Assessing the Adherence of Operative Notes for Laparoscopic Appendectomy with the Royal College of Surgeons Guidelines
By Fatima Mannan, Roger Christopher Gill, Abdul Ahad Sohail, Rehman AlviAffiliations
doi: 10.29271/jcpsp.2021.02.202ABSTRACT
Objective: To determine the frequency of adherence of laparoscopic appendectomy operative notes with the Royal College of Surgeons (RCS) guidelines at the tertiary care centre.
Study Design: A clinical audit report.
Place and Duration of Study: The Aga Khan University Hospital, Karachi between January and June 2018.
Methodology: Operative notes of laparoscopic appendectomy, written by residents of general surgery from trainee levels R1 to R5 during the study period, were included in the study. Each component from RCS guidelines, was assessed. The response to every question in proforma was marked either as Y=Yes or N=No. Overall score of more than 70% was chosen arbitrarily as a qualifying standard for an adequate operative note. Data were analysed by using SPSS (version 21). A p-value of <0.05 was considered significant.
Results: A total of 74 operative notes relating to laparoscopic appendectomy were reviewed during the study period. Most of these, i.e. 46% notes, were written by year one residents; 47.1% operative notes showed adequacy of practice in concordance with RCS guidelines. The most lacking component in operative notes was mentioning of the operative time, port sites, intraoperative complications and details of specimen removed. Stratified analysis of operative notes did not reveal any association between age, gender and level of training of residents to affect the adequacy of operative note documentation.
Conclusion: Only a quarter of the studied documentation fulfilled the criteria for adequacy of practice. Residents need to be educated and familiarised with these guidelines to improve documentation of operative procedures. Strategies need to be formulated and tested to improve the performance.
Key Words: Operative notes, Good medical practice, Acute appendicitis, Laparoscopic appendectomy, RCS guidelines.
INTRODUCTION
Operative notes in essence are one of the most essential components of good surgical practice. It forms an important record of intervention performed on the patient with its medico-legal implications.1 These notes are formulated as soon as the procedure is carried out, making sure a complete record of procedure, including events are recorded in a timely manner by a competent member of the surgical team, avoiding any recall error. Proper documentation of these notes ensures that the patient’s continuity of care is maintained and quality of care is enhanced, which may also have an impact on postoperative and future management of the patient. The same document may hold potential for future research endeavours, as it holds essential data.2
Hence, writing good quality operative notes could achieve multiple purposes, further enhancing its value.3,4
Operative notes are very important for academic learning residents; and are considered an essential source for the surgical training and education.5-8 In Pakistan, it is very unfortunate that the majority of residency training programmes offer no teaching in this important skill. Similar trends have been observed internationally, especially, amongst the general surgery residents; and some evidence exists that training them in this regards would be beneficial.9 Evidence exist that educating surgeons has revealed improvements in operative note documentation.10
The objective of this study was the comparison of operative notes to the international standards, set by the Royal College of Surgeons of England (Table I), identifying the deficiencies and suggesting measures to help improve this aspect of training. The results of this study may help researchers formulate strategies and guidelines, which may be implemented in the residency programmes throughout Pakistan.
METHODOLOGY
This was a cross-sectional study, conducted at the Department of Surgery, The Aga Khan University Hospital, Karachi from January to June 2018. A non-probability (consecutive) sampling technique was used. Operative notes of laparoscopic appendectomy, written by residents of general surgery from trainee levels R1 to R5 during the study period, were included in the study. Illegible notes, notes written by consultants, house officers, paramedical staff and operative notes of patients with conversion or open appendectomy procedures, were excluded from the study. The study was conducted after approval from the Ethics Review Committee of the University.
At Aga Khan University Hospital, operative notes for all procedures are conventionally written on a sheet of paper attached in a confidential file. These operative notes were reviewed prospectively and data was collected on a daily basis by the primary investigator. A predesigned proforma was used to collect the data prospectively from the files of patients, who underwent laparoscopic appendectomy.
