Effect of Ramadan Fasting on Thyroid Hormone Levels in Patients on Levothyroxine Treatment
By Fatma Dilek Dellal1, Berna Ogmen1, Didem Ozdemir1, Afra Alkan2, Fatma Neslihan Cuhaci Seyrek1, Sefika Burcak Polat1, Reyhan Ersoy1, Bekir Cakir1Affiliations
doi: 10.29271/jcpsp.2020.10.1009ABSTRACT
Objective: To evaluate the changes in thyroid functions in Ramadan, and compare late evening and pre-seheri use of levothyroxine in patients with hypothyroidism.
Study Design: Cross-sectional study.
Place and Duration of Study: Department of Endocrinology, Ankara Ataturk Education and Research Hospital and Ankara Yildirim Beyazit University, Turkey, from May to June 2018.
Methodology: Patients who were on levothyroxine treatment and having normal thyroid functions were recruited for the study in the last one week before Ramadan. Patients were offered to take levothyroxine at 22.30-23.00 pm before sleep or between 01:30-03:00 am at least 30 min pre-seheri.
Results: There were 53 (85.5%) female and 9 (14.5%) male patients. Basal thyrotrophin (TSH) was 2.02 μIU/mL (0.27-4.14) and insignificantly increased at the end of Ramadan [2.18 μIU/mL (0.04-19.69), p=0.167]. Free-triiodothyronine (fT3) decreased while free-thyroxine (fT4) increased (p<0.001 for both). Eighteen patients preferred to take levothyroxine in late evening and 44 preferred to take at pre-seheri. There were insignificant increases in TSH in both groups (p=0.401 and p=0.276, respectively). At the end of Ramadan, TSH increased in 39 (63.9%), decreased in 22 (36.1%), and did not change in one patient.
Conclusion: Increase in TSH was not significant after Ramadan. While there was an insignificant increase in median TSH, about one-third of patients had lower TSH, indicating for the need to evaluate every patient individually and follow closely during Ramadan. Clinical studies with larger sample sizes will be helpful to determine the optimal time for levothyroxine use during Ramadan.
Key Words: Thyroid functions, Ramadan fasting, Hypothyroidism, Levotyhroxine.
INTRODUCTION
Muslims change their eating and sleeping habbits during Ramadan, which is an Islamic lunar month. They usually eat two main meals with a greater amount and more variety of foods. One of these meals is called seheri which is eaten before sunrise; and the other is iftar, which is eaten just after sunset. Sleeping time is usually reduced or interrupted with variable sleep-awakening periods.
All these alterations in eating and sleeping habits might cause some metabolical, biochemical and hormonal changes associated with normal circadian rhythm. There are a limited number of studies with contradictory results investigating the effects of Ramadan fasting on thyroid hormones.1-5
The main treatment of hypothyroidism, which is the most common functional thyroid disorder in the general population, is levothyroxine. It is known that the absorption of levothyroxine is optimal when taken during fasting.6 Number of studies evaluating changes in TSH, fT3 and fT4, and the optimal time of levothyroxine use during Ramadan is very scarce.7-9
In this study, the aim was to compare the thyroid functions before and at the end of Ramadan, and to investigate the effects of late evening and pre-seheri use of levothyroxine on thyroid functions in patients with hypothyroidism.
METHODOLOGY
This observational study was conducted at Ankara Ataturk Education and Research Hospital and Ankara Yildirim Beyazit University, Turkey, from May to June 2018. Ankara is located in North hemisphere at 39.92 latitude and 32.85 longitude. In 2018, Ramadan month was between 16th May and 14th June, and evening meal (iftar) was taken after 20:04-20:25 pm (sunset occurs later towards the end of the month); and seheri was taken before 3:42-3:17 am (sunrise occurs earlier towards the end of the month). Thus, duration of fasting during the day was about 16-17 hours.
