Mesenteric Hematoma: Challenges in Diagnosis and Management
By Kamal Kant Sahu, Ajay Kumar Mishra, Amos Lal, Iryna ChastainAffiliations
doi: 10.29271/jcpsp.2020.06.667
Sir,
Mesenteric hematoma (MH) is a rare but a fatal complication of antithrombotic therapy, if not managed properly. Through this letter, we discuss the important bedside clinical signs of intra-abdominal bleeding and management strategies.
 Figure 1A: Ecchymosis extending from flank to the front of the lower abdomen, with approximate dimensions of 5×5 cm.
Figure 1A: Ecchymosis extending from flank to the front of the lower abdomen, with approximate dimensions of 5×5 cm.
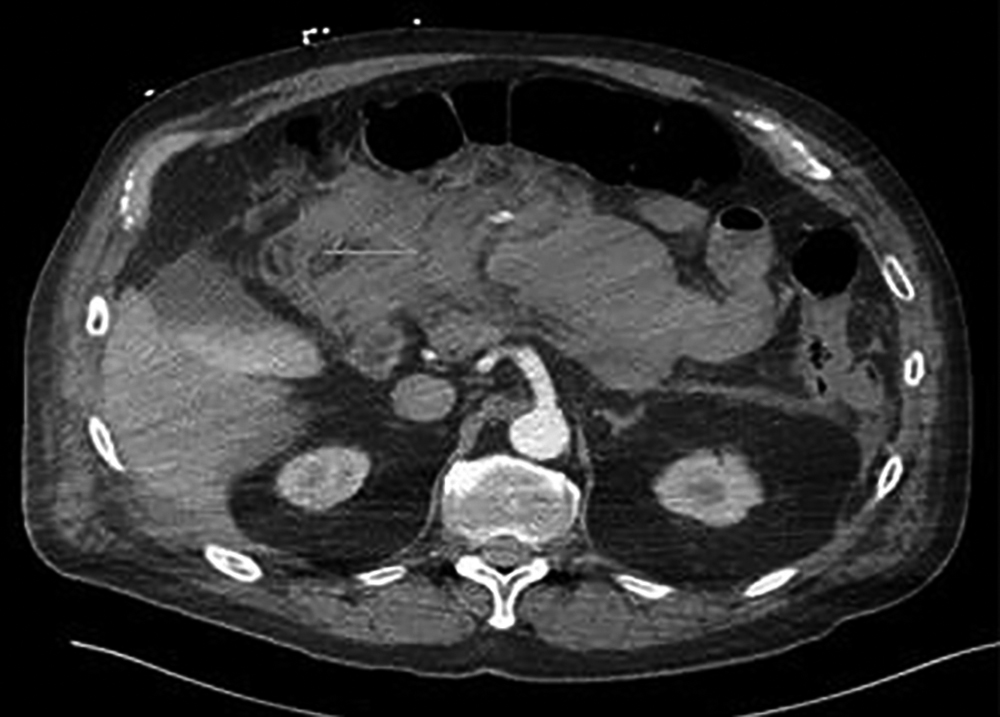 Figure 1B: CT abdomen transverse section showing large mesenteric hematoma (8×8×6 cm) with adjacent mesenteric fat stranding with a higher attenuation of 45-50 HU.
Figure 1B: CT abdomen transverse section showing large mesenteric hematoma (8×8×6 cm) with adjacent mesenteric fat stranding with a higher attenuation of 45-50 HU.
A 65-year old man with a past medical history of atrial fibrillation, on warfarin, presented for abdominal pain of three days' duration. Examination showed bluish discoloration of approximately 5x5 cm over his right flank (Figure 1A). Investigations showed large MH (Figure 1B), anaemia (Hb-7.2 gm/dL) and coagulopathy (INR-4.3). His warfarin was stopped. He was given 2 units of packed red blood cells (PRBCs) and 5 mg Vitamin K, after which his clinical condition improved without recurrence of symptoms or further fall in haemoglobin.
Bluish discolouration involving the flank and extending on to the front of the abdomen, above the hip, is classically known as Grey Turner's sign.1 It has been classically described in haemorrhagic pancreatitis resulting in a large retroperitoneal hematoma (RPH). In various prospective studies, this clinical sign is reported to be present in around ~1% of patients with acute pancreatitis.2-4 It is postulated to result from methaemalbumin (MHA), an albumin complex formed as a result of combination of albumin and heme, giving bluish-brown color to the skin when it leaks into the fascial plains. Similarly, Cullen’s and Fox’s signs are two other clinical signs (Table I).