Each component from RCS guideline, as shown in Table I, was assessed. The response to every question in proforma was marked either, Y=Yes or N=No. Overall score of more than 70% was chosen arbitrarily as a qualifying standard for an adequate operative note.
As there is no local data available regarding assessment of quality of operative notes, one of the most recent international studies done in this regard was selected, which showed the concordance rates, ranging from 36% to 100% (17) and considered the mean that is 68%. Of all the components analysed, intraoperative complications was taken as a significant variable with a concordance rate, i.e. 68%, to calculate the sample size. Sample size was measured by using open EPI software with a confidence level of 95%, precision of 12%, and anticipated population proportion of 68% (17). The measured sample size came out to be 60 procedures.
Data were analysed by using SPSS (version 21). Descriptive analysis of continuous variables (age of resident writing the operative notes) along with overall score of operative notes was described by mean ± SD. Frequency of adequate practice was evaluated for each applicable component by calculating the percentages of marked components as per RCS guidelines. Stratified analysis was done for effect modifiers, i.e. age, gender and year of resident, writing the operative note, training year of the resident, and case location (day care/in-patients). Post-stratification, Chi-square test, and Fisher’s Exact test was applied and p-value of < 0.05 was considered significant.
RESULTS
A total of 74 operative notes of laparoscopic appendectomy, written by residents, were observed at the Aga Khan University Hospital, Karachi during the study period. Most of the cases, 91.9% (n=68), were in-patients.
The average age of the resident writing the operative notes was 27 ± 1.96 years and the overall average score of the operative notes was 70.20 ± 10.47. Around, 44.59% (n=33) of operative notes were written by male residents and 55.41% (n=41) written by female residents. Almost 45.95% (n=34) of the notes were written by year I residents (Figure 1).
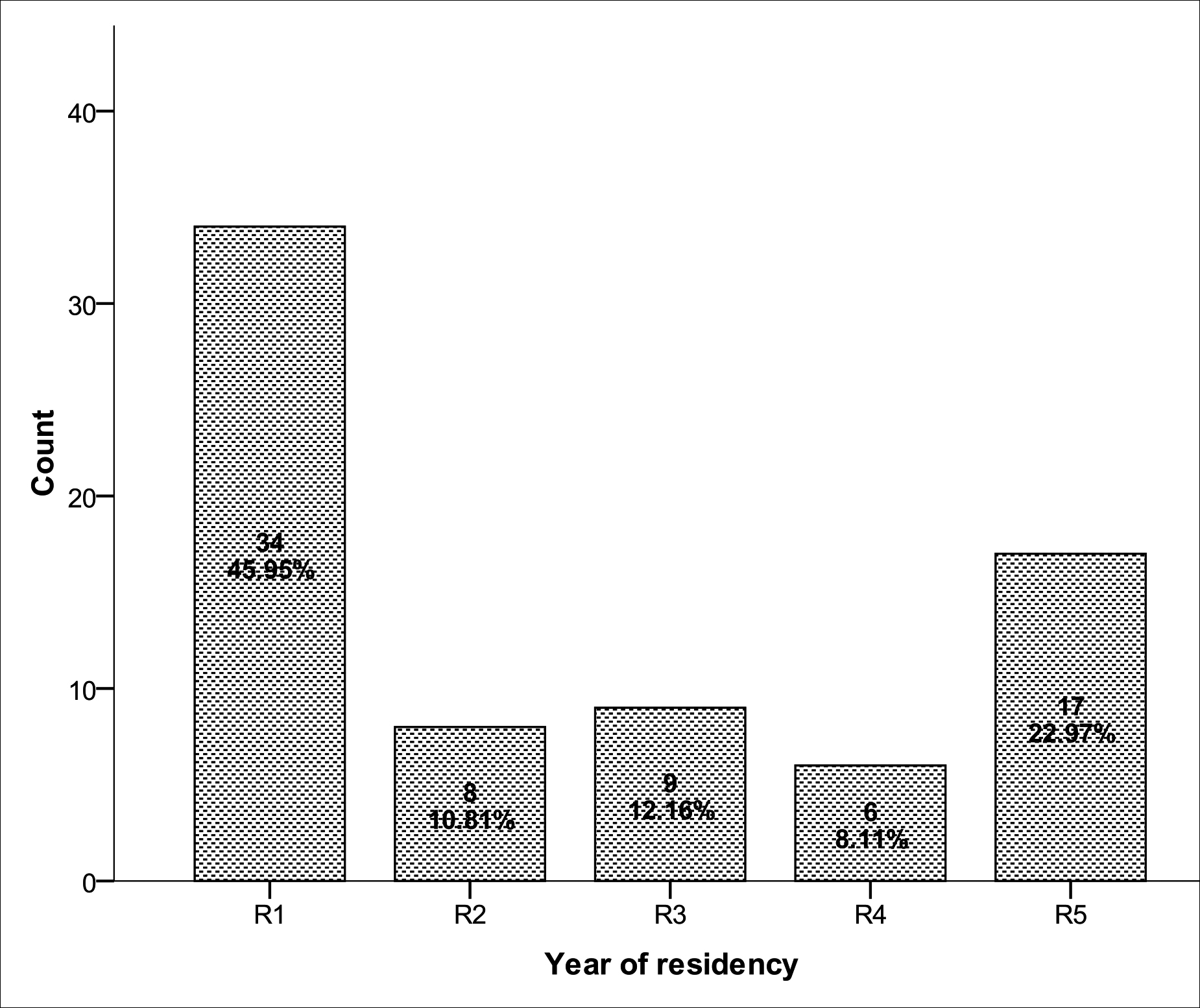 Figure 1: Distribution according to the level of residents who wrote the operative note n= 74.
