Comparison of Guy’s, S.T.O.N.E. and CROES Scoring Systems for Predicting Percutaneous Nephrolithotomy Outcomes in Eldery Patients
By Salih Polat1, Serkan Yarimoglu2, Omer Koras3, Murat Sahan2, Ertugrul Sefik2, Ibrahim Halil Bozkurt2, Tansu Degirmenci2Affiliations
doi: 10.29271/jcpsp.2021.03.307ABSTRACT
Objective: To evaluate the efficacy and reliability of Guy’s (GSS), S.T.O.N.E., and CROES scoring systems developed to predict percutaneous nephrolithotomy (PCNL) outcomes in aged patients.
Study Design: Descriptive study.
Place and Duration of Study: Department of Urology, Ministry of Health University Izmir Bozyaka Training and Research Hospital and Department of Urology, Faculty of Medicine, Amasya University, Turkey, from April 2011 to January 2020.
Methodology: Patients aged 65 years and over, who underwent PCNL for kidney stones, were retrospectively analysed. The patients’ clinical and perioperative characteristics and the radiological features of the stones were obtained from the prospectively recorded data. GSS, S.T.O.N.E. and CROES nephrolithometry scores were calculated for each patient and their relation with stone-free status, complications, and perioperative findings were analysed.
Results: A total of 147 patients were included in the study. Stone-free status was achieved in 76.0% of the patients, and complications developed in 27.2%. All three scoring systems were associated with stone-free status and complication development. GSS (OR=0.213,p=0.005) and S.T.O.N.E. (OR=0.601, p=0.042) scores were detected as independent markers for stone-free status, while the CROES score was not an independent marker. Only diabetes mellitus was determined to be an independent marker for the development of complications (OR=2.375, p=0.045).
Conclusion: PCNL is an effective and safe treatment method with high stone-free rates in the treatment of large renal stones, but care should be taken in terms of cardiac risks. The results of this study showed that GSS and S.T.O.N.E. scoring systems were effective and reliable in predicting stone-free status.
Key Words: Aged, Nephrolithotomy, Percutaneous, Comorbidity, Stone-free status, Treatment outcome, Complications, Scoring systems.
INTRODUCTION
Percutaneous nephrolithotomy (PCNL) is recommended as the first-line treatment option with a high stone-free and acceptable complication rates for kidney stones that are either refractory to extracorporeal shock wave lithotripsy (ESWL) or >2 cm in diameter.1 However, PCNL can become more complicated in the presence of obesity, chronic kidney disease (CKD), comorbidities, and staghorn stones.2
With the increase in life expectancy, the number of patients of advanced age, who present to urology outpatient clinics for the treatment of renal stones, is gradually increasing. In the literature, it has been stated that the risk of blood transfusion increases with age, and increased age is also associated with postoperative complications and mortality. When planning treatment in this risky patient group, the success and complication rates after PCNL need to be fully known.3,4 However, the literature contains only a limited number of studies reporting PCNL outcomes in elderly patients, and there seems to be no specific standardisation.
Scoring systems have been developed to provide standardisation in reporting PCNL outcomes. The developed scoring systems are used for clinical decision, evaluation of surgical outcomes, counselling patient. Guy’s stone scoring (Guy’s SS), S.T.O.N.E. nephrolithometry, and CROES nomogram are most commonly used scoring systems in urology practice. Guy’s SS categorises patients into four grades (grade I-IV) according to stone burden and renal anatomy based on radiological findings.5 The S.T.O.N.E. scoring system consists of five parameters abbreviated as STONE. These parameters are (S) tone size, (T) ract length, degree of (O) bstruction, (N) umber of calyces involved, and stone (E) ssence (density).6 CROES is a nephrolithometric nomogram that includes patient characteristics in addition to radiological findings, using the continuous scale to grades PCNL success.7
Although there are studies evaluating the efficacy of Guy’s SS, S.T.O.N.E. and CROES systems in patients with obesity and CKD in the literature, there is no study evaluating the efficacy of these three scoring systems in elderly patients.
In the current study, the aim was to evaluate the efficacy and reliability of Guy’s SS, S.T.O.N.E. and CROES scoring systems in this patient group.
METHODOLOGY
Patients aged 65 years and over, who underwent PCNL for the treatment of renal stones at the Ministry of Health University, Izmir Bozyaka Training and Research Hospital, and Faculty of Medicine, Amasya University, between April 2011 and January 2020, were retrospectively analysed after the approval of the Ethics Committee of the Amasya University (Meeting/Decision No.1/12.21). Patients with unavailable preoperative computed tomography (CT) and laboratory data were excluded from the study. The clinical features and perioperative characteristics of the patients and the radiological features of the stones were obtained from the prospectively recorded data.
