Scheuermann’s Disease as a Risk Factor for Lumbar Disc Herniation Recurrence
By Yan Ding1,2, Shiqiao Lv2, Guangrun Li3, Shengjie Dong2, Xuri Sun2, Yunzhen Chen1Affiliations
doi: 10.29271/jcpsp.2020.06.584ABSTRACT
Objective: To verify whether Scheuermann’s disease (SD) is a risk factor for patients with recurrent lumbar disc herniation (rLDH) than in patients without recurrence.
Study Design: Case-control study.
Place and Duration of Study: Department of Orthopaedics, Yantaishan Hospital, China, from December 2016 to September 2019.
Methodology: The demographics (age, gender, body mass index [BMI], alcohol abuse, and current smoking), diabetes mellitus, and radiological data (affected levels, herniated side, herniation type, Pfirrmann grade, and the presence of SD) of 602 patients were retrospectively analysed, who underwent surgery for symptomatic LDH from December 2016 to August 2018. They were underwent one-year follow-up and were divided into LDH and rLDH groups. Both typical and atypical SD criteria were used to diagnose SD. Independent-sample t-test was used to analyse the role of age and BMI in both groups, and the Chi-square test was conducted to analyse other parameters. Logistic regression analysis was performed to evaluate various factors.
Results: There was a significant difference in age (p=0.026), BMI (p=0.007), current smoking (p=0.001), and SD (p<0.001) between the groups. When these parameters were included in the logistic regression analysis, age, current smoking status, and SD were found to be risk factors for rLDH.
Conclusion: Age, current smoking, and SD are risk factors for rLDH. Older patients with radiological characteristics of SD should quit smoking to prevent rLDH.
Key Words: Scheuermann’s disease, Kyphosis, Disc herniation, Recurrence, Age, Smoking, Risk factor.
INTRODUCTION
Lumbar disc herniation (LDH) is the most frequently occurring disorder of the lumbar spine, accompanied with symptoms of back pain, and radiating leg pain. Lumbar discectomy is the most prevalent surgery for treating LDH; with reported complication rate of 5%–20%.1 The most common complication indicating an unsatisfactory surgery is recurrent LDH (rLDH), occurring in 5%–15% of the cases.2-4 The widely accepted definition of rLDH is LDH re-appearance at the same level regardless of the side, ipsilateral or contralateral, causing radiculopathy.2,4,5
However, the pain-free interval after the primary surgery is debatable, suggested as at least 6 months,2,4-6 two months,7 or at least one month.8 It may be caused by further disc material extruding from the primary disc space, with or without associated scar tissue; retained disc fragments at the time of the first discectomy; or compression of the neural elements by parts of the disc endplate including bone, annulus, and other reactive tissues.1,4 Treatment of symptomatic rLDH is associated with a longer hospital stay, higher surgical costs, delayed return to work, and poorer outcomes compared to those achieved by primary intervention.2,4 Thus it is important to identify risk factors for rLDH to prevent recurrence.