Figure 1: Distribution according to the level of residents who wrote the operative note n= 74.
Table I: Operative notes components as per RCS guidelines.
|
Good surgical practice components |
Notes |
% |
|
Patient name |
73 |
98.6% |
|
Date of birth |
56 |
75.7% |
|
Hospital number |
74 |
100% |
|
Date of operation |
69 |
93.2% |
|
Time of operation |
9 |
12.2% |
|
Name of the operating surgeon |
74 |
100% |
|
Name of operating assistant |
73 |
98.6% |
|
Name of operation mentioned |
72 |
97.3% |
|
Port sites mentioned |
46 |
62.2% |
|
Operative findings |
74 |
100% |
|
Intraoperative complications |
4 |
5.5% |
|
Any extra procedure performed |
3 |
4.1% |
|
Details of tissue removed |
50 |
67.6% |
|
Details of any fluid aspirated |
15 |
20.3% |
|
Postoperative care instructions mentioned |
45 |
60.8% |
|
Signature of surgeon |
52 |
70.3% |
|
Type of anesthesia |
73 |
98.6% |
|
Duration of surgery mentioned |
0 |
0% |
Out of 74 operative notes, only 48.6% (n=36) were found to be adequate practice (concordance with RCS guidelines); while 51.4% (n=38) inadequate. Components of operative note in terms of percentage are reported in Table II. The most common lacking component were: time of operation, port sites mentioned, intraoperative complications, any extra procedure performed, details of tissue removed, details of any fluid aspirated, postoperative care instructions, signature of surgeon, and duration of surgery.
Table II: Frequency of adherence of laparoscopic appendectomy operative notes with the RCS guidelines.
|
Operative notes |
p-value |
||
|
|
Adequate n=36 |
Inadequate n=38 |
0.337 |
|
Male |
14 (38.9%) |
19 (50%) |
|
|
Female |
22 (61.1%) |
19 (50%) |
|
|
Resident age-group <26 years |
16 (44.4%) |
22 (57.9%) |
0.357
|
|
26-30 |
14 (38.9%) |
9 (23.7%) |
|
|
>30 years |
6 (16.7%) |
7 (18.4%) |
|
|
Case day care In patient |
3 (8.3%) 33 (91.7%) |
3 (7.9%) 35 (92.1%) |
>0.999 |
|
Level of residents R1 – R3 (Junior) R4 – R5 (Senior) |
24 (47.1%) 12 (52.2%) |
27 (52.9%) 11 (47.8%) |
0.684 |
Name of the operating surgeon and operating assistant was mentioned in the above 98.6% (n=73) of the notes. Patient name, date of birth, hospital number, and date of operation were adequately mentioned in the operative notes (Table I).