Clinical features included age, gender, body mass index (BMI), history of comorbidities, American Society of Anesthesiologists (ASA) score, extracorporeal shock wave lithotripsy (ESWL) history, and stone surgery history. Stone characteristics were stone burden, localisation and density. Perioperative characteristics referred to the number of access, puncture level, operation time (OT), fluoroscopy time (FT), nephrostomy tube removal time (NT), presence of residual stones, blood transfusion requirement (BTR), length of hospital stay (LOS), and complications. Stone burden was calculated in square millimeters using the ellipsoid formula: length x width x π x 0.25, where π is a mathematical constant equal to 3.14.8 The estimated glomerular filtration rate (GFR) was calculated using the Cockcroft–Gault formula.9
PCNL were performed in the prone position under general anesthesia. After the ureteral catheter was inserted in the lithotomy position, the patient was placed in the prone position, and access to the pelvicalyceal system was provided with an 18-G Chiba needle under fluoroscopy. After the guide wire was confirmed to be in the pelvicalyceal system, the tract was dilated up to 28 or 30-French with using Amplatz dilators. The stone fragmentation was achieved by a pneumatic lithotripter. Forceps were used in the extraction of the stones. At the end of the procedure, a 14-f nephrostomy was placed under fluoroscopy. The nephrostomy tube was clamped and removed on the first or second postoperative day in the absence of fever or marked hematuria. Fluoroscopy time was defined as the time elapsed from the beginning of calyceal access procedure to the insertion of the nephrostomy. OT was calculated as the time from prone positioning to nephrostomy tube placement.
The patients were evaluated with kidney-ureter-bladder X-Ray (KUB) at the first postoperative month. The patients with suspicious opacity on the radiograph, symptomatic cases, or patients with non-opaque stones were evaluated by CT. Stone-free status (SFS) was considered to be achieved in patients with stones of <4 mm without any symptom.
Guy’s SS, S.T.O.N.E., and CROES nephrolithometry scores were calculated for each patient, and their correlation with SFS, OT, FT, LOS, and BTR was evaluated. The patients were divided into four groups (grades 1-4) according to Guy’s SS, four groups according to CROES (grade 1:80–129, grade 2:130–169, grade 3:170–219, and grade 4:220–350), and three groups according to S.T.O.N.E. (5-6, 7,-8, and 9-13).10 Modified Clavien classification system was used for grading postoperative complications and also its relationship with scoring systems was examined.
