Mature Orbital Teratoma
By Rabia Chaudhry, M. Nasar Qamar, Areej RiazAffiliations
doi: 10.29271/jcpsp.2021.05.596ABSTRACT
Orbital teratoma is a rare tumour that is composed of tissues derived from all three germ cell layers. It presents, in otherwise, healthy neonates with unilateral proptosis that progresses rapidly, threatening vision through optic nerve compromise or exposure keratopathy. Globe conservation may be difficult too in advanced cases. Mature teratomas are benign, but the immature ones can sometimes become malignant. We report a case of a six-month female infant who presented with mature orbital teratoma since birth. Vision could not be salvaged; but following complete surgical excision, good cosmesis was achieved.
Key Words: Mature teratoma, Orbit, Congenital tumour, Surger.
INTRODUCTION
Congenital orbital teratomas are rare tumours composed of tissues derived from all three germinal layers.1 They cause severe unilateral proptosis that may result in optic nerve compromise and exposure keratopathy.2 They show rapid growth but malignant conversion is rare.1 Most common locations for teratoma are gonads, sacrococcyx, retroperitoneum and mediastinum.3,4 Head and neck teratomas make up only 9% of all cases and among these, the orbital teratomas make up a very small number.3,4 Recurrences can occur.5 The aim of management is primarily to save the globe so that normal orbitofacial development is possible. Salvaging the vision is not possible in many cases due to secondary optic atrophy and exposure keratopathy. Here, we report a case of a six-month female infant, who presented with a mature orbital teratoma that had compromised the vision due to secondary optic atrophy, but the globe could be saved and good cosmetic outcome achieved.
CASE REPORT
A six-month female infant, result of a non-consanguineous marriage and uneventful term delivery, presented with progressive proptosis of left eye since birth. On examination, extreme proptosis and lateral displacement of the left globe along with distension of lids was seen (Figure 1). Mild conjunctival hyperemia was seen but the cornea did not show any signs of exposure keratopathy. There was scarring along medial aspect of orbit, indicative of a surgical procedure in the past.
 Figure 1: Preoperative clinical images: (a) non-axial proptosis of left eye; (b) closer view.
Figure 1: Preoperative clinical images: (a) non-axial proptosis of left eye; (b) closer view.
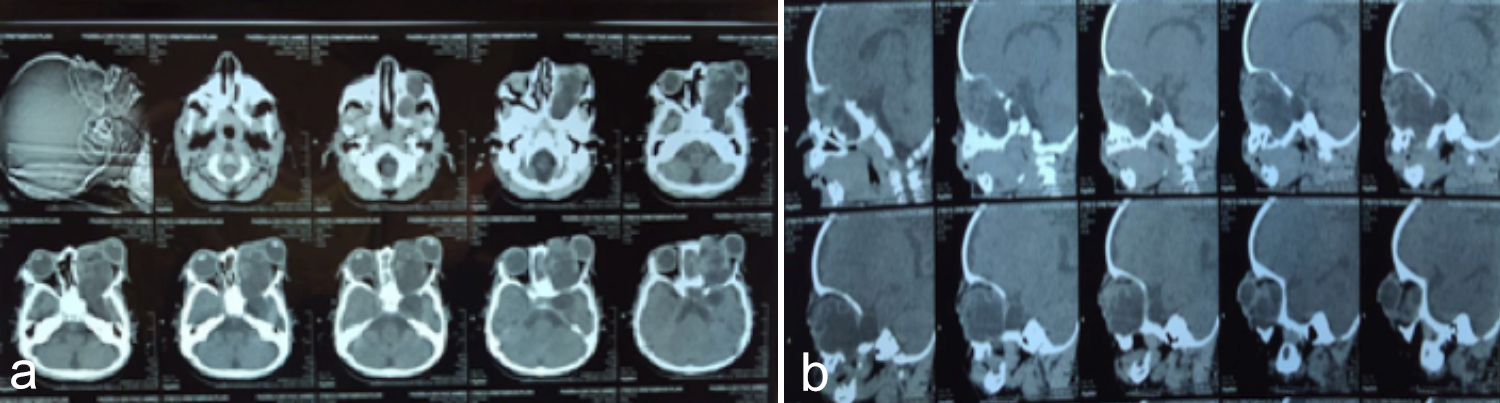 Figure 2: Preoperative CT images showing a huge mass filling up the entire left orbit: (a) axial view; (b) coronal view.
Figure 2: Preoperative CT images showing a huge mass filling up the entire left orbit: (a) axial view; (b) coronal view.
On further enquiry, it was revealed that a previous incisional biopsy had been done elsewhere; but the parents had lost the histopathology report. The child could only follow light in the left eye. Left relative afferent pupillary defect was present. Fundus examination showed pale optic disc in the left eye. The right eye was completely normal. The child was, otherwise, fully healthy.