Scheuermann’s disease (SD) was first described as a structural thoracic kyphosis with more than three wedged vertebrae (WV). SD usually develops from adolescence but does not present any symptoms until adulthood.9,10 Thus, the worldwide accepted definition of SD now is the appearance of the radiographic features of SD, with or without clinical symptoms.10,11 Typical SD is defined as ≥3 consecutive WV, with an angle of at least 5°, while atypical SD is defined as only one or two WV with endplate or disc lesions.12
Table I. Comparison of the demographic, clinical and radiographic parameters between the groups.|
|
LDH group |
rLDH group |
p-value |
|
|
Total number |
569 |
33 |
|
|
|
Age (mean ± standard deviation) |
50.14±13.67 |
55.58 ±11.98 |
0.026* |
|
|
BMI (mean ± standard deviation) |
23.71 ±3.07 |
24.69 ±1.84 |
0.007** |
|
|
Sex |
Male (%) |
304 (53.43%) |
22 (66.67%) |
0.138 |
|
Female (%) |
265 (46.57%) |
11 (33.33%) |
||
|
Alcohol |
Yes (%) |
151 (26.54%) |
7 (21.21%) |
0.499 |
|
No (%) |
418 (73.46%) |
26 (78.79%) |
||
|
Current smoking |
Yes (%) |
201 (35.33%) |
21 (63.64%) |
0.001** |
|
No (%) |
368 (64.67%) |
12 (36.36%) |
||
|
Diabetes mellitus |
Yes (%) |
75 (13.18%) |
7 (21.21%) |
0.191 |
|
No (%) |
494 (86.82%) |
26 (78.79%) |
||
|
Herniation type |
Protrusion |
136 (23.90%) |
7 (21.21%) |
0.565 |
|
subligamentous extrusion |
152 (26.71%) |
9 (27.27%) |
||
|
Transligamentous extrusion |
130 (22.85%) |
5 (15.15%) |
||
|
Sequestration |
151 (26.54%) |
12 (36.36%) |
||
|
Pfirrmann grade |
I |
27 (4.75%) |
0 (0.00%) |
0.330 |
|
II |
69 (12.13%) |
7 (21.21%) |
||
|
Ⅲ |
17 1(30.05%) |
7 (21.21%) |
||
|
Ⅳ |
144 (25.31%) |
10 (30.30%) |
||
|
Ⅴ |
113 (19.86%) |
5 (15.15%) |
||
|
Ⅵ |
45 (7.91%) |
4 (12.12%) |
||
|
Affected level |
L3/4 |
53 (9.31%) |
4 (12.12%) |
0.853 |
|
L4/5 |
276 (48.51%) |
16 (48.48%) |
||
|
L5/S1 |
240 (42.18%) |
1 3 (39.39%) |
||
|
Herniated side |
Left |
299 (52.55%) |
14 (42.42%) |
0.258 |
|
Right |
270 (47.45%) |
19 (57.58%) |
||
|
SD |
Yes (%) |
179 (31.46%) |
26 (78.79%) |
<0.001** |
|
No (%) |
390 (68.54%) |
7 (21.21%) |
||
|
p<0.05, p<0.01, BMI=body mass index, SD=Scheuermann’s disease, LDH=lumbar disc herniation, rLDH=recurrent lumbar disc herniation. |
||||
The pathophysiology of SD remains unclear,13 though some authors suggested possible genetic causes.14 Besides kyphosis, the common pathological changes of SD include the lesions of vertebral endplates and discs, with the appearance of radiological features such as Schmorl’s nodes (SNs), irregular vertebral end plates (IEs), and disc lesions.12
Various studies have reported diverse risk factors for rLDH including demographic parameters like age,1-6,8,15 gender,4,15 body mass index (BMI),4,6,16,17 alcohol abuse,4 cigarette smoking status,3,18,19 clinical complications such as diabetes mellitus,4,18,20 and radiological characters (affected levels, herniated side, herniation type, and Pfirrmann grade)4,7,16,18, but only few reported on congenital structural diseases.21 Given that SD can induce disc degeneration, endplate lesions11,12 which can further impact the fibrous ring healing after discectomy, it is reasonable to speculate that SD might be associated with rLDH. In the authors’ clinical practice, it was noticed that SD occurred more frequently in patients with rLDH than in patients without recurrence. Thus, the aim of the present study to investigate SD as a risk factor for rLDH.
METHODOLOGY
Patients who were diagnosed with LDH and underwent single-level discectomy at the Spine Centre, Department of Orthopaedics, Yantaishan Hospital from December 2016 to August 2018. All patients were followed up for one year and then were divided into two groups: LDH group (non- recurrent, 569 cases) and rLDH group (recurrent, 33 cases). The study was approved by the Affiliated Yantai Yuhuangding Hospital of Qingdao University (Approval No. 2020-008), and written informed consent was obtained from the patients and their relatives.