Statistical analyses were performed with the Statistical Package for the Social Sciences, version 21. Categorical data were presented as numbers and percentages. Continuous data that did and did not conform to normal distribution were presented as mean ± S.D and median (IQR: 25th-75th percentile)”. The independent t-test was used to compare two independent data with normal distribution, while the Mann-Whitney U-test was conducted for data that were not normally distributed. Pearson’s Chi-square, likelihood ratio or Fisher’s exact test was used to compare categorical data. Correlation analyses were undertaken using Spearmen’s correlation coefficient (r). The multivariate logistic regression analysis was used to evaluate the factors associated with SFS and complication development. Receiver operating characteristic (ROC) curves were applied to analyse the predictive ability of the three scoring systems on SFS and complications. A p value of <0.05 was considered statistically significant.
RESULTS
A total of 147 patients, who met the inclusion criteria, were included in the study. The median age of the patients, was 67 (65-71) years. The stone-free rate was found to be 76.0%. The comparison of the demographic and perioperative characteristics of the patients according to SFS, is given in Table I.
Stone size, OT, FT, and LOS were found to be significantly lower in the stone-free group. Three scoring systems were found to be significantly associated with SFS. A statistically significant correlation was found between all three scoring systems and SFS (r=-0.544, r=-0.394 and r=0.451 all p<0.001 for Guy’s SS, S.T.O.N.E., CROES, respectively).
Table I: Comparison of the patient characteristics according to postoperative stone-free status.|
Variables |
Stone free (n=111) |
Not stone free (n=35) |
p-value |
|
Age, years |
67 (65-71) |
68 (65.8-72) |
0.680 |
|
Gender, n (%) Female Male |
51 (45.9) 60 (54.1) |
11 (31.4) 24 (68.6) |
0.130@ |
|
BMI, kg/m2 |
26.1 (23.4-29.4) |
27.6 (24-31.1) |
0.931 |
|
Metabolic syndrome, n (%) |
32 (28.8) |
10 (28.6) |
0.977@ |
|
Comorbidities, n (%) Diabetes mellitus Hypertension Chronic kidney disease |
26 (23.4) 44 (39.6) 7 (6.3) |
11 (31.4) 15 (42.9) 2 (5.7) |
0.342@ 0.735@ >0.999^ |
|
Previous history of ESWL, n (%) Ipsilateral surgery, n (%) |
18 (16.2) 26 (23.4) |
3 (8.6) 11 (31.4) |
0.261@ 0.342@ |
|
ASA category, n (%) ASA I ASA II ASA III |
3 (2.7) 72 (64.9) 36 (32.4) |
1 (2.9) 21 (60.0) 13 (37.1) |
0.872¥ |
|
Side, n(%) Right Left |
53 (47.7) 58 (52.3) |
17 (48.6) 18 (51.4) |
0.932@ |
|
Stone location, n (%)* |
|
|
<0.001@ |
|
Pelvis Single calyx Pelvis + one calyx Multiple calyx Partial staghorn Staghorn |
42 (37.8)b 20 (18.0) b 29 (26.1)a 4 (3.6) a 14 (12.6) b 2 (1.8) b |
2 (5.7) a 1 (2.9) a 4 (11.4) a 3 (8.6) a 19 (54.3) a 6 (17.1) a |
|
|
Stone density, HU |
930.8 ± 336.7 |
1065.4 ± 298.4 |
0.036 |
|
Stone size, mm2 |
266.9 (196.3-447.5) |
643.7 (447.5-1118.6) |
<0.001 |
|
Operation time, min |
90 (75-110) |
120 (90-165) |
<0.001 |
|
Fluoroscopy time, sec |
54 (33-77) |
72.5 (39.3-108.3) |
0.032 |
|
Length of hospital stay, days |
4 (3-4) |
4 (3-7) |
0.012 |
|
Nephrostomy removal time, days |
2 (2-3) |
3 (2.8-3) |
0.083 |
|
Complication rates, n(%) |
25 (22.5) |
14 (40.0) |
0.042@ |
|
Guy’s stone score |
2 (1-2) |
3 (2-3) |
<0.001 |
|
S.T.O.N.E. score |
7 (6-8) |
9 (8-10.3) |
<0.001 |
|
CROES score |
244 (176-279) |
153 (130.1-175.9) |
