Acute Ischemic Stroke after Thyroid Examination
By Avni Uygar Seyhan, Rohat Ak, Erdal YilmazAffiliations
doi: 10.29271/jcpsp.2021.03.367Sir,
A 78-year woman presented to Emergency Department (ED) complaining of weakness in her right lower extremity. The patient reported she had an examination for the thyroid gland in general surgery outpatient clinic that morning; and that her complaint of lower extremity weakness had started one hour after that examination. Her past medical history showed that she had diabetes mellitus (DM) for 13 years and hypertension for 11 years. For these medical disorders, she regularly took metformin and bisprolol medications. Upon presentation to ED, her vital signs were: blood pressure 130/ 80 mmHg, heart rate of 73 bpm, and blood oxygen saturation on room air (SpO2) of 98%. ECG showed atrial fibrillation. On physical examination, the patient was cooperative and orientated. Neurological examination showed motor deficit in right lower extremity. Bedside trans-thoracic echocardiography revealed normal left ventricle systolic functions [Ejection fraction (EF), 65%] and left atrial dilation. No thrombus was observed in heart cavities. Blood tests including complete blood count, biochemistry, and coagulation profile were within normal limits. A fasting lipid profile on the second day of hospitalisation showed: total cholesterol 233 mg/dL, low-density lipoprotein cholesterol (LDL-C) 154 mg/dL, triglycerides 144 mg/dL, and a high density lipoprotein cholesterol (HDL-C) 50 mg/dL. Thyroid function tests and thyroid ultrasonography examination were normal. No acute pathology was detected on brain computed tomography (CT). Diffusion-weighted MRI demonstrated a hyper-intense region adjacent to the posterior horn of the left ventricle (Figure 1). The apparent diffusion coefficient (ADC) in this territory was reduced (Figure 2). Brain CT angiography showed intense plaque formation bilaterally in internal carotid arteries (ICAs). It was thought that this cerebrovascular accident (CVA) had developed due to blood vessel atherosclerosis and not secondary to cardio-embolic stroke. As there was no indication for thrombolytic therapy, the patient was started on low-dose aspirin and apixaban medications.
Prevention of risk factors and correction of treatable ones are important in preventing stroke. Stroke risk factors are divided into three groups: unchangeable (age, gender, race, genetics), changeable (hypertension, diabetes, smoking, alcohol, physical inactivity, etc) and potentially changeable (hyperhomocysteinemia, inflammation, and infection).1,2 Half of all ischemic strokes occur due to atherosclerosis of large arteries. Stroke occurs due to thrombus formation as a result of rupture of the atheroma plaques in the extra-cranial and/or intra-cerebral vascular structures and bifurcations. Prognosis varies according to the region that had been thrombosed. Most commonly, high cortical dysfunctions, sensory and motor deficits occur; and rarely brain stem and cerebellar dysfunction can be seen.3,4 Atherosclerotic plaque rupture leads to platelet activation and formation of occlusive thrombi that trigger acute ischemic events.5,6
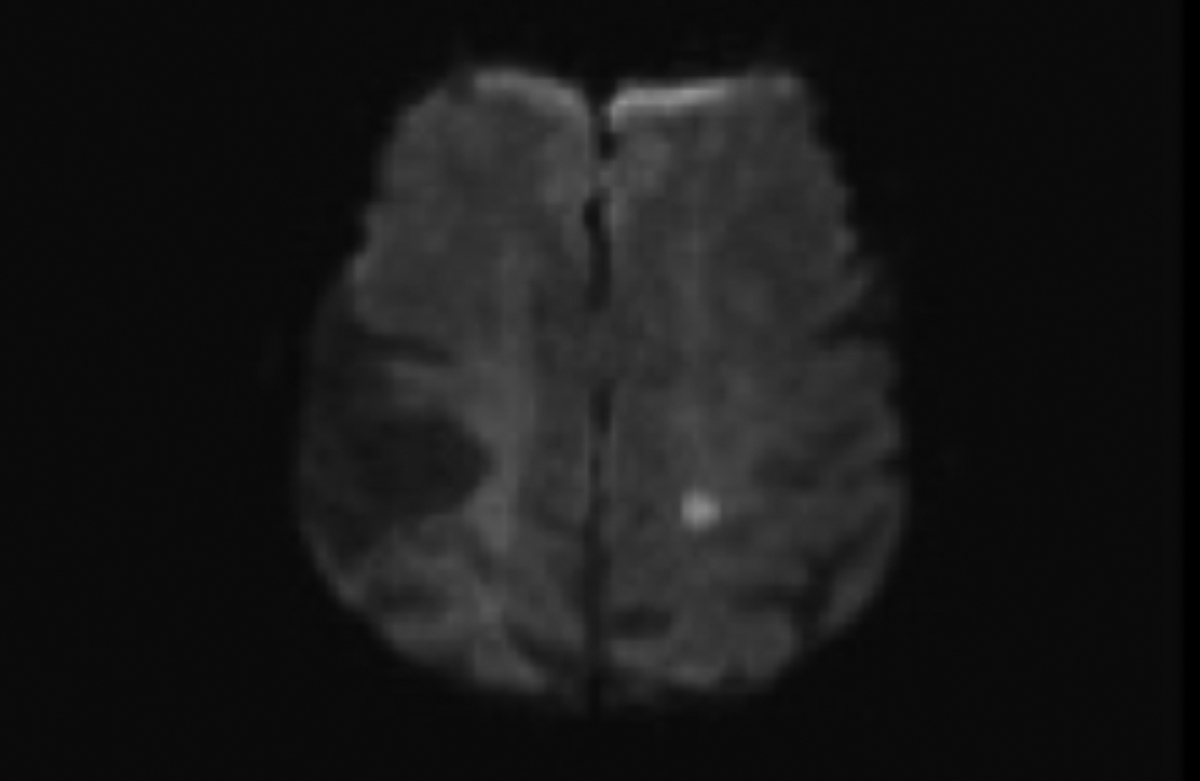 Figure 1. Diffusion-weighted MRI demonstrates a hyperintense region adjacent to the left ventricle posterior horn.