Table II. Results of multivariate analysis identifying potential risk factors for predicting recurrence after lumbar discectomy.
|
|
Odds radio |
95% CI |
p-value |
|
Age |
1.047 |
1.005–1.091 |
0.030* |
|
Sex |
0.604 |
0.189–1.931 |
0.395 |
|
BMI |
1.097 |
0.962–1.251 |
0.167 |
|
Alcohol |
0.421 |
0.157–1.125 |
0.084 |
|
Current smoking |
4.077 |
1.359–12.234 |
0.012** |
|
Diabetes mellitus |
1.062 |
0.337–3.348 |
0.918 |
|
Herniation type |
1.201 |
0.855–1.688 |
0.290 |
|
Pfirrmann grade |
0.808 |
0.553–1.180 |
0.269 |
|
Affected Level |
1.290 |
0.699–2.378 |
0.415 |
|
Herniated Side |
1.349 |
0.630–2.890 |
0.441 |
|
SD |
8.300 |
3.339–20.635 |
<0.001** |
|
p<0.05, p<0.01, CI=confidence interval, BMI=body mass index, SD=Scheuermann's disease. |
|||
Only the primary surgical procedures performed by the posterior approach, tubular assistant discectomy with laminotomy, were included. In addition, the levels involving L3/4, L4/5, and L5/S1 were included. Patients who received other surgical procedures including percutaneous endoscopic discectomy, discectomy with unilateral laminectomy (hemilaminectomy), discectomy with bilateral laminectomy (total laminectomy), and discectomy with fixation and fusion were excluded. Those with a pain-free interval shorter than one month were also excluded. The other exclusion criteria were primary herniation at other levels, inability to have magnetic resonance imaging (MRI) examination, spine trauma history, pathological vertebral fractures, active infection, spinal metastasis and other congenital spinal disorder (i.e. scoliosis). Pain-free interval of at least one-month after the primary surgery was taken as duration of recurrence.8 The rLDH cases were diagnosed by postoperative MRI if patients complained of the recurrent leg pain.
All the patients received preoperative radiologic examination (including X-ray, computed tomography scan, and MRI). Patient demographic information (age, gender, BMI, alcohol abuse, current smoking status), diabetes mellitus status, and radiological characteristics (affected levels, herniated side, herniation type, Pfirrmann grade, and the presence of SD) were collected before the primary surgery and were analysed. The types of herniation were classified as protrusion, subligamentous extrusion, transligamentous extrusion, and sequestration, by reviewing the surgical records. The degree of disk degeneration was assessed on T2-weighted sagittal sequences according to modified Pfirrmann criteria.4,22
Both the classic Sorenson’s criterion (at least three consecutive WV showing >5° of anterior wedging in the thoracic or lumbar spine region) and the modified Heithoff’s criterion (simultaneous presence of less than three WV with multiple SN and IE in the thoracic and/or lumbar spine region) were used to diagnose SD.11,12 Patients’ images meeting either one of these criteria were defined as SD. A typical case of SD with rLDH is shown in Figure 1.
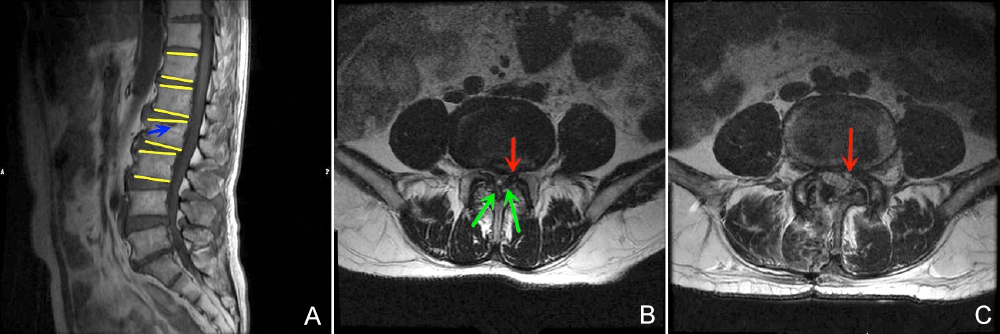 Figure 1: Typical case. Male patient aged 67 years with a history of smoking. Complaints: lower back pain with radiating left leg pain. No intermittent claudication. (A) His MRI findings meet the criteria for typical SD, as reflected by the presence of at least three consecutive wedged vertebrae (T12, L1, L2, L3, yellow line) and Schmorl’s nodes (blue arrows). (B) He was diagnosed with L4/5 LDH (red arrows) combined with lumbar spinal stenosis caused by hypertrophy of the ligament flavum (green arrows). (C) He underwent tubular-assisted bilateral approach decompression and discectomy and achieved full release after the operation. Unfortunately, his symptoms recurred one month after the primary surgery, which led to the diagnosis of rLDH on MRI (red line).
