An Old Enemy: Still Nephrotoxic
By Faruk Recep Ozalp1, Tugba Karadeniz2, Alper Alp3Affiliations
doi: 10.29271/jcpsp.2021.02.228ABSTRACT
Tubulointerstitial nephritis (TIN) presents histopathologically as tubulitis and oedema/inflammation and fibrosis, affecting the renal tubules and interstitium with relative sparing of the glomeruli and vasculature. It can be acute or chronic or acute on chronic and has a wide range of etiologies. In this article, we report a case of a 44-year male who presented with acute TIN, associated with the use of diclofenac at therapeutic doses, that resolved with treatment but later progressed to chronic TIN after the patient resumed diclofenac therapy. The case is discussed in the context of literature regarding the nephrotoxic effects of nonsteroidal anti-inflammatory drugs (NSAIDs).
Key Words: Nonsteroidal anti-inflammatory drugs, Acute kidney injury, Tubulointerstitial nephritis.
INTRODUCTION
Tubulointerstitial nephritis (TIN) is characterised by the coexistence of acute kidney injury (AKI) and infiltration of interstitial areas by inflammatory cells. Known causes of TIN include certain drugs (e.g., nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, tacrolimus, lithium), heavy metals, metabolic diseases, vesicoureteral reflux, sickle cell anaemia, and immune diseases.1 The use of NSAIDs is extremely common in the community and generally unsupervised by physicians. Females, older adults, and patients with underlying chronic kidney disease (CKD), chronic liver diseases, volume depletion, or electrolyte disturbances are prone to the nephrotoxic effects of NSAIDs. Renal biopsy should be performed as soon as possible to establish an early diagnosis and initiate treatment in order to prevent fibrosis and development of CKD.
CASE REPORT
A 44-year male presented with complaints of swelling of the feet and abdomen and reduced urine output. He had no chronic diseases other than a 4-year history of Guillain–Barré syndrome (GBS) and arterial hypertension. He was under long-term treatment with 600 mg gabapentin 3 times a day and 50 mg diclofenac sodium twice a day, due to lower extremity pain associated with GBS, and was also taking 5 mg amlodipine once a day as antihypertensive therapy. He had no history of using herbal or alternative therapies.
On physical examination, his pulse was 76/min and blood pressure was 150/85 mmHg. On respiratory examination, breath sounds were reduced in the middle and lower zones bilaterally. He had bilateral 2+ pretibial oedema. Laboratory findings are summarised in Table I. His creatinine level measured 2 years before presentation to our clinic was 0.8 mg/dL. Ultrasound of the urinary tract showed normal renal dimensions and parenchymal thickness. The patient remained oliguric and had severe refractory metabolic acidosis, so hemodialysis (HD) was initiated. Renal biopsy was performed due to signs of kidney damage of unknown cause and urinalysis results (Figure 1). Acute TIN associated with diclofenac sodium was suspected, based on these findings. Treatment was initiated with methylprednisolone at a dose of 1 mg/Kg/day. After six sessions of HD, follow-up assessment showed improved renal functions and HD was discontinued. On day 10 of steroid therapy, the patient’s creatinine levels had decreased to 2 mg/dL and he was discharged with instructions to use 16 mg methylprednisolone and avoid the use of NSAIDs. Approximately four months after discharge, the patient returned with difficulty in breathing, swelling of the feet, extensive pruritus, and poor general condition. It was learned that he had appeared for follow-up only once since being discharged from the hospital and had continued using diclofenac despite being cautioned against it. On physical examination, his pulse was 82/min and blood pressure was 144/80 mmHg. On auscultation, breath sounds were reduced in the middle and lower zones and there were sporadic course rales. He had bilateral 2+ pretibial oedema. Laboratory findings are summarised in Table I. Urinary tract ultrasound showed normal renal dimensions and parenchymal thickness. No stones or hydronephrosis were detected. HD was initiated again due to severe metabolic acidosis and oliguria. Renal biopsy was also repeated due to his progressive decline in renal function and to rule out other renal disorders that may be seen in patients with chronic NSAID use, such as membranous glomerulopathy and acute tubular necrosis (Figure 2).