Computed tomography scan (Figure 2) and magnetic resonance imaging revealed a huge well-defined largely cystic, multiseptated mass, filling up the left orbit completely, causing forward and lateral displacement of the globe. Expansion of bony orbit without any bony erosion was present. No extension to surrounding structures was seen. Optic nerve and extraocular muscles could not be visualised separately from the mass. Routine blood tests, chest x-ray and ultrasound abdomen were normal. Serum alpha fetoprotein (AFP) was elevated at 144.8 ng/ml (normal: <20 ng/ml). Serum beta-HCG level was less than 0.1 mIU/ml (normal: <1 mIU/ml).
Complete surgical excision through a superomedial orbitotomy approach was performed. Globe was not penetrated by the mass so it was preserved. Histopathological examination revealed a lesion composed of mature, columnar epithelium, fibroadipose tissue, glial tissue, mucous and serous acini and mature cartilage. On the basis of the presence of mature elements, derived from all three germ cell layers, diagnosis of mature orbital teratoma was made. Although vision could not be salvaged in our patient because of late presentation, but good cosmetic outcome was achieved (Figure 3). Six-monthly follow-up was advised to look out for recurrence.
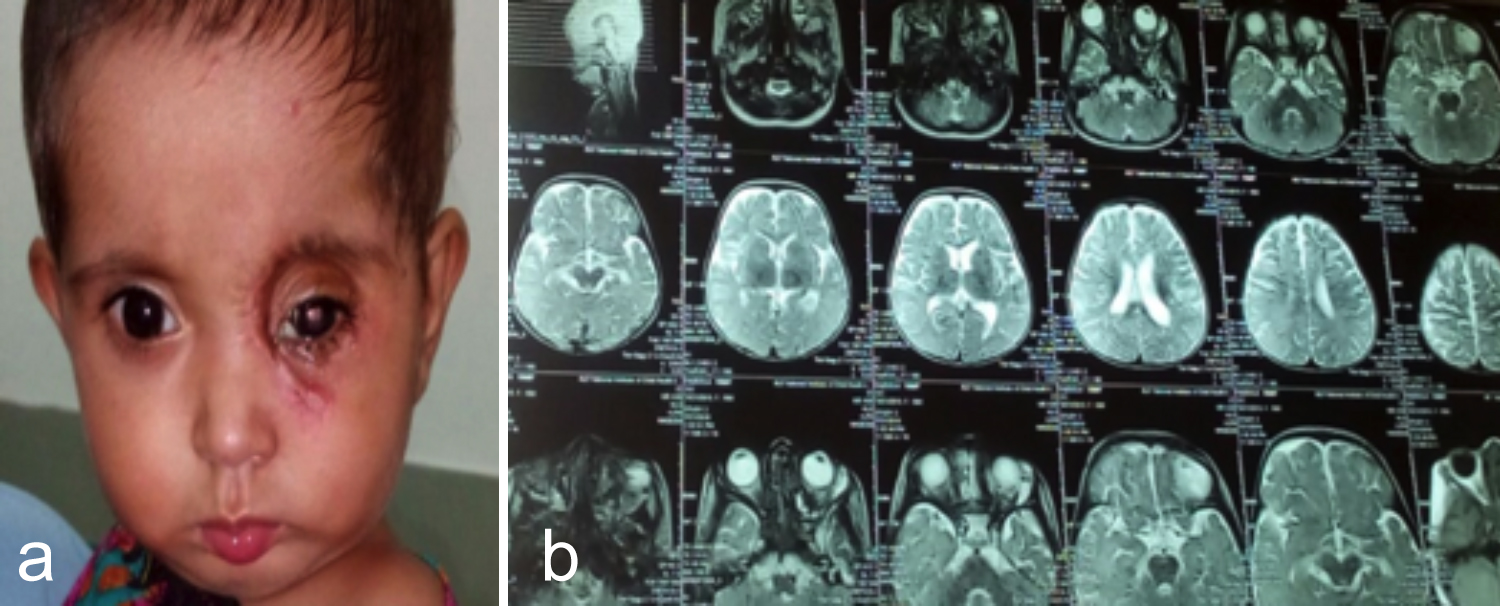 Figure 3: Postoperative: (a) clinical image showing a good cosmetic outcome; (b) MRI image depicting orbit free of any residual mass.
Figure 3: Postoperative: (a) clinical image showing a good cosmetic outcome; (b) MRI image depicting orbit free of any residual mass.