<0.001 |
|
^Fisher’s Exact test; ¥Likelihood ratio; @Pearson Chi-square; *Each superscript letter denotes a subset of PNL and RIRS categories whose column proportions do not differ significantly from each other at the 0.05 level. |
|||
Complications developed in 27.2% of the patients. The comparison of the demographic and perioperative characteristics of the patients according to the development of complications is presented in Table II. Complication development was found to be associated with all three scoring systems. Each scoring system was found to correlate with the development of complications (r=0.234 p=0.004, r=0.196 p=0.017 and r=-0.247 p=0.003 for Guy’s SS, S.T.O.N.E., CROES, respectively).
A significant positive correlation was observed between Guy’s SS and OT, LOS, FT and BTR (r=0.430 p<0.001, r=0.276 p=0.001, r=0.181 p=0.029 and r=0.194 p=0.019, respectively). While the S.T.O.N.E. scoring system had a significant positive correlation with OT, LOS, and BTR (r=0.323 p<0.001, r=0.217 p=0.009 and r=0.176 p=0.033, respectively), it had no correlation with FT. A significant negative correlation was determined between the CROES nomogram and OT, LOS, and BTR (r=-0.498 p<0.001, r=-0.328 p<0.001 and r=-0.181 p=0.029, respectively). CROES nomogram had the best correlation with OT and LOS, Guy’s SS had the best correlation with BTR (r=0.194).
The results of the multivariate logistic regression analysis of factors associated with SFS and complication development are shown in Table III. For SFS, the Guy’s SS (OR=0.213, p=0.005) and S.T.O.N.E. (OR=0.601, p=0.042) scores were determined as independent markers. None of the three scoring systems were found to be an independent marker for the development of complications, and only DM was identified as an independent marker for complication development (OR=2.375, p=0.045).
Table II: Comparison of the patient characteristics according to postoperative complication development.|
Variables |
Complication present (n = 40) |
No complication (n = 107) |
p-value |
|
Age, years, median (IQR) |
68 (65-72) |
67 (66-71) |
0.751 |
|
Gender, n (%) Female Male |
17 (42.5) 23 (57.5) |
46 (43.0) 61 (57.0) |
0.957@ |
|
BMI, kg/m2, median (IQR) |
27.2 (23.3-31.1) |
27.3 (24.2-29.4) |
0.456 |
|
Metabolic syndrome, n (%) |
15 (37.5) |
28 (26.2) |
0.179@ |
|
Comorbidities, n (%) Diabetes mellitus Hypertension Chronic kidney disease |
16 (40.0) 19 (47.5) 4 (10.0) |
21 (19.6) 40 (37.4) 5 (4.7) |
0.011@ 0.265@ 0.255^ |
|
Previous history of ESWL, n (%) Ipsilateral surgery, n (%) |
5 (12.5) 12 (30.0) |
16 (15.0) 25 (23.4) |
0.705@ 0.409@ |
|
ASA Category, n(%) ASA I ASA II ASA III |
1 (2.5) 21 (52.5) 18 (45.0) |
3 (2.8) 73 (68.2) 31 (29.0) |
0.193¥ |
|
Solitary kidney, n(%) |
2 (5.0) |
5 (4.7) |
>0.999^ |
|
Abnormal renal anatomy, n(%) |
3 (7.5) |
4 (3.7) |
0.390^ |
|
Side, n(%) Left Right |
21 (52.5) 19 (47.5) |
56 (52.3) 51 (47.7) |
0.986@ |
|
Stone location, n(%)* |
|
|
0.001¥ |
|
Pelvis Single calyx Pelvis + one calyx Multiple calyx Partial staghorn Staghorn |