RPH is a rare complication, with an incidence of 1.3% to 6.6% per year. Hypotension, altered mentation and death are expected sequelae in cases of massive RPH, if not addressed timely. Underlying comorbidities like bleeding diathesis, thrombocytopenia, and use of anticoagulation could be extremely devastating. In most cases, RPH needs a supportive medical management only which includes stopping inciting antithrombotic agent, transfusing blood products including use of reversal agents like Vitamin K, Kcentra, etc. Though FDA has approved targeted anti-reversal agents, namely, idarucizumab (dabigatran’s reversal agent), Andexanet (Factor Xa inhibitor’s reversal agent), they are still far from practical uses due to high cost and insurance-related obstacles. Hence, warfarin remains the widely considered anticoagulant given the universal availability of fresh frozen plasmas (FFPs), Vitamin K, etc.5,6 Very rarely, surgical ligation is required in case active bleeding vessel is recognised and patient remains hemodynamically instable despite best supportive care. Moreover, the role of interventional radiology-guided approach is increasingly being popular owing to its simplicity, less complications and outstanding outcome. Embolization can be either by local thrombus formation or by local polymer formation.
Once the patients are appropriately managed for bleeding episode, next few questions arise: How long should we wait to restart anticoagulation? Would direct oral anticoagulants (DOACs) be a better choice than warfarin? How to follow patients with RPH, and the role of imaging?
Available literature suggests that it is reasonable to restart anticoagulants after four to seven days of stoppage of bleeding.5 Till date, there is no study to compare warfarin vs. DOACs with regard to anticoagulation of choice during post-bleeding episode.
We aim to emphasise that the role of various imaging techniques and investigations should be an add-on to the clinical examination and not to replace them. Reporting of such cases will ensure to keep the zeal of bedside examination intact amongst the internists.
Table I: Table showing signs, mechanism of development, associated conditions and their clinical significance.|
Signs |
Location |
First reported by |
Mechanism of sign |
Seen in |
|
Grey Turner’s |
Ecchymosis/discoloration of the flanks |
British surgeon George Grey Turner |
Enzymatic digestion digested blood tracks subcutaneously around the abdomen from the inflamed pancreas |
|
|
Cullen sign |
Periumbilical ecchymosis |
American gynecologist, Thomas Stephen Cullen |
Results from blood tracking subcutaneously along the gastrohepatic and falciform ligament around the umbilicus |
|
|
Fox’s sign |
Upper thigh along the inguinal ligament |
American dermatologist, George Henry Fox |
Blood extravasation along the fascial plain of psoas and iliacus muscle beneath the inguinal ligament which then manifests as subcutaneous discoloration in the upper thigh |
|
|
Bryant’s sign |
Blue discoloration of the scrotum |
John Henry Bryant |
Extravasation of blood beneath intact penile or scrotal epithelium |
|
|
Stabler’s sign |
Bruising of the pubis and groin |
Francis Edward Stabler |
Extravasation of blood in subcutaneous plain in inguinal-pubic area |
|
|
Seat Belt sign |
Bleeding in the Subcutaneous plain along the diagonal strap |
Garrett and Braunstein |
Contusion usually sustained during motor vehicle accident |
|
|
Fountain’s sign |
Ultrasonographic sign in transverse color Doppler of scrotum |
- |
Hypervascularity of the scrotal sac wall gives an impression of Fountain in doppler study |
|
CONFLICT OF INTEREST:
Authors declared that none of them had any conflict of interest.
AUTHORS’ CONTRIBUTION:
KKS, AKM, AL, IC: Case management, review of literature, manuscript writing, table making and proof reading.
KKS, AKM: Photography.
REFERENCES
- Rao AG, Swathi T, Farheen SS, Kolli A, Hari S, Reddy UD, et al. Desmoid tumor of rectus abdominis presenting with grey-turner's and cullen's sign: A report of a rare case. Indian J Dermatol 2017; 62(3):318-20.
- Sahu KK, Mishra AK, Zhang P. Femoral neuropathy: A rare presentation of retroperitoneal hematoma with review of literature. Indian J Hematol Blood Transfus 2019; 01126-5.
- Wright WF. Cullen sign and grey turner sign revisited. J Am Osteopath Assoc 2016; 116(6):398-401.
- Sahu KK, Maradana S, Mishra A, Chastain I. A spontaneous rectus sheath hematoma. Intern Emerg Med 2018; 13(8): 1341-3.
- Colantino A, Jaffer AK, Brotman DJ. Resuming anticoagulation after hemorrhage: A practical approach. Cleve Clin J Med 2015; 82(4):245-56.
- Sahu KK, Mishra AK, Lal A, George SV. Retroperitoneal and rectus sheath hematomas: Challenges in diagnosis and management. Am J Surg 2019; S0002-9610(19)30764-0.