Angioembolisation for the Treatment of Pseudo-aneurysm of Internal Maxillary Artery
By Muhammad Azeemuddin1, Anosha Khan2, Atif Hafeez Siddiqui3, Asad Shakil1, Basit Salam1, Raza Sayani1Affiliations
doi: 10.29271/jcpsp.2021.03.340ABSTRACT
Pseudo-aneurysm of internal maxillary artery, following a road traffic accident, is a rare clinical scenario. The consequence of pseudo-aneurysm may be spontaneous rupture of the arterial wall, which may eventually lead to life-threatening hemorrhage. We report a case of a 20-year male who presented with recurrent epistaxis. CT scan was performed, which revealed a pseudo-aneurysm of the internal maxillary artery; this was successfully treated by angioembolisation. Similar cases of traumatic pseudo-aneurysms have been reported, however, none presented with recurrent epistaxis after management of pan-facial fractures.
Key Words: Epistaxis, Pseudo-aneurysm, Angioembolisation, Pan-facial fracture.
INTRODUCTION
A pseudo-aneurysm, also known as false aneurysm, is a collection of blood that forms between the two outer layers of an artery, the tunica media and the tunica adventitia, due to incomplete rupture of the vessel wall. This eventually leads to formation of a hematoma with the compression of the normal surrounding tissues.
Pseudo-aneurysms can occur throughout the body due to trauma, infection or surgery. However, pseudo-aneurysm of internal maxillary artery (IMA), a branch of the external carotid artery is a rare clinical entity. The management options for pseudoaneurysms include ultrasound-guided compression (USGC), ligation of afferent and efferent vessels, abscission of the pseudo-aneurysm along with stent graft and coil embolisation.1,2 Angioembolisation was the only non-surgical option in our case as digital compression at this site is neither possible nor adequate for its management.
CASE REPORT
A 20-year male was brought to the Emergency Department of our hospital with complaint of recurrent epistaxis. He was previously admitted in another tertiary care hospital about six months back, after a road traffic accident with multiple pan-facial fractures. These were managed via open reduction and internal fixation.
The patient was kept on ventilator for a week after the surgical intervention during that admission.
Since the past four weeks, patient experienced recurrent epistaxis from the left side, which was managed by pinching and nasal packing.
On examination, the patient was stable with no limitation of mouth opening, no facial paralysis and no active bleeding. His blood pressure was 125/78 mm Hg, respiratory rate 20/min, pulse rate 121/min, and temperature 37°C. On rigid nasal endoscopy, clots were seen in the left middle meatus. CT scan head and neck was performed, which revealed a number of comminuted fractures of the posterolateral and anterolateral wall of the left maxillary sinus, left pterygoid plate and the greater wing of the sphenoid on the left. The presence of two pseudo-aneurysms of the left IMA was also confirmed on CT scan.
The patient was then referred to the interventional radiology suite for angioembolisation. Under local anesthesia, right femoral artery was punctured and 4 Fr sheath was placed by Seldinger’s technique. 4 Fr cerebral H1 catheter was used for cannulation of left external carotid artery, where two pseudo-aneurysms were identified arising from the left IMA measuring 23 x 8mm and 6 x 5 mm, respectively. The pseudo-aneurysms were embolised, using a 355-500 micron PVA (Poly Vinyl Alcohol) particles followed by placement of micro-coils 2 mm x 2 cm (Figure 1).
No immediate post-procedural complication was noted and patient was discharged next day with follow-up appointments with maxillofacial and ENT teams.