9 (22.5)a 1 (2.5)b 12 (30.0) a 0 (0.0) a 15 (37.5)b 3 (7.5) a |
36 (33.6) a 20 (18.7) a 21 (19.6) a 7 (6.5) a 18 (16.8)a 5 (4.7) a |
|
|
Puncture level, n(%) |
|
|
0.571@ |
|
Intercostal |
17 (42.5) |
40 (37.4) |
|
|
Subcostal |
23 (57.5) |
67 (62.6) |
|
|
Number of accesses, n (%) |
|
|
0.132^ |
|
Single |
34 (87.2) |
102 (95.3) |
|
|
Multiple |
5 (12.8) |
5 (4.7) |
|
|
Stone density, HU |
1100 (875-1200) |
900 (743-1200) |
0.080 |
|
Stone size, mm2 |
467 (235.5-739.9) |
298.3 (204.1-588.8) |
0.159 |
|
Operation time, min |
100 (78.8-130) |
90 (75-120) |
0.100 |
|
Fluoroscopy time, sec |
77.5 (39.8-102.5) |
54 (33-77) |
0.007 |
|
Length of hospital stay, days |
6 (4-7) |
3 (2-4) |
0.002 |
|
Nephrostomy removal time, days |
3 (2-3) |
2 (2-3) |
0.002 |
|
Guy’s stone score |
2 (2-3) |
2 (1-2) |
0.020 |
|
S.T.O.N.E. score |
8 (7-9) |
7 (6-8) |
0.009 |
|
CROES score |
172 (142-198.5) |
241 (169-277) |
0.035 |
|
@Pearson Chi-square; ¥Likelihood ratio; ^Fisher’s exact test; *Each superscript letter denotes a subset of PNL and RIRS categories whose column proportions do not differ significantly from each other at the 0.05 level. |
|||
The predictive ability of the three scoring systems for SFS and complication development was evaluated by the ROC analysis (Figures 1 and 2). The area under the curve (AUC) values were calculated as 0.848 for Guy’s SS, 0.813 for S.T.O.N.E., and 0.787 for CROES, at asymptotic significance of <0.001 for each system. The three scores had comparable predictive accuracy for SFS. The three scores had comparable predictive accuracy for SFS. In predicting complication development, the AUC values of the Guy’s SS, S.T.O.N.E. and CROES scores were 0.643, 0.652, and 0.650, with p values of 0.008, 0.005, and 0.005, respectively. The three scoring systems had similarly poor predictive ability in terms of complication development.
Table III: Multivariate logistic regression analysis of independent predictors for postoperative stone-free status and complications.|
Variables |
OR |
95% CI |
p-value |
|
Stone-free status |
|||
|
Stone size |
1.000 |
0.998-1.001 |
0.448 |
|
Partial/complete Staghorn |
0.620 |
0.128-3.009 |
0.553 |
|
Guy’s stone score |
0.213 |
0.073-0.622 |
0.005 |
|
CROES score |
0.418 |
0.160-1.095 |
0.076 |
|
S.T.O.N.E. score |
0.601 |
0.368-0.982 |
0.042 |
|
Complications |
|||
|
Diabetes mellitus |
2.375 |
1.018-5.542 |
0.045 |
|
Partial Staghorn |
1.439 |
0.370-5.599 |
0.600 |
|
Guy’s stone score |
1.071 |
0.443-2.588 |
0.879 |
|
CROES score |
0.754 |
0.348-1.632 |
0.473 |
|
S.T.O.N.E. score |
1.035 |
0.729-1.469 |
0.849 |
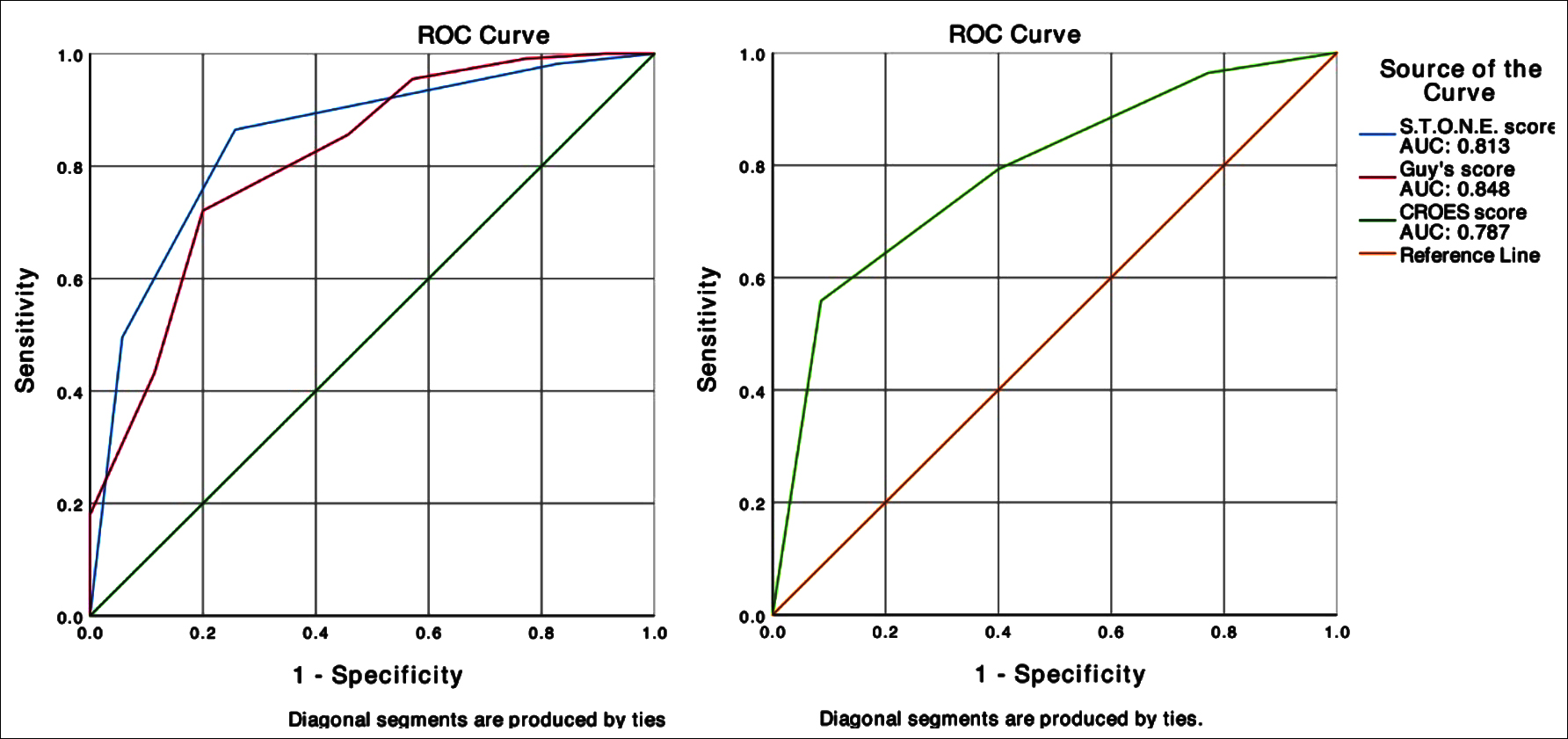 Figure 1: ROC curves and AUC values for the Guy’s SS, S.T.O.N.E., and CROES scoring systems in predicting stone-free status.
Figure 1: ROC curves and AUC values for the Guy’s SS, S.T.O.N.E., and CROES scoring systems in predicting stone-free status.
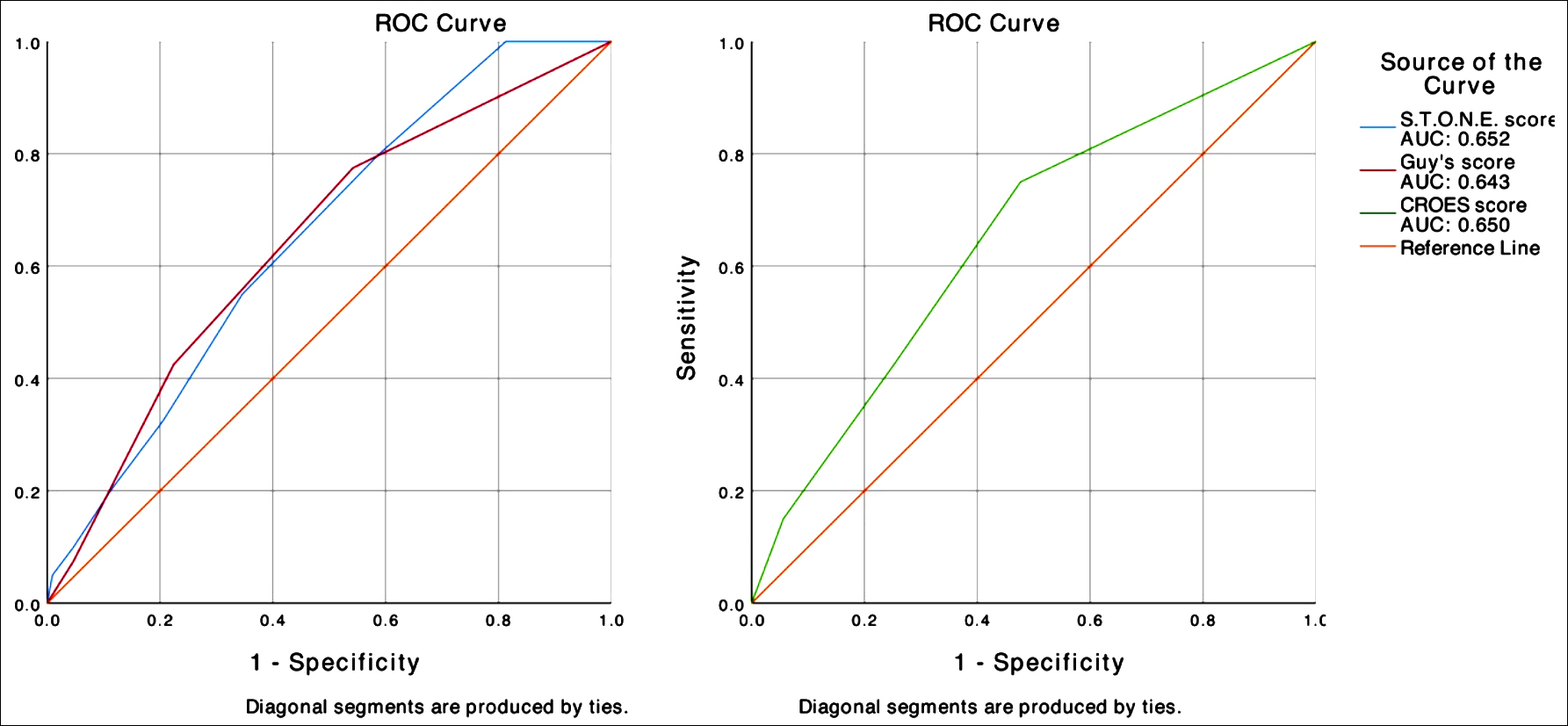 Figure 2: ROC curves and AUC values for the Guy’s SS, S.T.O.N.E., and CROES scoring systems in predicting complication development.