Figure 1: Typical case. Male patient aged 67 years with a history of smoking. Complaints: lower back pain with radiating left leg pain. No intermittent claudication. (A) His MRI findings meet the criteria for typical SD, as reflected by the presence of at least three consecutive wedged vertebrae (T12, L1, L2, L3, yellow line) and Schmorl’s nodes (blue arrows). (B) He was diagnosed with L4/5 LDH (red arrows) combined with lumbar spinal stenosis caused by hypertrophy of the ligament flavum (green arrows). (C) He underwent tubular-assisted bilateral approach decompression and discectomy and achieved full release after the operation. Unfortunately, his symptoms recurred one month after the primary surgery, which led to the diagnosis of rLDH on MRI (red line).
LDH = Lumbar disc herniation; MRI = Magnetic resonance imaging; SD = Scheuermann’s disease; rLDH = Recurrent lumbar disc herniation.
Continuous variables are expressed as mean ± standard deviation, and categorical variables are expressed either as frequencies or percentages. Independent-sample t-test and chi-squared test were performed to analyse the difference in continuous and categorical variables between the two groups, respectively. Furthermore, logistic regression analysis was performed to evaluate which variable can behave as independent risk factors for rLDH. SPSS (version 25.0, IBM SPSS, Chicago, IL, USA) was used for statistical analysis. P-values of less than 0.05 were considered significant.
RESULTS
There were 602 patients enrolled in this study, including 33 (5.48%) recurrent cases (rLDH group) and 569 (94.52%) non-recurrent cases (LDH group). In rLDH group, there were 22 males and 11 females with their ages ranging from 30 to 72 years. In LDH group, there were 304 males and 265 females and the ages ranged from 13 to 85 years . The mean pain-free period of rLDH group ranged from 1.07 to 10.53 months (4.78 ±2.28 months). The presence of SD was 78.79% (26/33) in rLDH group vs. 31.46% (179/569) in LDH group.
The results of univariate analysis of demographic, clinical, and radiologic parameters are shown in Table I. Of these factors, age (p=0.026), BMI (p=0.007), current smoking status (p=0.001), and SD (p=0.000) were found to be significantly associated with the incidence of rLDH. Including these parameters into the logistic regression analysis, age (P=0.030), current smoking status (p=0.012), and SD (p=0.000) were found to be risk factors of rLDH. The odds radio, 95% confidence interval (CI), and p-values are shown in Table II.
DISCUSSION
This study showed that the age, current smoking status, and SD were risk factors for rLDH. To the authors’ knowledge, this is the first study reporting SD as one of the risk factors for rLDH. Based on these findings, it is suggested that the older patients with radiological characteristics of SD should quit smoking to prevent rLDH.