Patients who were seen in the last one week before Ramadan (8-15 May 2018) in this outpatient clinic were recruited for the study. Patients taking levothyroxine for primary, postoperative or postradioactive iodine hypothyroidism, and had normal thyroid functions without any need for change in levothyroxine dose and who were planning to fast for more than 15 days in Ramadan were included. Patients who were taking medicines that might interfere with levothyroxine absorption (calcium, iron preparations, proton pump inhibitors, etc.), patients with gastrointestinal malabsorption (Crohn, celiac disease, etc.), and having previous history of gastrointestinal surgery were excluded. Pregnancy, systemic diseases such as malignancy, chronic renal failure, chronic liver disease and fasting less than 15 days were also considered as exclusion criteria. Demographical and clinical data were obtained and basal thyroid functions were measured between 8.00-10.30 am after at least 8 hours of fasting.
One hundred and fifteen patients were recruited for the study. Follow-up data was available in 75 (65.2%) patients. Thirteen patients were excluded from the study at the end of Ramadan for various reasons and data of 62 patients were analysed. Flowchart of the study is shown in Figure 1. Before Ramadan, all patients were taking levothyroxine before breakfast. They were offered to take levothyroxine at 22.30-23.00 pm before sleep or between 01:30-03:00 am at least 30 minutes pre-seheri. According to their preference, patients were grouped as late evening and pre-seheri. At the 26-28th day of Ramadan (11-13 June 2018), thyroid functions were re-evaluated. The number of fasting days, time of levothyroxine use, and fasting durations before and after drug use, were recorded. In addition, the time of blood sampling was recorded and duration of fasting before sampling and duration between sampling-drug use were determined. Patients were asked to make a subjective assessment about their well-being and state whether they feel better, worse or unchanged during Ramadan.