Stratified analysis was performed, and it was observed that adequate operative notes were evaluated by age groups of resident (p = 0.357), gender of resident (p = 0.337), and day-care and in-patient (p = >0.999); but no significant difference was observed among them in adequate operative notes. However, when compared among level of residents, also no significant difference was found (p = 0.684, Table II).
DISCUSSION
Operative notes are of great importance for all surgical specialties, as they are the only source of information documenting step-by-step events that took place during surgery.1 They also serve as an important medico-legal document, and can be used in surgeon’s defence in the face of litigation.11 However, studies have shown that only 55 percent of operative notes are useful in the court of law.6 The Royal College of Surgeons of England has introduced guidelines to help surgeons write a complete and concise operative note, which can be used for postoperative management of the patients and early recognition of postoperative complications as well as for medico-legal, research and audit purposes.1,11-13
Studies have shown that operative notes are generally of poor quality with crucial elements of the procedure frequently absent.8 These results are similar to these studies with only 24.32% of the operative notes found to be adequate in accordance to the RCSE guidelines; while 75.58% were inadequate. However some other studies had higher compliance rates such as a study conducted in India by Krishnan et al. on oral and maxillofacial surgery operative notes, which demonstrated that 84.6% of them were in accordance to RCSE guidelines in the initial audit, which significantly improved to 94.8% in the second audit conducted after a 6-month period.14
In this study, the components that are most frequently missing among the inadequate operative notes were the time of operation (mentioned in 12.2% of operative notes), duration of surgery (0%), any extra procedure performed (4.1%), intraoperative complications (5.5%), details of any fluid aspirated (20.3%), postoperative care instructions (60.8%), port sites mentioned (62.2%), details of tissue removed (67.6%) and signature of surgeon (70.3%).
In comparison to this, a recent study conducted by Coughlan et al. on orthopedic operative notes demonstrated similar results with operative diagnosis, postoperative instructions, incision details, prosthesis details, and tourniquet time frequently absent.12
A study conducted by Thompson et al. on operative notes for laparoscopic cholecystectomy after introducing procedure specific proformas based on RCSE guidelines in their institute, showed statistically significant improvement in documentation according to guidelines.13
However, procedure specific proformas for writing operative notes could not be used in this study due to logistic reasons as they need to readily available in all the theatres, where the procedure could be performed.
A recent study conducted by Parwaiz et al. demonstrated that simple interventions in the form of presentations and seminars could lead to statistically significant improvements in documentation of crucial aspects of operative notes. Re-audit after these interventions showed marked improvements; for example, time of surgery (from 4% to 60%), type of procedure (1% to 83%), complications of procedure (67% to 100%), estimated blood loss (2% to 73%) and signature of surgeon (78% to 97%).11 A study by Borchert et al. revealed that 75% of surgical residents have never received any formal training in writing an operative note, and 93% of them believed that it is an important skill that should be formally taught during the surgical training.15
The study conducted by Krishnan et al. showed significant improvements in documentation of the operative notes after introduction of a computerised-based proforma.14 The latest RCSE guidelines recommends that operative notes are preferably typed,12 as this increases the legibility from 66% to 100%, as shown in one study.16 This resolves the problem of poorly legible operative notes decreasing errors in postoperative management of the patient, and improving surgeon’s defence in the event of litigation. If operative note record is electronic and saved on a secured database, then it can become readily accessible to all healthcare professionals. However, this can prove to be a logistic challenge as this requires a computer terminal and access to hospital database, which needs to be available in all theatres where surgery is taking place.