The risk factors for rLDH are widely debated because of the various clinical and complicated biomechanical parameters involved.16 Many studies have investigated whether age is one of the risk factors for rLDH, but their results varied. Some researchers identified age as a risk factor,3,6 whereas others reported contradictory observations .1,2,5,8,15,17,19 Moreover, studies reporting that age was a risk factor also had two opposing viewpoints, wherein some authors concluded that the older patients had an increased risk of rLDH,18 while others reported that the younger patients were more prone to developing rLDH.6 This data confirmed that the older patients were more prone to recurrence, irrespective of analysis method (t-test or logistic regression). However, the odds radio was only 1.047, suggesting that old age may contribute to developing rLDH, but the risk is not very serious. A large cohort study published by Jansson et al.23 retrospectively reviewed 27,576 cases and reported that the patients with age between 40 and 59 years had a higher risk of reoperation than those with age <40 years. The age of patients in rLDH group of this cohort (55.58 ±11.98 years) also fell in this range indicating a possible link of advance age with rLDH. The other explanation may be that the discs in older patients are generally more degenerative, lack elasticity, and the remaining fragment of the nucleus pulposus is more susceptible to prolapse after primary surgery.18
Some studies considered BMI as a risk factor,16,17 whereas others did not.15,19 This data showed that BMI was higher in the rLDH group and could possibly contribute to rLDH. This association appears reasonable because increased loading of the operative disc may contribute to the recurrence of LDH.16,17 This observation is also supported by several biomechanical studies showing that even relatively small cyclical increases in intradiscal pressures could cause high shear and fibre strains along the posterolateral aspect of the annulus fibrosus, leading to disc herniation.16 However, BMI was not found to be a risk factor when analysed by logistic regression. This result may be attributed to the fact that our follow-up period was one year, whereas the effects of the axial load over the intervertebral space may only be apparent after a longer interval. Meredith et al. reported that the BMI >30 Kg/m2 might be an independent risk factor for recurrence17. In our study, although the BMI of the rLDH group was higher than that of the LDH group, BMIs did not exceed 25 Kg/m2 in both groups, indicating that these patients were not severely obese. This might be another reason for BMI not being a significant risk factor in our patient population.
Although some studies concluded that the smoking was not a risk factor for rLDH,2,15,17 numerous studies have identified smoking as a risk factor,3,18,19 which is comparable to our data. This study revealed that the patients in rLDH group (63.64%) had significantly more number of smokers than in LDH group (35.33%). Logistic regression analysis showed that the risk for rLDH was four times higher in smokers than in non-smokers. Smoking contributes to many pathological processes, but the exact mechanism has not been completely elucidated. The potential mechanisms may be as follows. First, it was speculated that the toxins generated by cigarette smoking may impair or delay the healing of the annulus fibrosus and posterior longitudinal ligament18 due to nicotine’s effects on nutrition and oxygenation of the disc annulus, as demonstrated by a previous study.19 The prolonged healing time may make the remaining nucleus pulposus more susceptible to relapse from the incomplete or delayed healing of the annulus fibrosus.18 Second, in addition to the pathophysiological changes, smoking can cause repetitive coughing and increase the intervertebral pressure, which may also contribute to rLDH.18
A previous study revealed that SD was related to lower back pain14 and thoracolumbar disc herniation.24 Patients who showed the clinical characteristics of SD were significantly higher in rLDH group (78.79%) than in LDH group (31.46%). Further, logistic regression analysis showed that the risk for rLDH was eight times higher in patients with SD than those without SD. SD is a systemic disease with genetic background in which kyphosis may mainly occur at the thoracic region but the IE and SN can be found throughout the spine region of SD patients.14,24 However, the exact underlying mechanism is not clear. We suspect that the possible reasons may be as follows. First, as widely accepted, IE is one of the main pathologic changes in SD.24 Some researchers have demonstrated that the endplate is the main gateway of nutrient supply to the disc and annulus fibrosus.14 Thus, patients with SD have a weaker endplate and can obtain less nutrition to support the healing of the annulus fibrosus. Secondly, patients with SD have disc lesions, and the disc space collapses existed before the primary surgery. Researchers have demonstrated that the degenerative discs and decreased intervertebral height are risk factors for rLDH.16 Thirdly, if the typical SD occurred at the lumbar region, there will be several WV. The increased local kyphosis can increase the stretching stress on the posterior annulus of the discs,24 which may attribute to rLDH. Fourthly, the healing annulus fibrosus needs collagen to participate in, but the gene related to collagen formation is abnormal,14 which may also attribute to rLDH.