Venous blood samples for TSH, fT3, fT4, antithyroid peroxidase antibody (anti-TPO), and antithyroglobulin antibody (anti-Tg) were measured by chemiluminescence methods (Immulite 2000; Diagnostic Products Corporation, Los Angeles, CA; and UniCel DxI 800; Beckman Coulter, Brea, CA). The reference ranges for TSH, fT3, fT4, anti-TPO, and anti-Tg were 0.4-4 mIU/mL, 1.57-4.71 pg/mL, 0.61-1.12 ng/dL, <10 IU/mL, and <30 IU/mL, respectively. Patients with TSH in normal reference range was considered euthyroid. Anti-Tg levels were routinely measured in patients with differentiated thyroid cancer. Anti-TPO levels in these patients, and anti-TPO and anti-Tg levels in other patients were obtained from medical records, if measured in the last 12 months. The thyroid antibody levels over the upper range were accepted as positive.
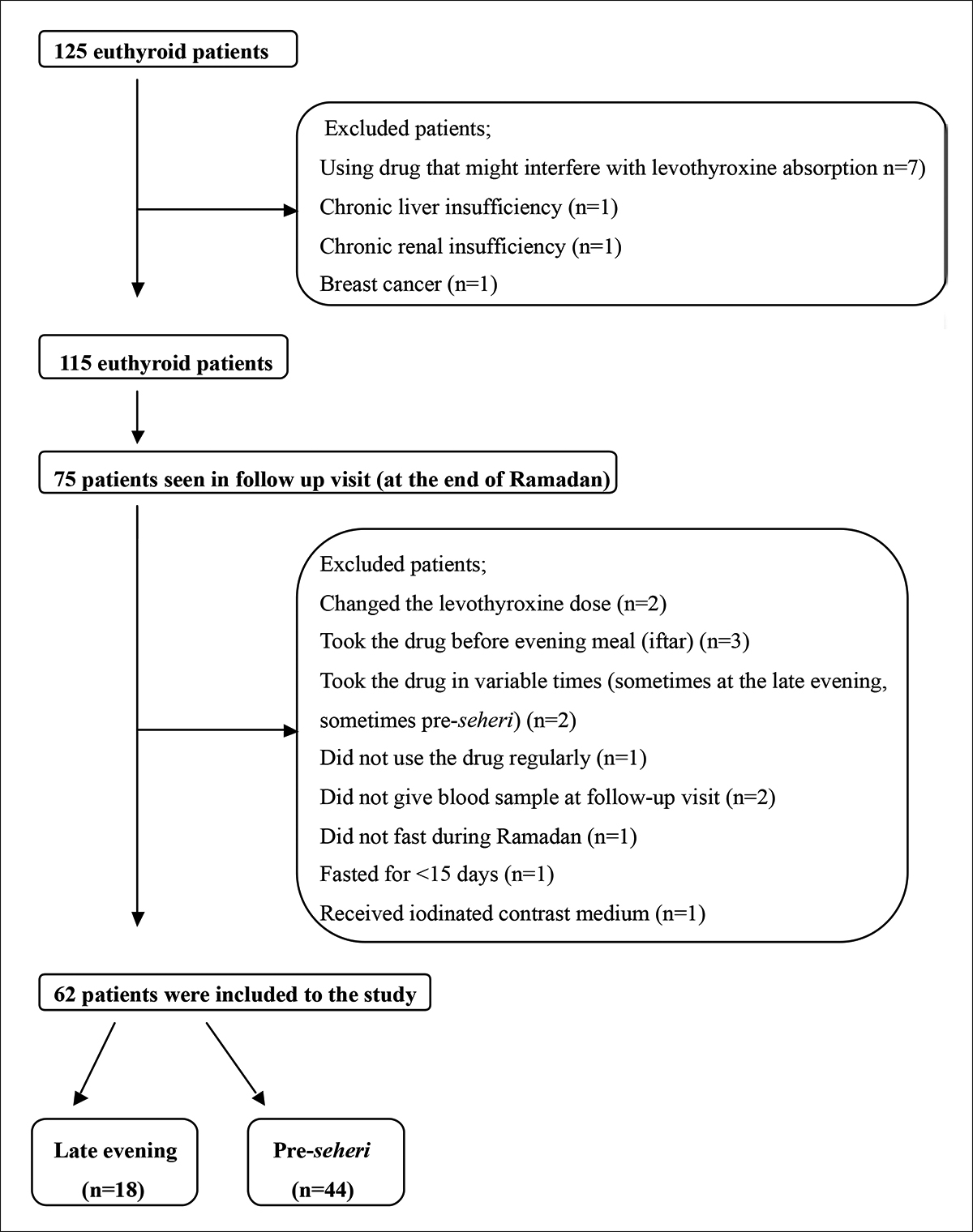 Figure 1: Flowchart of the study.
Figure 1: Flowchart of the study.
Thyroid functions of patients before Ramadan and at the last days of Ramadan were compared. The changes in TSH, fT3 and fT4 in two-time periods were compared between late evening and pre-seheri groups. Coefficient variant (CV) for TSH assay was determined. Positive and negative percent changes above CV value before and after Ramadan were considered as increase and decrease in TSH, respectively. All procedures performed in the study were in accordance with the ethical standarts of the instutional research committee (Ankara Yildirim Beyazit University Medical Faculty, 07.05.2018, Acceptance number: 26379996/141) and with the Helsinki Declaration.
The distributions of the continuous variables were examined by the Shapiro-Wilk’s test and the normality plots. All continuous and discrete variables were reported by median (min-max). Frequency and percentage were given for categorical variables. Demographical, clinical and laboratory features in late evening and pre-seheri groups, and in patients with increased and decreased TSH were compared by Mann-Whitney U-test and Chi-square test for numerical and categorical variables, respectively.