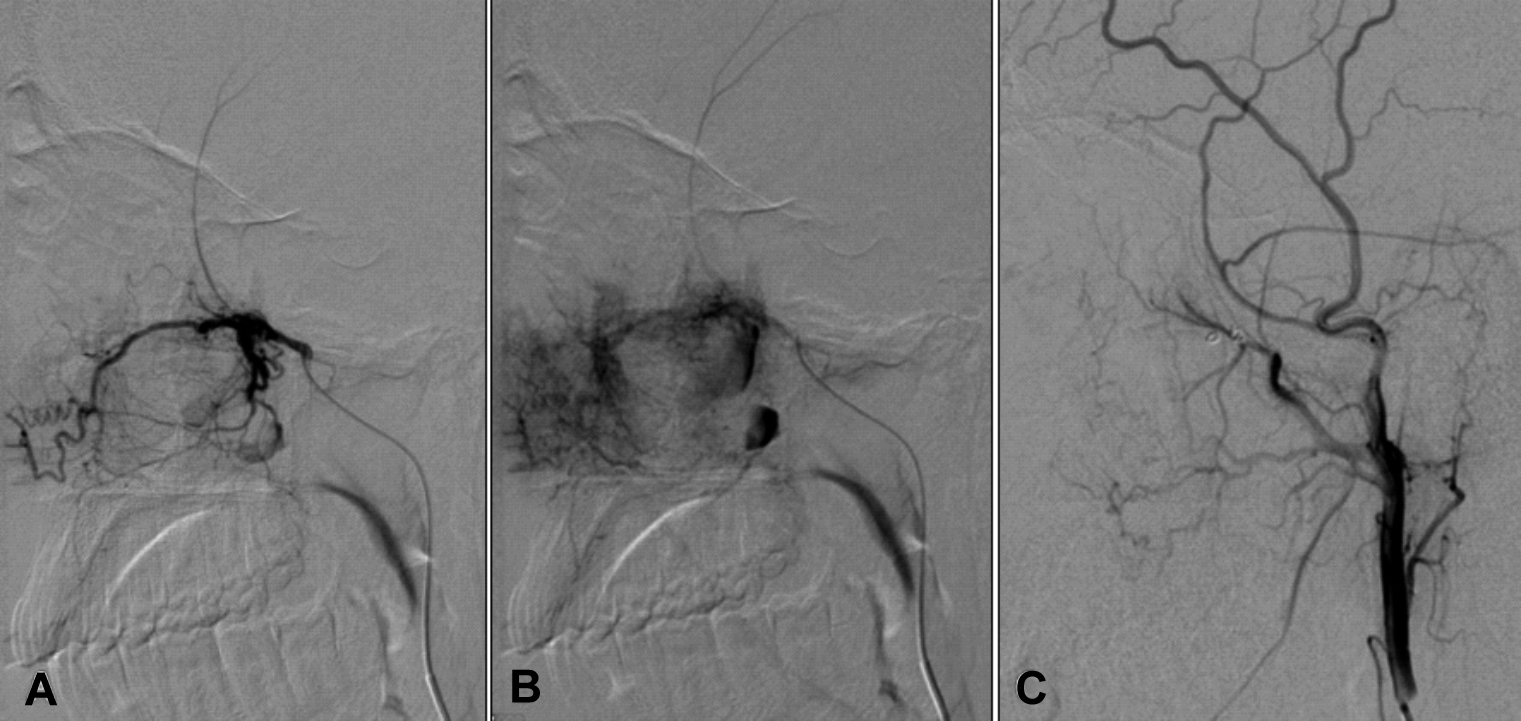 Figure 1: Images from digital subtraction angiography (DSA) of external carotid artery. Arterial phase (A) shows catheter tip in external carotid artery. Delayed phase (B) shows abnormal vascularity and filling of the pseudoaneurysm. Post-embolisation arteriogram (C) shows occlusion of the abnormal vascularity and the pseudoaneurysm.
Figure 1: Images from digital subtraction angiography (DSA) of external carotid artery. Arterial phase (A) shows catheter tip in external carotid artery. Delayed phase (B) shows abnormal vascularity and filling of the pseudoaneurysm. Post-embolisation arteriogram (C) shows occlusion of the abnormal vascularity and the pseudoaneurysm.
