A Circular Intrahepatic Portal Vein
By Deng Yong Zhang, Zheng LuAffiliations
doi: 10.29271/jcpsp.2021.03.365Sir,
A knowledge of anatomy of the intrahepatic portal vein (PV) is essential to guiding hepatectomy. The 5 types of PV, described by Atri et al.,1 have been used until now. We now report a case of PV variation that has never been seen before.
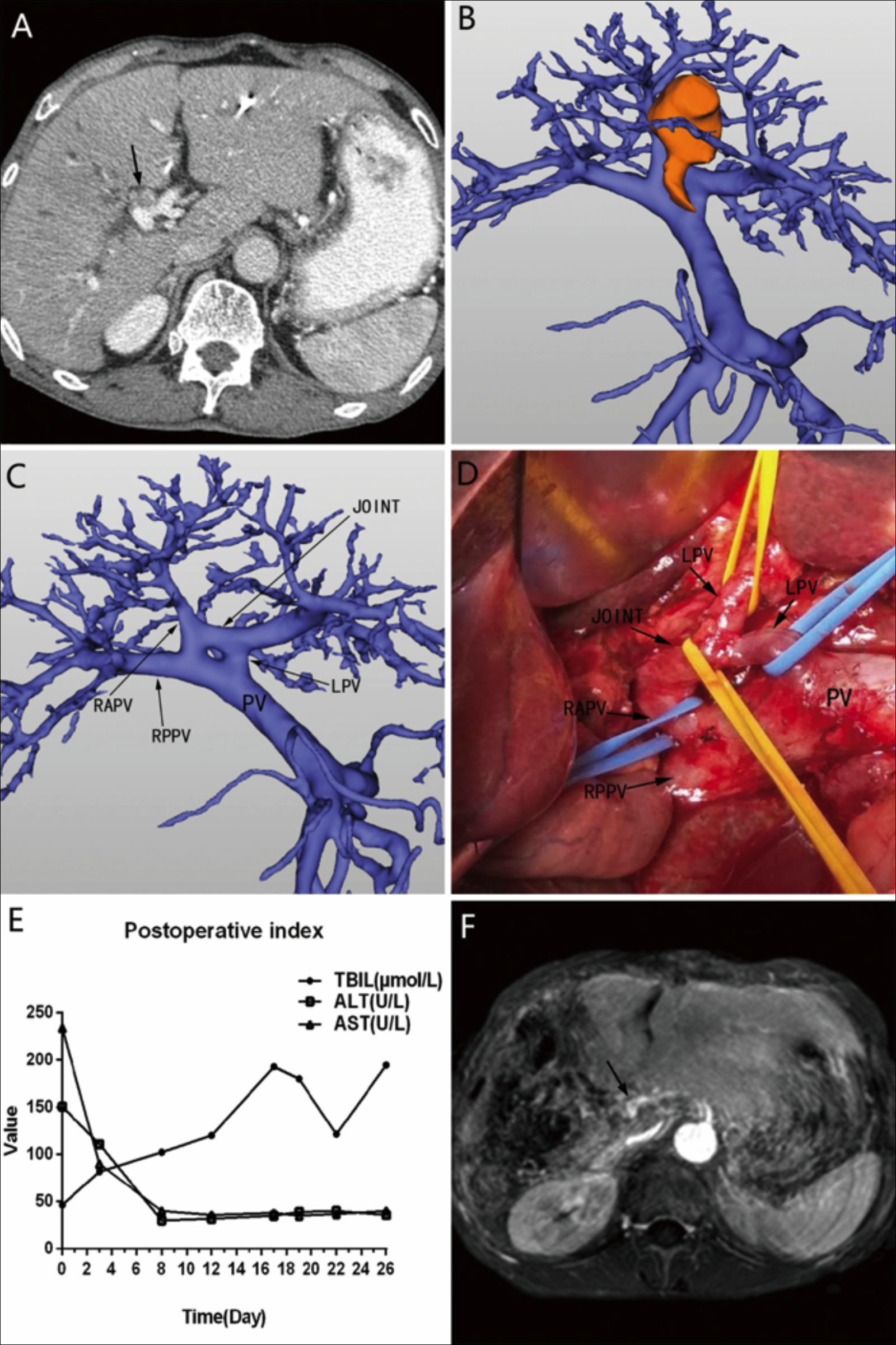 Figure 1: (A) CT scan revealing a tumor located in the hilum of the liver; the arrow indicates the tumor. (B) Three-dimensional reconstruction examination of the portal vein and tumor (yellow lump). (C) Three-dimensional reconstruction examination of the portal vein. (D) Anatomy of the portal vein, as observed during the operation. (E) The patient’s postoperative total bilirubin, alanine aminotransferase, and aspartate aminotransferase concentrations. (F) MRI showing the left portal vein (arrow) after surgery.