Table I: Demographical, clinical and laboratory features of patients.|
|
Total (n=62) Median (min-max) n (%) |
Late evening (n=18) Median (min-max) n (%) |
Pre-seheri (n=44) Median (min-max) n (%) |
P |
|
Age (years) |
49 (21-73) |
48.5 (30-72) |
49.5 (21-73) |
.433 |
|
Gender, Female |
53 (85.5) |
14 (77.8) |
39 (88.6) |
.427 |
|
Weight (Kg) |
75.7 (54.0-110.3) |
68.8 (57.2-99.1) |
77.2 (54.0-110.3) |
.461 |
|
BMI (Kg/m2) |
29.2 (20.8-44.0) |
27.5 (21.8-44.0) |
29.7 (20.8-41) |
.285 |
|
Etiology of hypothyroidism: Primary / postradioactive iodine Postoperative |
45 (72.6) 17 (27.4) |
11 (61.1) 7 (38.9) |
34 (77.3) 10 (22.7) |
.222 |
|
Duration of hypothyroidism (year) |
6.0 (0.3-25.0) |
4.5 (0.3-15.0) |
8.0 (0.7-25.0) |
.019 |
|
Comorbid diseases* |
13 (21.0) |
2 (11.1) |
11 (25.0) |
.312 |
|
Levothyroxine dose (mcg) |
85.7 (25.0-160.7) |
89.3 (50.0-160.7) |
80.3 (25.0-157.1) |
.168 |
|
Number of fasting days |
27 (17-29) |
27.5 (19-29) |
27 (17-29) |
.396 |
|
General well-being: Worse As usual Better |
15 (24.2) 36 (58.1) 11 (17.7) |
3 (16.7) 11 (61.1) 4 (22.2) |
12 (27.3) 25 (56.8) 7 (15.9) |
.621 |
|
Anti-TPO positivity (n=47) |
25 (53.2) |
6 (54.5) |
19 (52.8) |
1.000 |
|
Anti-TG positivity (n=53) |
15 (28.3) |
3 (21.4) |
12 (30.8) |
.732 |
|
Fasting BL (min) |
180 (0-330) |
90 (0-240) |
210 (15-330) |
<.001 |
|
Fasting AL (min) |
60 (20-240) |
188 (150-240) |
30 (20-105) |
<.001 |
|
Levothyroxine-BS time (h) |
9.7 (1.0-35.3) |
10.9 (8.9-35.3) |
9.0 (4.0-33.4) |
<.001 |
|
Fasting BBS (h) |
8.2 (5.5-17.4) |
8.6 (5.5-17.4) |
8.2 (6.0-13.5) |
.981 |
|
Patients with increased TSH |
39 (63.9) |
12 (66.7) |
27 (62.8) |
1.000 |
|
*Type 2 diabetes, hypertension, hyperlipidemia, coronary heart disease, asthma, chronic obstructive lung disease. BMI: Body mass index, Anti-TPO: Anti-thyroid peroxidase antibodies, Anti-TG: Anti-thyroglobulin antibodies, BL: Before Levothyroxine, AL: After Levothyroxine, BS: Blood sampling, BBS: Before blood sampling. |
||||
Table II: Changes in weight, body mass index and thyroid functions of patients that used levothyroxine at late evening and pre-seheri.
