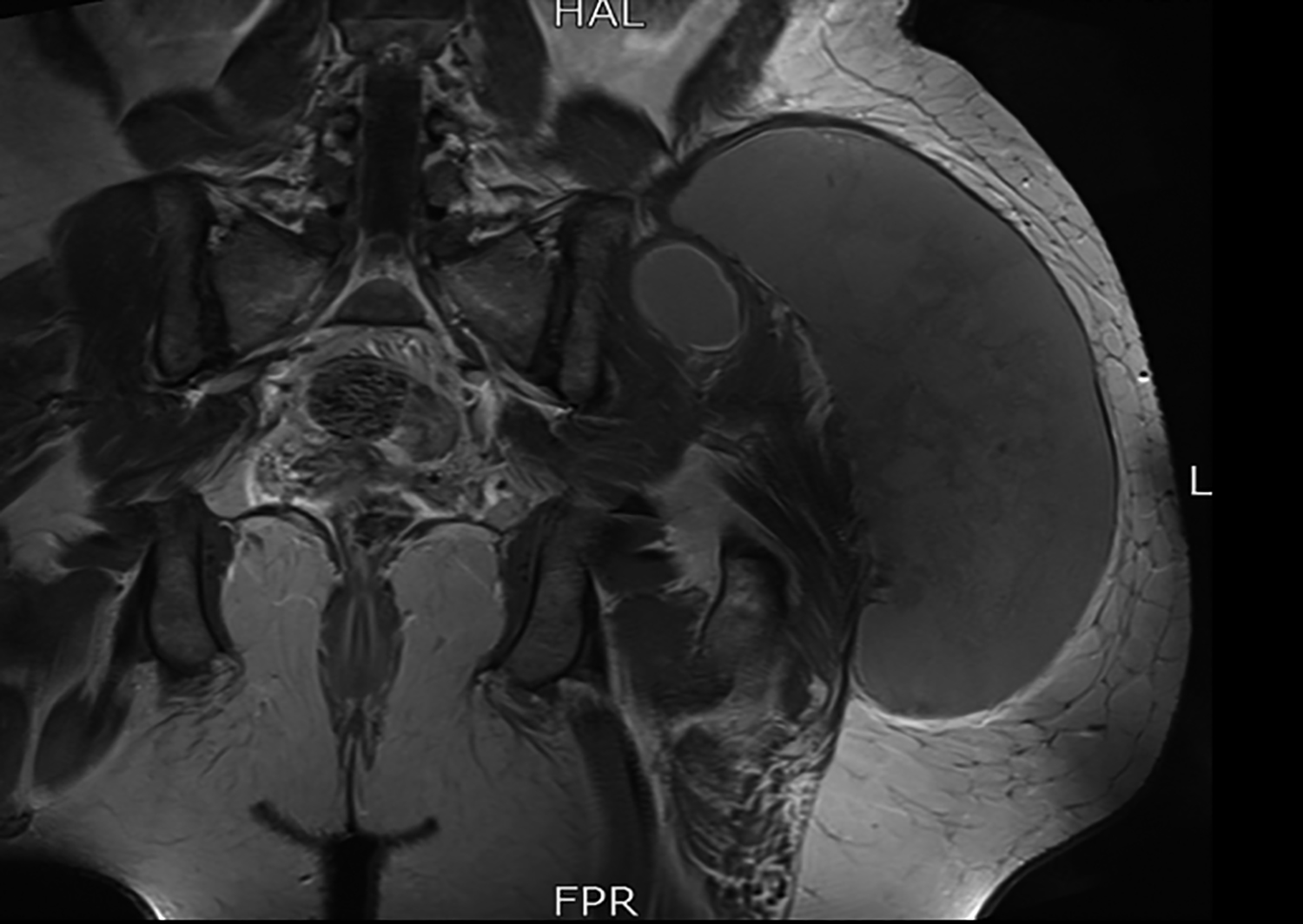 Figure 6: MRI coronal post-contrast image shows no post-contrast enhancement.
Figure 6: MRI coronal post-contrast image shows no post-contrast enhancement.
The location of the lesion determines the contents of the cavity, which can vary from blood and lymph to necrotic fat.4 When blood vessels are involved, the cavity swells rapidly while involvement of lymphatic channels results in gradual growth of the cavity.4
Morel-Lavellée lesions have varied clinical presentations. They have been described along knee, calf, buttocks, lumbar spine, and scapula.5 Their size can vary from several centimetres to very small fluid lesions. The lesion may have an acute or an insidious presentation, as seen in our case. Most chronic lesions tend to be firmly attached to the underlying fascia and are either oval or fusiform in shape.5 The predilection of this condition for certain locations has been attributed to the variation in fat tissue structure in different locations.1 Interestingly, the vicinity of trochanteric area is especially predisposed to Morel-Lavallée lesion, as in our patient who presented with a lesion near left pelvis and upper thigh. This might be attributed to the loose hypodermal tissue and subcutaneous presence of bony structures.6 Often, Morel-Lavallée lesion is overlooked in patients presenting with multiple injuries due to severity of other injuries.6 When the lesion is missed, it can grow gradually until it starts producing symptoms due to its size and compression of surrounding anatomical structures.