DISCUSSION
The IMA is one of the largest terminal branches of the carotid arteries. It runs its way through the maxilla, mandible, cerebral dura mater and nasal cavity. It is divided into three parts; namely, the mandibular part, the pterygoid part and the pterygopalatine part. This relationship explains why IMA is likely to be lacerated highly due to comminuted pan-facial fractures. Furthermore, pseudo-aneurysm can occur as a consequence of other facial fractures, needle aspirations, trauma, and mandibular osteotomies along with infections.3 The comminuted pan-facial fractures can result in the laceration of vessel wall of the IMA. This eventually leads to a formation of pseudo-aneurysm, which is associated with breaching of the vessel wall with blood clots and compression of the surrounding normal tissues. This is a rare but life- threatening entity, and if not treated, can lead to hemorrhage and exsanguination following rupture.4,5
The IMA pseudo-aneurysm presents as epistaxi, pulsatile swelling in the parotid region with facial nerve palsy, along with recurrent bleeding from oral and throat, depending upon the segments of the artery involved. An audible bruit can be heard almost exclusively during systole.6 Most of the instances begin within two months of injury. In our patient, the epistaxis began five months post-trauma. The diagnosis is usually made with CT or MRI; but digital subtraction angiography (DSA) is the imaging modality of choice for diagnosis and management.
Once diagnosed, the pseudo-aneurysm can be managed either surgically or by endovascular approach. Angioembolisation is definitely a safer and minimally invasive technique to perform with reduced risks of bleeding and revascularisation.7,8 Reflux of embolisation material outside the intended area of embolisation may rarely result in complications such as blindness or stroke4 but this is now a rare complication as superselective technique is used utilising microcatheter.
To conclude, formation of pseudoaneurysm of IMA needs urgent management in order to minimise the risk of life-threatening complications. An appropriate multidisciplinary team- approach is required in a tertiary care hospital with availability of interventional radiologists and surgical specialists.
PATIENT'S CONSENT:
Consent was taken from the patient, regarding the procedure as well as using images for publication without name / identity disclosure
CONFLICT OF INTEREST:
Authors declared no conflict of interest.
AUTHORS' CONTRIBUTION:
MA: Conception and design, analysis and revision.
AK: Drafting, analysis and revision.
AHS: Drafting, analysis and revision.
AS, BS, RS: Conception and design, analysis and revision.
REFERENCES
- Kim JH, Jung YJ, Chang CH. Superficial temporal artery pseudoaneurysm treated with manual compression alone. J Cerebrovasc Endovasc Neurosurg. 2015; 17(1):49-53. doi: 10.7461/jcen.2015.17.1.49.
- D'Souza J, Bedi VS, Indrajit IK, Pant R. Non-surgical management of pseudoaneurysms. Med J Armed Forces India 2007; 63(2):115-119. doi:10.1016/S0377-1237(07) 80051-7.
- Chakrabarty S, Majumdar SK, Ghatak A, Bansal A. Management of pseudoaneurysm of internal maxillary artery resulting from trauma. J Maxillofac Oral Surg 2015; 14(Suppl 1):203-8. doi: 10.1007/s12663-012- 0427-x.
- Nastro Siniscalchi E, Catalfamo L, Pitrone A, Papa R, Fama F, Lo Giudice G, et al. Traumatic pseudoaneurysm of the internal maxillary artery: Arare life-threatening hemorr-hage as a complication of maxillofacial fractures. Case Rep Med 2016:9168429. doi.org/10.1155/2016/9168429.
- Pinjala RK, Joshi S, Rammurti S. Traumatic pseudoaneurysm of the internal maxillary artery. EJVES Extra 2007; 14(5):54-55. doi.org/10.1016/j.ejvsextra.2007.08. 003.
- Karanth SK, Jagannathan M, Mahesh SG, Devale M. Internal maxillary artery pseudoaneurysm in a case of mandibular fracture. Indian J Plast Surg 2007; 40(1):51-3.
- Soh HY, Muda AS, Jabar NA, Nordin R, Nabil S, Ramli R. Non-pulsatile traumatic pseudoaneurysm of the internal maxillary artery following trauma to mandible. Oral Maxillofac Surg 2015; 19(4):423-5. doi: 10.1007/s10006- 015-0497-2.
- Wang D, Su L, Han Y, Fan X. Embolisation treatment of pseudoaneurysms originating from the external carotid artery. J Vasc Surg 2015; 61(4):920-6. doi: 10.1016/j.jvs. 2014.10.093.