|
|
Total (n=62) |
Late evening (n=18) |
Pre-seheri (n=44) |
BGP |
GTIP |
|
Weight (kg): Before Ramadan After Ramadan WGP |
75.7 (54.0-110.3) 75.4 (51.7-106.9) <.001 |
68.8 (57.2-99.1) 67.5 (56.7-97.6) <.001 |
77.2 (54.0-110.3) 76.2 (51.7-106.9) .002 |
.461 .340 |
.087 |
|
BMI (kg/m2): Before Ramadan After Ramadan WGp |
29.2 (20.8-44.0) 28.8 (19.9-43.2) <.001 |
27.5 (21.8-44.0) 26.9 (21.5-43.2) <.001 |
29.7 (20.8-41.0) 29.5 (19.9-39.7) <.001 |
.285 .203 |
.388 |
|
TSH (μIU/mL): Before Ramadan After Ramadan WGp |
2.02 (0.27-4.14) 2.18 (0.04-19.69) .167 |
1.64 (0.32-3.95) 1.84 (0.04-7.67) .401 |
2.18 (0.27-4.14) 2.51 (0.24-19.69) .276 |
.100 .364 |
.725 |
|
fT3 (pg/mL): Before Ramadan After Ramadan WGp |
2.85 (1.81-4.22) 2.46 (1.28-3.96) <.001 |
2.81 (1.81-3.91) 2.50 (1.57-3.52) .006 |
2.86 (1.95-4.22) 2.44 (1.28-3.96) <.001 |
.932 .415 |
.208 |
|
fT4 (ng/dL): Before Ramadan After Ramadan WGp |
1.41 (0.95-1.97) 1.49 (0.67-2.75) <.001 |
1.56 (1.07-1.97) 1.52 (1.27-1.93) .278 |
1.38 (0.95-1.71) 1.46 (0.67-2.75) <.001 |
.032 .153 |
.369 |
|
BGP: Between-group comparison result, WGP: Within-group comparison result, GTIP: Group*Time interaction p value. BMI: Body Mass Index, TSH: Thyrotropin, fT3: free triiodothyronine, fT4: free thyroxine. |
|||||
The change in thyroid function test results during Ramadan were compared by F1-LD-F1 design, non-parametric approach to the longitudinal data, after detecting no significance effect of the weight change on these measurements by generalised linear mixed models. The trend of weight and BMI during Ramadan in groups were also investigated by F1-LD-F1 design. The results for the time effect within each group and the group-time interaction effect were supplied from F1-LD-F1 design. Moreover between-group comparisons were obtained by Mann-Whitney U-test.
Table III: Comparison of demographical, clinical and laboratory features in patients with increased and decreased thyrotropin.|
|
Increased TSH (n=39) Median (min-max) n (%) |
Decreased TSH (n=22) Median (min-max) n (%) |
BGP |
|
Age (years) |
50 (30-73) |
48.5 (21-63) |
.568 |
|
Gender, Female |
35 (89.7) |
17 (77.3) |
.263 |
|
Weight (kg): Before fasting After fasting WGp |
69.9 (54.0-99.0) 70.3 (51.7-97.7) <.001 |
82.2 (57.1-110.3) 79.8 (56.6-106.9) .012 |
(GTIP=.765) .005 .006
|
|
BMI (kg/m2): Before fasting After fasting WGp |
28.0 (20.8-35.5) 28.2 (19.9-35.0) <.001 |
31.3 (22.9-44.0) 30.5 (22.7-43.2) .002 |
(GTIP=.853) .056 .053
|
|
Etiology of hypothyroidism: Primary/postradioactive iodine Postoperative |
29 (74.4) 10 (25.6) |
15 (68.2) 7 (31.8) |
.826 |
|
Duration of hypothyroidism (year) |
5 (0.3-15) |
9 (1-25) |
.096 |
|
Comorbid diseases* |
6 (15.4) |
7 (31.8) |
.193 |
|
Levothyroxine dose (mcg) |
80.4 (25.0-160.7) |
92.9 (25.0-157.1) |
.362 |
|
Number of fasting days |
27 (17-29) |
27 (20-28) |
.933 |
|
Patients who used levothyroxine at pre-seheri |
27 (69.2) |
16 (72.7) |
1.000 |
|
General well-being: Worse As usual Better |
11 (28.2) 5 (12.8) 23 (59.0) |
4 (18.2) 5 (22.7) 13 (59.1) |
.492 |
|
Anti-TPO positivity |
19 (65.5) |
6 (35.3) |
.093 |
|
Anti-TG positivity |
11 (33.3) |
4 (21.1) |
.533 |
|
Fasting BL (min) |
180 (0-300) |
165 (0-330) |
.639 |
|
Fasting AL (min) |
60 (20-240) |
52.5 (30-240) |
.846 |
|
Levothyroxine-BS time (h) |
9.8 (1.0-35.1) |
9.5 (6.5-35.3) |
.563 |
|
Fasting BBS (h) |
8.4 (5.5-17.4) |
8.1 (5.9-13.5) |
.473 |
|
fT3 (pg/mL): Before fasting After fasting WGp |
2.85 (1.95-3.91) 2.41 (1.28-3.17) <.001 |
2.85 (1.81-4.22) 2.68 (1.80-3.96) <.001 |
(GTIP=.192) .254 .042
|
|
fT4 (ng/dL) Before fasting After fasting WGp |
1.43 (0.95-1.97) 1.43 (0.67-2.25) .588 |
1.35 (1.07-1.62) 1.58 (1.32-2.75) <.001 |
(GTIP<.001) .033 .010
|
|
*Type 2 diabetes, hypertension, hyperlipidemia, coronary heart disease, asthma, chronic obstructive lung disease. BGP: Between-group comparison result, WGP: Within-group comparison result, GTIP: Group Time interaction p-value. BMI: Body mass index, Anti-TPO: Anti-thyroid peroxidase antibodies, Anti-TG: Anti-thyroglobulin antibodies, BL: Before Levothyroxine, AL: After Levothyroxine, BBS: Before blood sampling, BS: Blood sampling, TSH: Thyrotropin, fT3: free triiodothyronine, fT4: free thyroxine. |