Figure 1. Diffusion-weighted MRI demonstrates a hyperintense region adjacent to the left ventricle posterior horn.
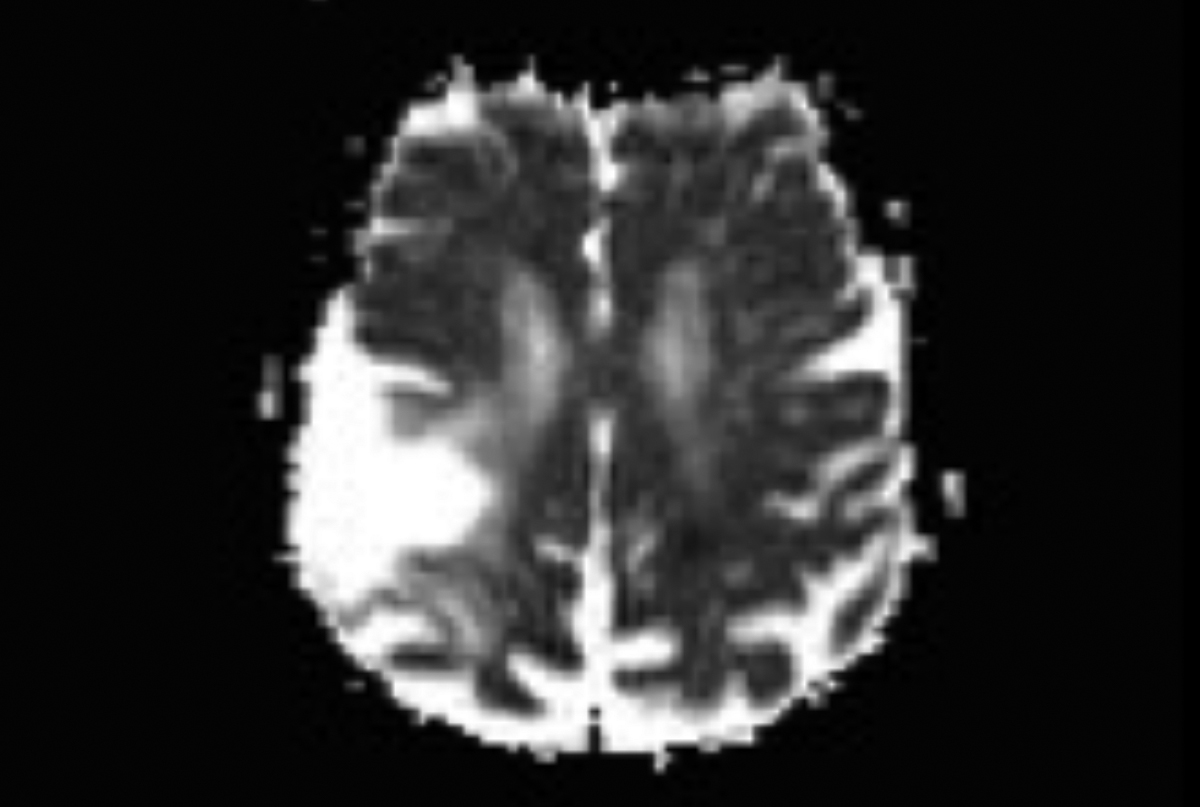 Figure 2. Apparent diffusion coefficient (ADC) in the territory shown in Figure 1 is reduced.
Figure 2. Apparent diffusion coefficient (ADC) in the territory shown in Figure 1 is reduced.
In the case we presented, the patient developed acute ischemic stroke after thyroid examination. CT angiography showed intense plaque formations bilaterally in the ICAs, suggesting that the cause of stroke was probably rupture of atherosclerotic plaques. Although the patient had risk factors for stroke such as advanced age, DM, and hypertension, the presence of dense plaques in bilateral ICAs and the history that complaint started just after thyroid gland examination suggests that thyroid examination triggered ischemic stroke. Physicians should be careful when performing neck thyroid examination, especially in patients with risk factors, and need to educate their patients about the changeable risk factors of stroke.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
AUS, RA, EY: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; and final approval of the version.
REFERENCES
- Strong K, Mathers C, Bonita R. Preventing stroke: Saving lives around the world. Lancet Neurol 2007; 6(2):182-7. doi: 10.1016/S1474-4422(07)70031-5.
- Kempers EWS. Insights in the effectiveness of usual care regarding functional decline in geriatric and stroke patients. Utrecht University 2016; Available from: https:// dspace.library.uu.nl/handle/1874/334905.
- Jauch EC, Saver JL, Adams HP, Bruno A, Connors JJB, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013; 44:870-947. doi.org/10.1161/STR.0b013e31828 4056a.
- Boehme AK, Esenwa C, Elkind MSV. Stroke risk factors, genetics, and prevention. Circ Res 2017; 120(3):472-95. doi: 10.1161/CIRCRESAHA.116.308398.
- Gao T, Zhang Z, Yu W, Zhang Z, Wang Y. Atherosclerotic carotid vulnerable plaque and subsequent stroke: A high-resolution MRI study. Cerebrovascular Diseases 2009; 27(4): 345-352. doi: 10.1159/000202011.
- Banerjee C, Chimowitz MI. Stroke caused by atherosclerosis of the major intracranial arteries. Circulation research 2017; 120(3):502-13. doi: 10.1161/CIRCRESAHA.116. 308441.