Figure 2: ROC curves and AUC values for the Guy’s SS, S.T.O.N.E., and CROES scoring systems in predicting complication development.
DISCUSSION
The main concern of urologists in the treatment of large or complex renal stones is the development of postoperative complications and the need for re-intervention, when SFS is not achieved. Both situations pose a risk, especially for elderly patients. The incidence of comorbidities increases with age. It has been reported that 65-88% of patients over 60 years have at least one comorbid disease, such as hypertension, diabetes mellitus, and chronic obstructive pulmonary disorder.3 Many studies have shown an association between comorbidities and the development of complications after PCNL.11,12
Although similar PCNL outcomes are reported in different age groups in the literature, bleeding requiring a large volume of transfusion, high complication rates, and high Clavien-grading complications have been reported in elderly patients.11,13,14 In brief, it is important to predict the success of PCNL and perioperative outcomes when planning this surgery in elderly patients.
Several scoring systems have been developed to define the complex structure of stones and predict PCNL outcomes. The most known scoring systems are Guy’s SS, S.T.O.N.E nephrolithometry, and CROES nomogram.5-7 External validation studies and paired and triple comparison studies of these scoring systems have been undertaken. The first of these studies belongs to Labadie et al., who compared the Guy’s SS, S.T.O.N.E. and CROES scoring systems in 246 patients and reported that all three systems predicted SFS at equivalent capacity.10 Similarly, in a study evaluating 586 patients, Tailly et al. reported that the Guy’s SS, S.T.O.N.E. and CROES scoring systems had the ability to predict SFS.15 In a prospective study including 162 patients, Al Adl et al. reported that the S.T.O.N.E. and CROES scoring systems were comparable in predicting SFS, but the latter had a better correlation with SFS.16 In the present study, the stone-free rate was found to be 76.0%, consistent with the literature. All three scoring systems were able to strongly predict SFS. Stone location and size were found to be associated with SFS, while the multivariate analysis revealed only STONE and Guy’s SS as independent predictors for the prediction of SFS.
Studies evaluating the relationship between scoring systems and development of complications and perioperative outcomes (OT, FT, BTR, and LOS) are limited. While Labadie et al. found Guy’s SS and S.T.O.N.E. to be associated with estimated blood loss (EBL) and LOS, CROES did not have a correlation with these parameters.10 In a study including 185 patients, Noureldin et al. reported that Guy’s SS and CROES were associated with OT, LOS, and EBL but had no relation with complications.17 Kumar et al. stated that there was a weak relationship between CROES and Guy’s SS and the development of complications, but these systems did not have any predictive value in the multivariate analysis. In the same study, a significant correlation was observed only between Guy’s SS and OT.18 In another prospective study, Guy’s SS, S.T.O.N.E. and CROES were found to be correlated with the development of complications (p<0.001 for all). While all three scoring systems were correlated with EBL, OT, and FT, they did not have a correlation with LOS.16 In this study, all three scoring systems were correlated with OT, LOS and BTR, but only Guy’s SS was correlated with FT. It is observed that all three systems were associated with the development of complications, but they had weak predictive value. In the literature, conflicting results regarding the development of complications have been reported. In studies that detected a relationship between scoring systems and development of complications tend to have prospective methodologies. Considering the Clavien grade distribution of the prospective and retrospective studies, the greatest difference results from Grade 1 and Grade 2 complications. It is considered that in retrospective studies, low-grade complications may be overlooked, which can lead to the misinterpretation of the predictive ability of scoring systems. The data were recorded prospectively, and a statistically significant correlation was found between the development of complications and scoring systems.