|||
RESULTS
Eighteen (29.0%) patients used levothyroxine at late evening and 44 (71.0%) used it at pre-seheri. Demographical, clinical and laboratory features of patients are shown in Table I.
Changes in weight, body mass index and thyroid functions of patients, who used levothyroxine at late evening and pre-seheri were shown in Table II. There were significant decreases in weight and BMI at the end of Ramadan. After fasting, TSH nonsignificantly increased, and fT3 and fT4 significantly decreased (WGP=.167, WGP <.001 and WGP <.001, respectively). TSH was increased in both late evening and pre-seheri groups without significance (WGP = .401 and WGP = .276, respectively). A need for change in levothyroxine dose occurred in 15 (24.2%) patients after Ramadan (increased in 11 and decreased in 4 patients). The changes over time for TSH, fT3 and fT4 were not significant (GTIP = .725, GTIP = .208 and GTIP = .369, respectively, Table II).
CV for TSH in May-June 2018 in our laboratory was 2.5%. There was only one patient with a change in TSH below this value (-1.59%). TSH had increased in 39 (63.9%) and decreased in 22 (36.1%) patients. Demographical, clinical and laboratory features of patients with increased and decreased TSH were compared in Table III.
DISCUSSION
According to the results of this study, TSH increased at the end of fasting in euthyroid patients using levothyroxine, but this increase was not statistically significant. Late evening or pre-seheri use of levothyroxine did not cause considerable changes in serum TSH, either.
In patients using levothyroxine, the effects of Ramadan fasting on TSH was evaluated in a very limited number of studies. Karoli et al. investigated effect of bedtime levothyroxine supplementation on TSH during Ramadan in 47 euthyroid patients and found that overall variation of TSH was ranging from 0.6 to 8 mIU/mL. The authors grouped patients according to change in TSH as ≥2 mIU/mL (increased) and <2 mIU/mL (unchanged) and reported no difference in age, sex and anti-TPO positivity between two groups. They concluded that a minimum of two-hour interval between the last meal and levothyroxine use was required; and suggested frequent and close monitoring of TSH for those in whom there is need to keep it in a narrow range.7 In their review on hypothyrodism and Ramadan, Hadjzadeh et al. evaluated four animal and seven human studies; and based upon their clinical experience, recommended to increase levothyroxine dose 25-50 mcg during and 15 days after Ramadan in women and elderly.10 Sheikh et al. found significanly increased TSH concentration in 64 hypothyroid patients after Ramadan month. The change in TSH was not affected by timing of levothyroxine intake and interval between last meal and drug use.8 In another study, Dabbous et al. evaluated thyroid functions in hypothyroid patients who used levothyroxine before dinner and pre-seheri. They reported that serum TSH increased and fT4 decreased in both groups. There was no diference in TSH increase among patients who used the drug before dinner and pre-seheri.9 In the present study, TSH was also increased in both late evening and pre-seheri groups, but this increase was not statistically significant. Lack of significant change in TSH might be related with relatively long half-life of TSH and short period of fasting in Ramadan. The changes in the form of increased or decreased TSH after Ramadan fasting might be explained by individual patients’ characteristics, consumption of different amount or type of foods, especially in different cultures and variations during fasting before levothyroxine use, which might effect absorbtion of the drug. Different results in the present study and the other study might be related with differences in methods, definition of significant change in TSH, and number of fasting days. The authors tried to determine an objective criteria for TSH change by calculating CV of TSH specific to the study period.