Table I: The patient’s biochemical results at both admissions.|
First admission |
Second admission |
||
|
Urea |
161 mg/dl |
Urea |
121 mg/dl |
|
Creatinine |
5,2 mg/dl |
Creatinine |
9 mg/dl |
|
GFR |
12,87 ml/min/1,73 m2 |
GFR |
6,83 ml/min/1.73 m2 |
|
Sodium |
133 mmol/L |
Sodium |
142 mmol/L |
|
Potassium |
4,5 mmol/L |
Potassium |
6,3 mmol/L |
|
Calcium |
9,1 mg/dl |
Calcium |
8,8 mg/dl |
|
Phosphorus |
6,5 mg/dl |
Phosphorus |
6,4 mg/dl |
|
pH |
7.25 |
pH |
7,29 |
|
HCO3 |
13,5 mmol/L |
HCO3 |
16,8 mmol/L |
|
24 h urinary protein |
2,5 gr/day |
24 h urinary protein |
3,9 gr/day |
|
WBC |
7500 |
WBC |
8300 |
|
Hemoglobin |
12 gr/dl |
Hemoglobin |
11,2 gr/dl |
|
Platelet |
250000 |
Platelet |
178000 |
|
Albumin |
2 gr/dl |
Albumin |
3 gr/dl |
|
Anti HCV |
Negative |
Anti HCV |
Negative |
|
HBsAg |
Negative |
HBsAg |
Negative |
|
Anti HIV |
Negative |
Anti HIV |
Negative |
|
Urinalysis |
Ery +3, prot +3 |
p-ANCA |
Negative |
|
p-ANCA |
Negative |
c-ANCA |
Negative |
|
c-ANCA |
Negative |
ANA |
Negative |
|
ANA |
Negative |
- |
- |
Three of 18 glomeruli examined from the renal biopsy showed near-global necrosis. Periglomerular fibrosis was detected in the other glomeruli (Figures 2 and 3). Glomerular tuft collapse was noted in some of the glomeruli. Mesangial IgG (+) and C3 (++) accumulation were detected. The findings suggested chronic TIN associated with long-term diclofenac use. Renal function did not return to normal during follow-up despite high-dose steroid therapy, so the patient was admitted to the HD programme. After about 4 months of chronic HD therapy, the patient exhibited improved renal function and HD was discontinued. The patient is currently under follow-up without HD (for 6 months) and his most recent creatinine levels ranged from 2 to 2.5 mg/dl.
DISCUSSION
The acute or chronic renal effects of NSAIDs constitute a major proportion of their numerous systemic effects. These drugs have been associated with acute tubular necrosis (ATN), hyponatremia/hyperkalemia, acute/chronic TIN, renal tubular acidosis, papillary necrosis, hypertension, minimal change disease/membranous glomerulonephritis, CKD, and in the long-term, urothelial cancer. Drugs are the most common cause of acute TIN. It can also occur as a result of infections, systemic diseases (sarcoidosis, Sjögren’s syndrome, multiple myeloma, IgG4-related disease), TIN and uveitis syndrome, and idiopathic causes. In some series, acute TIN was detected in 1–3% of kidney biopsies overall and 15–27% when limited to patients who underwent biopsy for the differential diagnosis of AKI.2 Drug-associated TIN accounts for 85% of all TIN cases, and may be highly reversible (~70%) in the early stage. Progression to CKD occurs in about 50% of TIN cases with delayed diagnosis or ongoing drug exposure.