In this study, only diabetes mellitus was found to be an independent marker for complications in the multivariate analysis. In the literature, many studies have shown that diabetes mellitus is a risk factor for infective and major complications after PCNL.19,20 Although the mechanism is not yet fully understood, diabetes mellitus is known to be a disease that includes immunosuppression and is characterised by recurrent urinary tract infections.21 Therefore, it would not be unreasonable to consider that diabetic patients, who present with urinary system stone disease may, have higher immunosuppression status. Furthermore, in another study, it was suggested that CD4 + CD28 null T lymphocytes, which are rarely found in healthy individuals and mostly detected in elderly patients, were increased in patients with type 2 diabetes mellitus, which may be responsible for the complications associated with the disease.22
In this study, the ability of the scoring systems to predict SFS was higher than reported in most previous studies. In previous research, the AUC values for SFS prediction were reported to be 0.629-0.785 for Guy’s SS, 0.563-0.838 for S.T.O.N.E., and 0.641-0.858 for CROES.15-17 This suggests that the predictive value of these scoring systems may be high in elderly patients. However, we think that the methodological differences between the studies, experience of the surgeon, and number of patients may also play a role in these differences.
Tailly et al. defined clinically insignificant stone size as 2 mm or less. This situation decreases the stone-free rate, especially in stones with low complexity, thereby reducing the predictive ability of scoring systems. In this study, the SFS rates were 96.5%, 92.3%, and 95.4% for Guy’s SS (Grade1), S.T.O.N.E. (scores 5-6), and CROES (Grade 4), respectively; while these rates were reported to be 80.3%, 82.1%, and 84.2%, respectively in the study of Tailly et al.15 Another difference in the AUC values can be due to the surgeon’s approach to elderly patients. In order not to prolong OT in more complex stones with a high stone burden, ensuring complete SFS can be pushed into the background. This can increase the predictive value of scoring systems by increasing the possibility of residual stones in cases with high complexity.
This study is the first to examine the predictive ability of the Guy’s SS, S.T.O.N.E., CROES scoring systems for PCNL outcomes in elderly patients.
The limitations of this study include its retrospective nature and the absence of the evaluation of inter-rater variability.
CONCLUSION
This study showed that the Guy’s SS and S.T.O.N.E. scoring systems were effective and reliable in predicting SFS in patients aged 65 years and over. However, the CROES scoring system was not found to be adequate in predicting SFS. All three scoring systems had poor predictive value for the development of complications and were not efficient and reliable in relation to this outcome. The finding of this study, revealing a relationship between diabetes mellitus and the development of complications, is important in terms of guiding the development of future scoring systems.
ETHICAL APPROVAL:
This study follows the principles of the Declaration of Helsinki; and it was approved by the Ethics Committee of Amasya University. (Ethic Board Meeting/Decision No. 1/12.21).
PATIENTS’ CONSENT:
Informed consent was not obtained due to the retrospective nature of the study design.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS' CONTRIBUTION:
SP: Study conception and design, analysis and interpretation of data, wrote the paper.
SY: Study conception and design, wrote the paper.
OK: Acquisition of data, analysis and interpretation of data.
MS: Acquisition of data, critical revision.
ES: Analysis and interpretation of data, statistical analysis.
İHB: Wrote the paper, critical revision.
TD: Analysis and interpretation of data, critical revision.
REFERENCES
- de la Rosette J, Assimos D, Desai M, Gutierrez J, Lingeman J, Scarpa R, et al. CROES PCNL study group. The clinical research office of the endourological society percutaneous nephrolithotomy global study: İndications, complications, and outcomes in 5803 patients. J Endourol 2011; 25(1):11-7. Doı: 10.1089/end.2010.0424.
- Kuzgunbay B, Turunc T, Yaycioglu O, Kayis AA, Gul U, Egilmez T, et al. Percutaneous nephrolithotomy for staghorn kidney stones in elderly patients. Int Urol Nephrol 2011; 43(3):639-43. Doı: 10.1007/s11255-010-9885-6.
- Buldu I, Tepeler A, Karatag T, Bodakci MN, Hatipoglu NK, Penbegul N, et al. Does aging affect the outcome of percutaneous nephrolithotomy? Urolithiasis 2015; 43(2): 183-7. Doı: 10.1007/s00240-014-0742-4.
- Resorlu B, Diri A, Atmaca AF, Tuygun C, Oztuna D, Bozkurt OF, et al. Can we avoid percutaneous nephrolithotomy in high-risk elderly patients using the Charlson comorbidity index? Urology 2012;79(5):1042-7. Doı: 10.1016/j.urology. 2011.10.060.
- Thomas K, Smith NC, Hegarty N, Glass JM. The Guy's stone score--grading the complexity of percutaneous nephrolithotomy procedures. Urology 2011; 78(2): 277-81. Doı: 10. 1016/j.urology.2010.12.026.
- Okhunov Z, Friedlander JI, George AK, Duty BD, Moreira DM, Srinivasan AK, et al. S.T.O.N.E. nephrolithometry: Novel surgical classification system for kidney calculi. Urology 2013; 81(6):1154-9. Doı: 10.1016/j.urology.2012. 10.083.