The increase in fT4 after Ramadan fasting in this study was most probably related with decreased time interval between levothyroxine use and blood sampling at the follow-up visit. This hypothesis can be supported by the finding that fT4 did not change in late evening group after Ramadan fasting, while significantly increased in pre-seheri group, in which levothyroxine use and blood sampling interval was significantly shorter. In contrary to the present study result, Dabbous et al. found significant decrease in fT4 in both pre-iftar and pre-seheri groups.9 This might be because their patient population became more hypothyroid compared to pre-Ramadan period. In theory, change in fT4 is not an expected finding after Ramadan fasting due to its relatively long half life. A possible explanation for significant decrease in fT3 in our study is inactivation of 5'-monodeiodinase and decreased conversion of T4 to T3 in prolonged fasting.11-13
The absorption of levothyroxine is optimal during fasting.6,14 It is recommended to take levothyroxine at least one hour before or four hours after the last meal. There are controversial findings about the optimal administration time of the drug. Although significantly lower and less variable TSHs were reported when taken in the morning compared to bedtime in a randomised crossover study. Another study showed similar TSH lowering effect with both morning and bedtime administration.15,16 In this study, TSH did not change significantly in groups that used levothyroxine in late evening and pre-seheri. Similarly, TSH was not affected by levothyroxine timing in other studies.8,9 In accordance with the study by Bolk et al., general well-being did not change in two groups.17 In contrary, Sheikh et al. observed an increase in quality of life scores in physical health, psychological health, and social relationships after Ramadan.8
This study has some limitations. Firstly, it included patients in a local area. Different results might be obtained in populations living in different geographical regions and with different nutrition culture. Secondly, other hormones (cortisol, growth hormone) or adipokines (leptin, adiponectin) were not evaluated that might change during fasting and influence thyroid hormones. Moreover, circadian rhythm of TSH was not determined. Another limitation is that the authors did not perform a detailed quality of life questionnaire.
CONCLUSION
The present study is one of the rare studies to compare the use of levothyroxine in late-evening and pre-seheri and to evaluate the effects of Ramadan fasting on TSH, fT4 as well as fT3 in patients with hypothyroidism. Although TSH increased in patients who fasted during Ramadan, the difference was not significant. In addition, TSH decreased in about one-third of patients, suggesting that every patient should be evaluated individually and followed closely during and after this period. Late evening or pre-seheri use of levothyroxine did not make any significant change in TSH.
ETHICAL APPROVAL:
Ethics Committee approval was received for this study from Ankara Yildirim Beyazit University Medical Faculty, on 07-05-2018 (No:26379996/141).
PATIENTS' CONSENT:
Informed consents were obtained from all patients prior to their participation in the study.
CONFLICT OF INTEREST:
Authors declared no conflict of interest.
AUTHORS' CONTRIBUTION:
FDD: Study design, data collection, literature review and writing.
BO, DO: Drafting of work.
AA: Statistical analysis.
FNCS, SBP: Data collection.
DO, RE, BC: Final review and approval of the article.
REFERENCES
- Sajid KM, Akhtar M, Malik GQ. Ramadan fasting and thyroid hormone profile. J Pak Med Assoc 1991; 41(9):213-6.
- Ahmadinejad Z, Ziaee V, Rezaee M, Yarmohammadi L, Shaikh H, Bozorgi F, et al. The effect of ramadan fasting on thyroid hormone profile: A cohort study. Pak J Bio Sci 2006; 9:1999-2002.