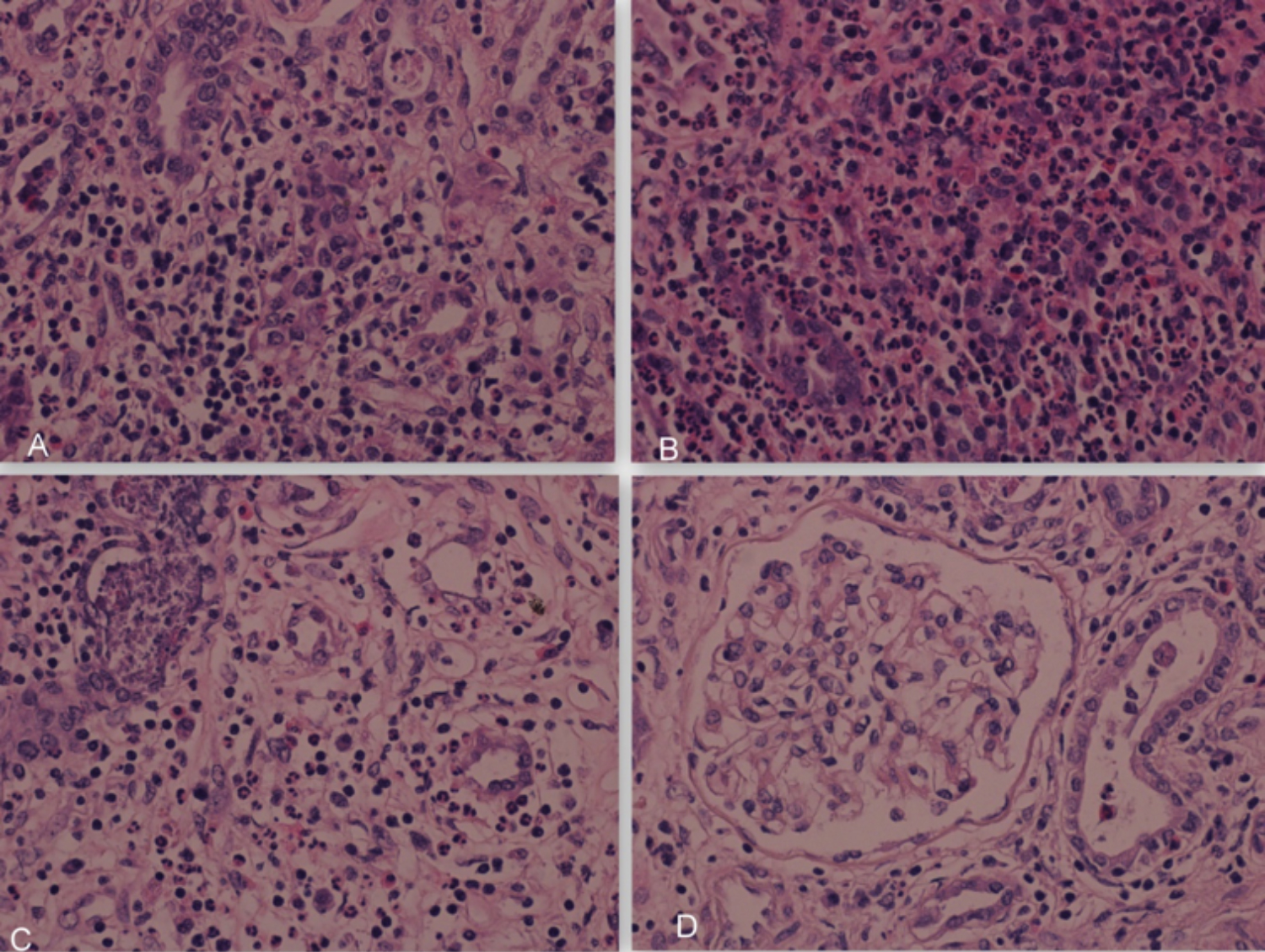 Figure 1: (A) Inflammatory cell infiltration in the tubulointerstitital area (haematoxylin eosinx40). (B) Destruction and regenerative/degenerative changes in tubular epithelial cells, oedema, and severe acute inflammatory cell infiltration of leukocytes and eosinophils with polymorphic nuclei in the tubular lumen and interstitium (haematoxylin eosinx40). (C) Oedema in the tubulointerstitial area and debris of leukocytes with polymorphic nuclei (haematoxylin eosinx40). (D) Glomeruli are normal (haematoxylin eosinx40). There is no immunohistochemical staining, acute tubulointerstitial nephritis.