Figure 1: (A) CT scan revealing a tumor located in the hilum of the liver; the arrow indicates the tumor. (B) Three-dimensional reconstruction examination of the portal vein and tumor (yellow lump). (C) Three-dimensional reconstruction examination of the portal vein. (D) Anatomy of the portal vein, as observed during the operation. (E) The patient’s postoperative total bilirubin, alanine aminotransferase, and aspartate aminotransferase concentrations. (F) MRI showing the left portal vein (arrow) after surgery.
PV: Portal vein; LPV: Left port vein; RPV: Right portal vein; RAPV: Right advanced port vein; RPPV: Right posterior port vein; JOINT: The connection of RAPV and LPV; CT: Computed tomography; ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; MRI: Magnetic resonance image.
A 71-year male presented to our Department for progressively worsening jaundice symptoms. Obvious dilatation of intrahepatic bile duct was found by ultrasonography. CT scan revealed a hilar bile duct tumor (Figure 1A), which on three-dimensional reconstruction was seen to invade the right anterior portal vein (RAPV) (Figure 1B) and right and left hepatic ducts, but not the hepatic artery or left portal vein (LPV). The patient’s CA19-9 was >1200 IU/mL. The preoperative diagnosis was Bismuth IV hilar cholangiocarcinoma. We observed a curious circular intrahepatic PV variation (Figure 1C), in which the RAPV joined the LPV. Percutaneous transhepatic bile drainage was conducted. The patient’s total bilirubin concentration decreased from 315.2 μmol/L preoperatively to 43.5 μmol/L. We considered right hemihepatectomy and caudate lobectomy. Reserved liver volume calculated using three-dimensional reconstruction was 52%. The PV’s diameter was 11 mm, the LPV was 4 mm, the right posterior PV (RPPV) was 9 mm, and RAPV was 5 mm during the operation. The PV’s anatomic variation was consistent with preoperative findings (Figure 1D). We performed right hemihepatectomy, caudate lobectomy, and cholangiojejunostomy. Figure 1E shows the total bilirubin increase, and the liver function index decreased postoperatively. The postoperative prothrombin time was 16.4 sec and the international normalised ratio was 1.48. No biliary obstruction or PV tumor thrombus was observed postoperatively on magnetic resonance imaging (Figure 1F). The patient died on the 30th day postoperatively.
A knowledge of anatomy of PV is essential to hepatectomy, especially hemihepatectomy. Many doctors overlook variations in PV because of its low incidence in clinical settings, leading to many adverse complications after surgery. Although many other researchers have explored the variations of PV through various autopsy and imaging techniques, no new type of PV has been observed.2-8 In our case,the cause of liver failure was thin LPV, which did not provide sufficient blood supply for the residual liver. The discovery of this variant and its painful lesson may provide a warning to other surgical teams.
CONFLICT OF INTEREST:
The authors have no conflicts of interest to disclose.
AUTHORS’ CONTRIBUTION:
DYZ: Drafted the manuscript;
ZL: Revised the manuscript.
REFERENCES
- Atri M, Bret PM, Fraser-Hill MA. Intrahepatic portal venous variations: Prevalence with US. Radio 1992; 184(1): 157-158. doi: 10.1148/radiology.184.1.1609075.
- Manjunatha YC, Beeregowda YC, Bhaskaran A. An unusual variant of the portal vein. J Clinl Diagnostic Res 2012; 6(4):731-3.
- Koç Z, Oğuzkurt L. Portal vein variations: Clinical implications and frequencies in routine abdominal multidetector CT. Diagn Interv Radiol 2007; 13(2):75-80.
- Sureka B, Patidar Y, Bansal K, Rajesh S, Agrawal N, Arora A. Portal vein variations in 1000 patients: Surgical and radiological importance. Br J Radio 2015; 88(1055): 20150326. doi: 10.1259/bjr.20150326.
- Akgul E, Inal M, Soyupak S, Binokay F, Aksungur E, Oguz M. Portal venous variations. Prevalence with contrast-enhanced helical CT. Acta Radiol 2002; 43(3):315-9. doi: 10.1080/j.1600-0455.2002.430314.x.
- Cheng YF, Huang TL, Lee TY, Chen TY, Chen CL. Variation of the intrahepatic portal vein; angiographic demonstration and application in living-related hepatic transplantation. Transplant Proc 1996; 28(3):1667-8.
- Erbay N, Raptopoulos V, Pomfret EA, Kamel IR, Kruskal JB. Living donor liver transplantation in adults: Vascular variants important in surgical planning for donors and recipients. AJR Am J Roentgenol 2003; 181(1):109-114. doi: 10.2214/ajr.181.1.1810109.
- Covey AM, Brody LA, Getrajdman GI, Sofocleous CT, Brown KT. Incidence, patterns, and clinical relevance of variant portal vein anatomy. AJR Am J Roentgenol 2004; 183(4): 1055-64. doi: 10.2214/ajr.183.4.1831055.