- Sulimanı RA. The effects of Ramadan fasting on thyroid functions in healthy male subjects. Nutrition Res 1988; 8(5):549-52. doi.org/10.1016/S0271-5317(88)80076-9.
- Bahrayni S, Vakili V, Nematy N, Norouzy A, Hashemy SI, Ebrahimi M, et al. The effect of ramadan fasting on thyroid hormones in 9-13 years old pre-menarche girls. J Nutrition Fasting Health 2013; 1(2):46-52.
- Ghiravani Z, Mesbahzadieh B. The effect of ramadan fasting on secretion thyroid hormones in healthy male adults. J Guilan Uni Med Sci 2006; 14(56):27-32.
- Fish LH, Schwartz HL, Cavanaugh J, Steffes MW, Bantle JP, Oppenheimer JH. Replacement dose, metabolism, and bioavailability of levothyroxine in the treatment of hypothyroidism. N Engl J Med 1987; 316(13):764-70. doi: 10.1056/NEJM198703263161302.
- Karoli R, Fatima J, Chandra A, Mishra PP. Levothyroxine replacement and Ramadan fasting. Indian J Endocrinol Metab 2013; 17(2):318-9. doi: 10.4103/2230-8210.109700.
- Sheikh A, Mawani M, Mahar SA. Impact of Ramadan fasting on thyroid status and quality of life in patients with primary hypothyroidism: A prospective cohort study from Karachi, Pakistan. Endocr Pract 2018; 24(10):882-8. doi: 10.4158/ EP-2018-0038.
- Dabbous Z, Alowainati B, Darwish S, Ali H, Farook S, Al Malaheem M, et al. A prospective study comparing two-time points of thyroid hormone replacement during the holy month of ramadan. Int J Endocrinol 2019; 2019: 9843961. doi: 10.1155/2019/9843961.
- Hadjzadeh MA, Pakdel R, Hayatdavoudi P, Nematy M. Hypothyroidism and ramadan fasting. J Fast Health 2014; 2(2):80-3.
- Spencer CA, Lum SM, Wilber JF, Kapten EM, Nicoloff JT. Dynamics of serum thyrotropin and thyroid hormone changes in fasting. J Clin Endocrinol Metab 1983; 56(5): 883-8. doi: 10.1210/jcem-56-5-883.
- Azizi F. Effect of dietary composition on fasting induced changes in serum thyroid hormones and thyrotropin. Metabolism 1978; 27(8):935-45. doi: 10.1016/0026- 0495(78)90137-3.
- Borst GC, Osburne RC, O'Brian JT, Georges LP, Burman KD. Fasting decreases thyrotropin responsiveness to thyrotropin-releasing hormone: A potential cause of misinterpretation of thyroid function test in the critically ill. J Clin Endocriol Metab 1983; 57(2):380-3. doi: 10.1210/ jcem- 57-2-380.
- Hays MT. Localisation of human thyroxine absorption. Thyroid 1991;1(3):241‑8. doi: 10.1089/thy.1991.1.241.
- Rajput R, Chatterjee S, Rajput M. Can levothyroxine be taken as evening dose? Comparative evaluation of morning versus evening dose of levothyroxine in treatment of hypothyroidism. J Thyroid Res 2011; 2011:505239. doi: 10.4061/2011/505239.
- Bach-Huynh TG, Nayak B, Loh J, Soldin S, Jonklaas J. Timing of levothyroxine administration affects serum thyrotropin concentration. J Clin Endocrinol Metab 2009; 94(10): 3905-12. doi: 10.1210/jc.2009-0860.
- Bolk N, Visser TJ, Nijman J, Jongste IJ, Tijssen JG, Berghout A. Effects of evening vs. morning levothyroxine intake: A randomised double-blind crossover trial. Arch Intern Med 2010; 170(22):1996-2003. doi: 10.1001/archinternmed. 2010.436.