Figure 1: (A) Inflammatory cell infiltration in the tubulointerstitital area (haematoxylin eosinx40). (B) Destruction and regenerative/degenerative changes in tubular epithelial cells, oedema, and severe acute inflammatory cell infiltration of leukocytes and eosinophils with polymorphic nuclei in the tubular lumen and interstitium (haematoxylin eosinx40). (C) Oedema in the tubulointerstitial area and debris of leukocytes with polymorphic nuclei (haematoxylin eosinx40). (D) Glomeruli are normal (haematoxylin eosinx40). There is no immunohistochemical staining, acute tubulointerstitial nephritis.
Diclofenac is a Group 1 NSAID and inhibits both COX-1 and COX-2 pathways. It decreases renal prostaglandin levels, inhibiting the vasodilator effect and reducing renal blood flow, which determines glomerular filtration rate. Therefore, due to these hemodynamic effects, they can lead to dose-dependent kidney damage. Moreover, they cause immune-mediated (primarily cellular) damage independent of dose. Drug-induced renal injury is attributed to the induction of host inflammatory response (delayed hypersensitivity reaction). Diclofenac-associated kidney damage is attributed to its effect on prostaglandin synthesis, as well as mitochondrial damage and reactive oxygen species production.
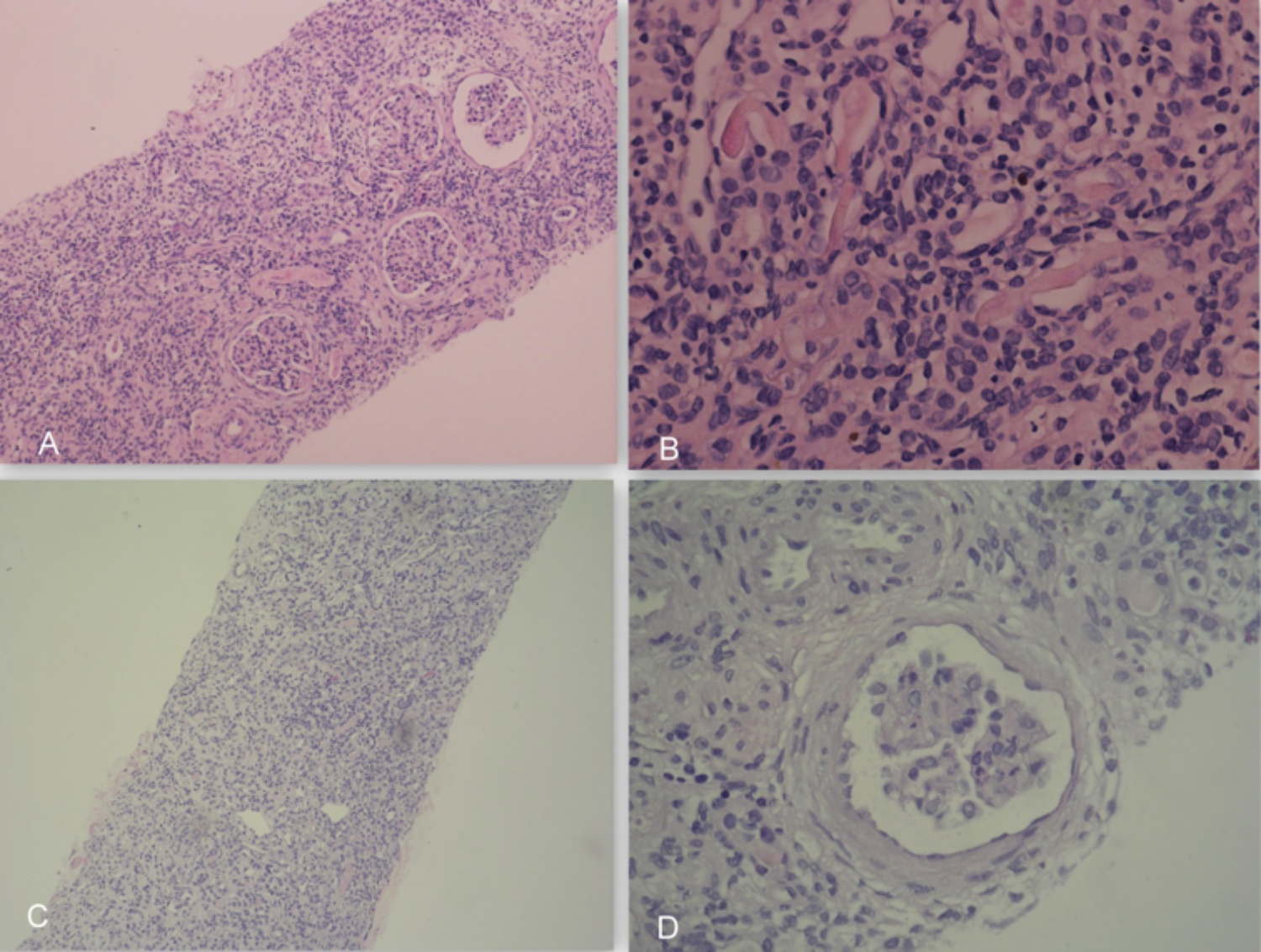 Figure 2: (A) Chronic inflammation in the tubulary and interstitial area (haematoxylin eosin x10). (B) Tubular thyroidisation (haematoxylin eosin x40). (C) Tubulointerstitial cell infiltration rich in lymphocytes and plasma cells (haematoxylin eosin x10). (D) Periglomerular fibrosis (haematoxylin eosin x40). Chronic tubulointerstitial nephritis.
Figure 2: (A) Chronic inflammation in the tubulary and interstitial area (haematoxylin eosin x10). (B) Tubular thyroidisation (haematoxylin eosin x40). (C) Tubulointerstitial cell infiltration rich in lymphocytes and plasma cells (haematoxylin eosin x10). (D) Periglomerular fibrosis (haematoxylin eosin x40). Chronic tubulointerstitial nephritis.