In this study, the junior residents demonstrated better compliance in writing the operative notes with 47.1% of the operative notes being adequate, according to the RCSE guidelines as compared to senior residents with only 52.2 % of the operative notes being adequate. However, this was not seen to be statistically significant. In contrast to this, the study conducted by Thompson et al. demonstrated that operative notes were adherent to the guidelines with increasing seniority of the author.13
The limitations of this study were small sample size and inclusion of only one type of procedure. On the basic of present result, it is recommended that other surgical specialties and procedures be evaluated for adherence to RCSE guidelines; and interventions need to be done such as that has been described above to significantly improve the quality of operative notes, resulting in better patient care outcomes postoperatively.
CONCLUSION
Only a quarter of the studied documentations fulfills the criteria for adequacy of practice according to RCSE guidelines. Residents need to be educated and familiarised with these guidelines to improve documentation of operative procedures. Strategies need to be formulated and tested to improve the performance, such as procedure specific proformas, which can be electronically based and avoid litigation risk in the event of a medico-legal case.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
FM: Contributed to the conception and design of work, analysis and interpretation, drafting of manuscript.
RCG: Contributed to design, analysis, interpretation, critical revision.
AAS: Literature search, conception, design, analysis, drafting of work.
RA: Conception, design, critical revision, final approval.
REFERENCES
- Cutting J, Hossain T, Maude K. Quality of operation note documentation in general surgical patients: Re-audit results. Int J Surg 2014; 12:S50.
- Wauben LSGL, Goossens RHM, Lange JF. Evaluation of operative notes concerning laparoscopic cholecystectomy: Are standards being met? World J Surg 2010; 34(5):903-9.
- C-P D. Crafting the operative note: Techniques critical to success. J Gynecol Tech 1995; 3:119-20.
- Moore RA. The dictated operative note: Important but is it being taught? J Am Coll Surg 2000; 190(5):639-40.
- Eichholz AC, Van Voorhis BJ, Sorosky JI, Smith BJ, Sood AK. Operative note dictation: Should it be taught routinely in residency programs? Obstet & Gynecol 2004; 103(2): 342-6.
- Lefter LP, Walker SR, Dewhurst F, Turner RWL. An audit of operative notes: Facts and ways to improve. ANZ J Surg 2008; 78(9):800-2.
- Porterfield JR, Altom LK, Graham LA, Gray SH, Urist MM, Hawn MT. Descriptive operative reports: Teaching, learning, and milestones to safe surgery. J Surg Educ 2011; 68(6):452-8.
- Edhemovic I, Temple WJ, de Gara CJ, Stuart GCE. The computer synoptic operative report a leap forward in the science of surgery. Ann Surg Oncol 2004; 11(10):941-7.
- Garcia A, Revere L, Sharath S, Kougias P. Implications of clinical documentation (In) accuracy: A pilot study among general surgery residents. Hosp Top 2017; 1-5.
- Singh R, Chauhan R, Anwar S. Improving the quality of general surgical operation notes in accordance with the Royal College of Surgeons guidelines: a prospective completed audit loop study. J Eval Clin Pract 2012; 18(3): 578-80.
- Parwaiz H, Perera R, Creamer J, Macdonald H, Hunter I. Improving documentation in surgical operation notes. Br J Hosp Med 2017; 78(2):104-7.
- Coughlan F, Ellanti P, Ní Fhoghlu C, Moriarity A, Hogan N. Audit of orthopaedic surgical documentation. Surgery research and practice 2015; 2015.
- Thomson DR, Baldwin MJ, Bellini MI, Silva MA. Improving the quality of operative notes for laparoscopic cholecystectomy: Assessing the impact of a standardized operation note proforma. Int J Surg 2016; 27:17-20.
- Krishnan B, Prasad GA, Madhan B. Improving the quality of oral and maxillofacial surgical notes in an indian public sector hospital in accordance with the royal college of surgeons guidelines: A completed audit loop study. J Maxillofacial Oral Surgery 2016; 15(3):315-20.
- Borchert D, Rarshen H, Kemps M, Lavelle M. Operative notes teaching: re-discovery of an effective teaching tool in surgical training. Int J Surg 2006; 8(1):1-11.
- Ghani Y, Thakrar R, Kosuge D, Bates P. Smart’electronic operation notes in surgery: An innovative way to improve patient care. Intern J Sur 2014; 12(1):30-2.