Diagnosis can be made clinically. Plain X-ray images have limited use in diagnosis of this lesion. They usually show a clearly delineated non-calcified soft tissue mass. Ultrasound may reveal hypoechoic or anechoic collection, which is typically compressible and usually located between deep fat and overlying fascia, regardless of age of the lesion.7 If hyperechoic areas are present, they represent fat in the lesion. On computed tomography (CT), fluid-fluid levels are seen due to pooling of blood and lymph from damaged blood vessels and lymphatic channels. Debris, including fat droplets, with or without an encircling capsule, may also be seen. MRI is the best technique available for diagnosis of Morel-Lavallée lesion. The edges of the cystic lesion are seen as uninterrupted lines along the surrounding fascial planes, while the internal appearance may vary depending upon the blood/lymph content. A capsule, which appears as a hypointense margin due to its fibroid structure, is usually present in chronic lesions.8 Other features that may be seen include: variable signal intensity on T1 weighted images, heterogenous hyperintensity on T2-weighted images (seen in chronic organising hematoma), peripheral enhancement, and water-like MRI features (seen in long-standing lesions).8 In 2005, Mellado et al. proposed a classification system for Morel-Lavallée lesion comprising of six levels based on radiological findings, such as homogenous or heterogeneous hypo- or hyper-intensity on T1- and T2-weighted MRI scans, fibrous capsule or pseudocapsule formation, and presence of sinus tract, with findings associated with chronicity increasing with higher level.
Complications, if improperly managed, include infection of the cavity and overlying skin necrosis due to compromised blood supply.9 These lesions usually resolve spontaneously by absorption of fluid but in some chronic cases, a pseudocapsule can develop.9 Morel-Lavallée lesion can contain multiple internal septations in the cavity, as in our case.1
There is no consensus on the treatment of choice for Morel-Lavallee lesion. Conservative management, e.g. applying pressure on the affected area and physical rest, often resolves small-sized lesions.1 For lesions of larger size or the lesions unresolved by conservative management, needle aspiration or surgical intervention may be necessary. Interestingly, in one study conservative measures were found to be effective in nearly 52% of cases.10 Most chronic lesions usually have an encircling capsule, lowering the chances of automatic healing. In such cases, surgery can alleviate symptoms and also prevent recurrence of infection in the lesion.1 Given the chronicity and extensive tissue involvement in our case, surgical excision was performed with favourable outcomes.
In summary, early diagnosis and treatment of Morel-Lavallee lesion are essential to prevent development of complications. The management depends on the age of the lesion along with some other factors.
PATIENT'S CONSENT:
The authors stated that informed consent was obtained from the patient prior to publishing this case.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS' CONTRIBUTION:
AHS, MTL, MSS: Wrote the manuscript,
MSK: Obtained images
HH: Performed literature review
REFERENCES
- Zairi F, Wang Z, Shedid D, Boubez G, Sunna T. Lumbar Morel-Lavallée lesion: Case report and review of the literature. Orthop Traumatol Surg Res 2016; 102(4): 525-7. doi.org/10.1016/j.otsr.2016.01.00
- Efrimescu CI, McAndrew J, Bitzidis A. Acute lumbar Morel-Lavallee haematoma in a 14-year-old boy. Emerg Med J 2012; 29(5):433. doi: 10.1136/emermed-2011-200660.
- Yilmaz A, Yener O. Giant post-traumatic cyst after motorcycle injury: A case report with review of the pathogenesis. Prague Med Rep 2013; 114(2):123-7. doi: 10.14712/23362936.2014.30.
- Pujol RM, Wang CY, Gibson LE, Su WP. Lipomembranous changes in nodular-cystic fat necrosis. J Cutan Pathol 1995; 22(6):551-5. doi: 10.1111/j.1600-0560.1995.tb01150.x.
- Jovanović M, Janjić Z, Vučković N. Giant post-traumatic cyst after closed degloving injury. Archive of Oncology 2007; 15(1-2):42-4. doi.org/10.2298/AOO0702042J.
- Hudson DA. Missed closed degloving injuries: Late presentation as a contour deformity. Plast Reconstr Surg 1996; 98(2):334e337. doi: 10.1097/00006534-199608000- 00020.
- Parra JA, Fernandez MA, Encinas B, Rico M. Morel-Lavallée lesions in the thigh. Skeletal Radiol 1997; 26:239-41.
- Payne WG. Morel-Lavallée lesion. Eplasty 2014; 14:ic12.
- Shaikh S, Faiq SM. Morel-Lavellee lesion: An uncommon entity needs imaging consideration. PJR 2018; 28(1).
- Miller J, Daggett J, Ambay R, Payne WG. Morel-Lavallée lesion. Eplasty 2014; 14:ic12.