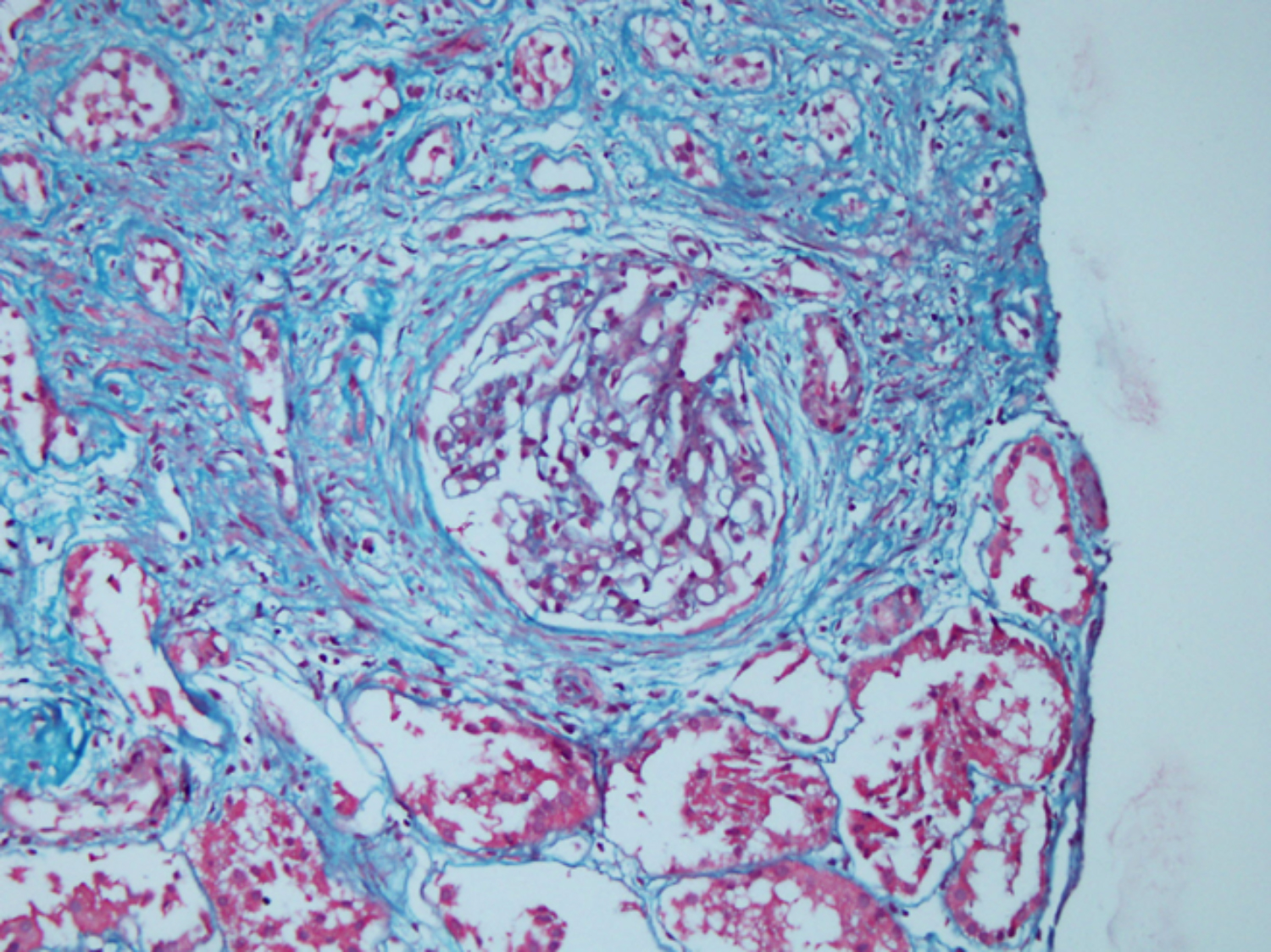 Fıgure 3: Periglomerular fibrosis (Masson Trichrome x40).
Fıgure 3: Periglomerular fibrosis (Masson Trichrome x40).
NSAIDs, such as diclofenac, are responsible for 20% of NSAID-related kidney damage. It may follow an asymptomatic course, with no clear signs or symptoms. Proteinuria is usually around 1 g/24 h, but nephrotic levels can be detected in 10% of patients. Patients with conditions such as CKD, heart failure, and liver dysfunction, those using drugs such as angiotensin-receptor blockers, angiotensin-converting enzyme inhibitors, cyclosporin, and diuretics, and/or at advanced age are at risk of NSAID-induced AKI.3
Because our case had recurrent TIN, he was screened for potential chronic autoimmune and granulomatous diseases before the second biopsy. In recurrent TIN, even if the patient provides a history that is consistent with their clinical presentation, screening for renal involvement of subclinical chronic granulomatous and autoimmune diseases is recommended.