- Smith A, Averch TD, Shahrour K, Opondo D, Daels FP, Labate G, et al. CROES PCNL Study Group. A nephro-lithometric nomogram to predict treatment success of percutaneous nephrolithotomy. J Urol 2013;190(1):149-56. Doı: 10.1016/j.juro.2013.01.047.
- Tiselius HG, Andersson A. Stone burden in an average Swedish population of stone formers requiring active stone removal: How can the stone size be estimated in the clinical routine? Eur Urol 2003;43(3):275-81. Doı: 10.1016/ s0302-2838(03)00006-x.
- Botev R, Mallié JP, Couchoud C, Schück O, Fauvel JP, Wetzels JF, et al. Estimating glomerular filtration rate: Cockcroft-Gault and Modification of Diet in Renal Disease formulas compared to renal inulin clearance. Clin J Am Soc Nephrol 2009;4(5):899-906. Doı: 10.2215/CJN.05371008.
- Labadie K, Okhunov Z, Akhavein A, Moreira DM, Moreno-Palacios J, Del Junco M, et al. Evaluation and comparison of urolithiasis scoring systems used in percutaneous kidney stone surgery. J Urol 2015;193(1):154-9. Doı: 10.1016/ j.juro.2014.07.104.
- Unsal A, Resorlu B, Atmaca AF, Diri A, Goktug HN, Can CE, et al. Prediction of morbidity and mortality after percutaneous nephrolithotomy by using the Charlson Comorbidity Index. Urology 2012;79(1):55-60. Doı: 10.1016/j.urology.2011.06.038.
- Tseng JS, Lin WR, Sun J, Lin TF, Tsai WK, Chiang PK, et al. Predicting percutaneous nephrolithotomy outcomes and complications in elderly patients using guy's scoring system and charlson comorbidity ındex. Int J Gerontology 2018; 12(3):239-43. Doı: 10.1016/j.ijge.2018.05.001.
- Abedali ZA, Large T, Heiman JM, Bandali E, Anderson BB, Lingeman JE, et al. Percutaneous Nephrolithotomy in the 80 Years of Age and Older Population. Urology 2019; 134:62-65. Doı: 10.1016/j.urology.2019.08.044.
- Okeke Z, Smith AD, Labate G, D'Addessi A, Venkatesh R, Assimos D, et al. CROES PCNL Study Group. Prospective comparison of outcomes of percutaneous nephrolithotomy in elderly patients versus younger patients. J Endourol 2012; 26(8):996-1001. Doı: 10.1089/end.2012.0046.
- Tailly TO, Okhunov Z, Nadeau BR, Huynh MJ, Labadie K, Akhavein A, et al. Multicenter external validation and comparison of stone scoring systems in predicting outcomes after percutaneous nephrolithotomy. J Endourol 2016; 30(5):594-601. Doı: 10.1089/end.2015.0700.
- Al Adl AM, Mohey A, Abdel Aal A, Abu-Elnasr HAF, El Karamany T, Noureldin YA. Percutaneous nephrolithotomy outcomes based on S.T.O.N.E., GUY, CROES, and S-ReSC scoring systems: The first prospective study. J Endourol 2020; 34(12):1223-8. Doı: 10.1089/end.2019.0856.
- Noureldin YA, Elkoushy MA, Andonian S. Which is better? Guy's versus S.T.O.N.E. nephrolithometry scoring systems in predicting stone-free status post-percutaneous nephrolithotomy. World J Urol 2015; 33(11):1821-5. Doı: 10.1007/ s00345-015-1508-5.
- Kumar S, Sreenivas J, Karthikeyan VS, Mallya A, Keshavamurthy R. Evaluation of CROES nephrolithometry nomogram as a preoperative predictive system for percutaneous nephrolithotomy outcomes. J Endourol 2016; 30(10): 1079-83. Doı: 10.1089/end.2016.0340.
- Olvera-Posada D, Tailly T, Alenezi H, Violette PD, Nott L, Denstedt JD, et al. Risk factors for postoperative complications of percutaneous nephrolithotomy at a tertiary referral center. J Urol 2015; 194(6):1646-51. Doı: 10.1016/j.juro. 2015. 06.095.
- Lorenzo Soriano L, Ordaz Jurado DG, Pérez Ardavín J, Budía Alba A, Bahílo Mateu P, Trassierra Villa M, et al. Predictive factors of infectious complications in the postoperative of percutaneous nephrolithotomy. Actas Urol Esp 2019; 43(3):131-6. Doı: 10.1016/j.acuro.2018.05.009.
- Ronald A, Ludwig E. Urinary tract infections in adults with diabetes. Int J Antimicrob Agents 2001; 17(4):287-92. Doı: 10.1016/s0924-8579(00)00356-3.
- Giubilato S, Liuzzo G, Brugaletta S, Pitocco D, Graziani F, Smaldone C, et al. Expansion of CD4+CD28null T-lymphocytes in diabetic patients: exploring new pathogenetic mechanisms of increased cardiovascular risk in diabetes mellitus. Eur Heart J 2011; 32(10):1214-26. Doı: 10.1093/eurheartj/ehq499.