DISCUSSION
Teratomas are rare benign tumors that arise from pluripotent stem cells that can differentiate into all three germinal layers. They are usually diagnosed after birth, but some reported cases have been picked up prenatally, too.5 Historically, orbital teratomas were classified on the basis of germinal layers present and the degree of differentiation.6 However, the latest classification focuses more on management and prognosis aspects and divides orbital teratomas into four groups as follows:7 primary intraocular teratoma, primary orbital teratoma, combined orbital and extraorbital teratoma, and secondary orbital teratoma. The teratoma is considered mature when the tumor tissue is uniformly mature resembling adult tissues.8 Immature teratoma, on the other hand, contains immature or embryonal tissue which can have malignant and metastatic potential. 8 Orbital teratoma is more common in females.9 It is more often seen in left orbit.9
Clinically, teratomas present in otherwise healthy neonates with severe progressive proptosis and extreme stretching of lids over a transilluminating fluctuating mass.10 The globe is developed normally but may undergo changes secondary to displacement by the mass. Rapid growth after birth is attributed to collection of glandular secretions within cystic spaces. The optic nerve may be surrounded by or adherent to the tumour leading to optic atrophy.
On imaging, orbital teratoma is seen as a well-defined multiloculated cystic mass showing mixture of tissues along with calcification but not causing any bony destruction.5 Routine prenatal ultrasound may or may not detect it. The differential diagnoses include dermoid cyst, lymphangioma, hemangioma, epidermal inclusion cyst and encephalocele.5 However, clinical distinction between these entities is very difficult; hence, despite the difficulty in preoperative diagnosis, early surgery is still recommended.
The goal of treatment is to salvage the vision and globe, wherever possible, in order to gain good function and cosmesis. Depending on the extent of growth, simple excision, enucleation or exenteration may be required followed by prosthesis placement where needed. Similar to present case, Sahraoui et al.6 reported an orbital teratoma, where globe preservation was possible; whereas, Gonzalez et al.1 and Prakash et al.9 documented cases where extensive tumour growth warranted an enucleation and exenteration, respectively. Following excision, detailed histopathological evaluation of the entire tumour is necessary to detect possible malignant component. Recurrence of orbital teratomas is rare, but has been reported with immature teratomas, so periodic follow-up is necessary.7
CONCLUSION
Orbital teratomas are very rare, yet potentially curable congenital tumours, so they should be included in the differential diagnoses of rapidly progressive proptosis in a neonate. Moreover, early surgical intervention aiming at compete surgical excision with globe preservation, wherever possible, should always be considered.
PATIENT'S CONSENT:
Formal consent was taken from the parents of the child to publish the data related to the case.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
RC, MNQ: Diagnosis and management.
AR: Data collection and manuscript writing.
REFERENCES
- Gonzalez C, Restrepo CA, Salazar GI, Monsalve P. Congenital orbital teratoma case report. Colomb Med 2012; 43:82-85. doi.org/10.25100/cm.v43i1.1062.
- Aiyub S, Chan W, John S, Sullivan LJ, Pater J, Cooper P, et al. Congenital orbital teratoma. Indian J Ophthalmol 2013; 61(12):767-9. doi: 10.4103/0301-4738.111219.
- Mehta M, Chandra M, Sen S, Bajaj MS, Pushker N, Meel R. Orbital teratoma: A rare cause of congenital proptosis. Clin Experiment Ophthalmol 2009; 37:626-8. doi.org/10.1111/ j.1442-9071.2009.02077.x.
- Herman TE, Vachharajani A, Siegel MJ. Massive congenital orbital teratoma. J Perinatol 2009; 29:396-7. doi.org/ 10.1038/jp.2008.205.
- Patel B. Benign orbital tumors: Teratoma. Clinical ophthalmic oncology: Orbital tumors 2014; 1: 83-4. doi.org/ 10.1007/978-3-642-40492-48.
- Khadka S, Shreshta GB, Gautam P, Shreshta JB. Orbital teratoma: A rare congenital tumour. Nepal J Ophthalmol 2017; 9(18):79-82. Doi:10.3126/nepjoph.v9i1.17540.
- Kivelä T, Tarkkanen A. Orbital germ cell tumors revisited: A clinicopathological approach to classification. Surv Ophthalmol 1994; 38:541-4. doi.org/10.1016/0039-6257 (94)90147-3.
- Alkatan HM, Al-Obaidan OS, Kfoury H, Al-Faky YH. Orbital immature teratoma a rare entity with diagnostic challenges. Saudi J Ophthalmol 2018; 2(1) doi.org/10. 1016/j.sjopt.2017.12.005.
- Prakash MVS, Indira R, Radhakrishnan M, Leela G. Malignant orbital teratoma in a neonate: A clinopathological report. J Postgrad Med 2017; 63:203-5. doi.org/10.4103/jpgm.jpgm_629_16.
- Pellerano F, Guillermo E, Garrido G, Berges P. Congenital orbital teratoma. Ocul Oncol Pathol 2017; 1:11-16. doi.org/10.1159/000448144.