The development of chronic TIN of the same or different aetiology following successful treatment of acute TIN associated with diclofenac use is not a common phenomenon. Similar to our case, there are previous reports of diclofenac-induced recurrent NS together with ATN/MCD that responded well to steroids.4,5 In a study evaluating drug-related renal effects, diclofenac was found to be the NSAID, most associated with nephrotoxic damage. The most common renal pathologies in that report were AKI, tubular necrosis, and TIN.6
The first step of treatment in drug-induced TIN is early recognition and discontinuation of the inciting drug. If there is no clinical response to drug cessation, steroid therapy should be tried first. Gonzalez et al. reported greater improvement in renal function with steroid therapy initiated within two weeks after diagnosis.7 At 24th month after biopsy, Prendecki et al. found that patients treated with steroids had higher mean estimated glomerular filtration rate (43 mL/min vs. 24 ml/min) and lower dependence on dialysis (5.1% vs. 24.1%), compared to patients who did not receive steroid therapy.2 The use of other immunosuppressive agents (e.g., mycophenolate mofetil, azathioprine, methotrexate) appears to be beneficial in patients who relapse after steroid discontinuation or are steroid-dependent. In our case, acute TIN at initial presentation significantly improved after discontinuing diclofenac sodium and administering low-dose steroid therapy. However, at second presentation, the patient was found to have developed steroid-refractory chronic TIN due to continued use of diclofenac. This may be attributable to chronicity of the inflammatory process or irreversible impairment of renal perfusion.
The priority in clinical practice is to detect and eliminate the causative agent of interstitial nephritis. In addition, the current approach includes steroid therapy and treating complications and comorbidities such as proteinuria, hypertension, and infection according to the degree of renal damage. If steroid therapy is planned, it must be initiated early and continued for at least one month. We have observed that newly introduced drugs can often cause interstitial nephritis. However, older and traditional agents must not be overlooked, and every patient should be questioned about these, when taking their history.
Unfortunately, public usage of NSAIDs is still widespread and unsupervised. It should be kept in mind that patients with a history of nephrotoxic injury may be subject to similar effects, if they continue using NSAIDs. It is essential to obtain a detailed medication history at every visit, especially in outpatient clinics. The renal effects of NSAIDs are still dangerous, and public awareness on this issue should be raised.
CONFLICT OF INTEREST:
The authors have declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
FRO: Collected the patient data, wrote the whole manuscript and participated in literature review.
TK: Analysed the pathological findings.
AA: Supervised and modified the article.
REFERENCES
- Martin-Navarro JA, Petkov-Stoyanov V, Gutierrez-Sanchez MJ, Pedraza-Cezon L. Acute renal failure secondary to interstitial acute nephritis and fanconi syndrome for metamizole and gemfibrozil. Nefrologia 2016; 36(3):321-3. doi: 10.1016/j.nefro.2015.06.022.
- Prendecki M, Tanna A, Salama AD, Tam FW, Cairns T, Taube D, et al. Long-term outcome in biopsy-proven acute interstitial nephritis treated with steroids. Clin Kidney J 2017; 10(2):233-9. doi: 10.1093/ckj/sfw116.
- Haas M, Spargo BH, Wit EJ, Meehan SM. Etiologies and outcome of acute renal insufficiency in older adults: A renal biopsy study of 259 cases. Am J Kidney Dis 2000; 35(3):433-47. doi: 10.1016/s0272-6386(00)70196-x.
- Lam MF, Lui SL, Lo WK. Recurrent nephrotic syndrome induced by nonsteroidal anti-inflammatory drugs. Hong Kong J Nephrol 2003; 5(2):98-100.
- Galesic K, Ljubanovic D, Bulimbasic S, Racic I. Minimal change disease and acute tubular necrosis caused by diclofenac. Nephrology 2008; 13(1):87-9. doi: 10.1111/ j.1440-1797.2007.00863.x.
- Prescriber Update. 2013; 34:14-5.
- Gonzalez E, Gutierrez E, Galeano C, Chevia C, de Sequera P, Bernis C, et al. Early steroid treatment improves the recovery of renal function in patients with drug-induced acute interstitial nephritis. Kidney Int 2008; 73(8):940-6. doi: 10.1038/sj.ki.5002776.