This study has several limitations. First, it was a retrospective study based on the review of medical records; thus, there is a potential risk of bias because of misinterpretation of the descriptions. Second, the study may be biased because both disc herniation and smoking are more common in men than in women. Therefore, it is possible that the results are not a true reflection of the risk. Third, the number of patients in the rLDH group was small, and the research was conducted at a single spine centre, which may reduce the confidence level of the study. Thus, a multi-centre study with a larger sample size should be conducted to further verify the conclusion. Fourth, the authors only focused on 1-year follow-up recurrence; therefore, further research is needed to validate the long-term results.
CONCLUSION
Older age, current smoking status, and SD are risk factors of rLDH. Older patients with radiological characteristics of SD should quit smoking to reduce the likelihood of rLDH occurrence. Further research is needed to determine the potential mechanism of this relationship.
ETHICAL APPROVAL:
The study was approved by the Affiliated Yantai Yuhuangding Hospital of Qingdao University (Approval No. 2020-008).
CONFLICT OF INTEREST:
Authors declare no conflict of interest.
PATIENTS’ CONSENTS:
Written informed consents were obtained from all study participants. The patients’ reported in this study provided informed consents for publication of their data.
AUTHORS’ CONTRIBUTION:
YD: Contributed to study design, data interpretation, and wrote and edited the original draft of the manuscript.
SL: Contributed to conception formulation, data analysis, and manuscript review and critical revision.
GL: Contributed to data analysis and obtainment of ethical approval.
SD: Contributed to data analysis and statistical analysis.
XS: Contributed to data acquisition.
YC: Contributed to conception formulation, study design, critical revision of the manuscript, and final approval of the version to be published.
REFERENCES
- Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: The effects of fragment type and anular competence. J Bone Joint Surg Am 2003; 85(1):102-8.
- Swartz KR, Trost GR. Recurrent lumbar disc herniation. Neurosurg Focus 2003; 15(3):E10.
- Miwa S, Yokogawa A, Kobayashi T, Nishimura T, Igarashi K, Inatani H, et al. Risk factors of recurrent lumbar disk herniation: A single center study and review of the literature. J Spinal Disord Tech 2015; 28(5):E265-9.
- Li Z, Yang H, Liu M, Lu M, Chu J, Hou S, et al. Clinical characteristics and risk factors of recurrent lumbar disk herniation: A retrospective analysis of three hundred twenty-one cases. Spine (Phila Pa 1976) 2018; 43(21):1463-9.
- Suk KS, Lee HM, Moon SH, Kim NH. Recurrent lumbar disc herniation: Results of operative management. Spine (Phila Pa 1976) 2001; 26(6):672-6.
- Yurac R, Zamorano JJ, Lira F, Valiente D, Ballesteros V, Urzúa A. Risk factors for the need of surgical treatment of a first recurrent lumbar disc herniation. Eur Spine J 2016; 25(5):1403-8.
- Shin EH, Cho KJ, Kim YT, Park MH. Risk factors for recurrent lumbar disc herniation after discectomy. Int Orthop 2019; 43(4):963-7.
- Shin BJ. Risk factors for recurrent lumbar disc herniations. Asian Spine J 2014; 8(2):211-5.
- Liu N, Guo X, Chen Z, Qi Q, Li W, Guo Z, et al. Radiological signs of scheuermann disease and low back pain: Retrospective categorization of 188 hospital staff members with 6-year follow-up. Spine (Phila Pa 1976) 2014; 39(20): 1666-75.
- Wood KB, Melikian R, Villami F. Adult scheuermann kyphosis: Evaluation, management, and new developments. J Am Acad Orthop Surg 2012; 20(2):113-21.
- Makurthou AA, Oei L, El Saddy S, Breda SJ, Castaño-Betancourt MC, Hofman A, et al. Scheuermann disease: Evaluation of radiological criteria and population prevalence. Spine (Phila Pa 1976) 2013; 38(19):1690-4
- Gokce E, Beyhan M. Radiological imaging findings of scheuermann disease. World J Radiol 2016; 8(11):895-901.
- Sardar ZM, Ames RJ, Lenke L. Scheuermann's kyphosis: Diagnosis, management, and selecting fusion levels. J Am Acad Orthop Surg 2019; 27(10):e462-e472.
- Palazzo C, Sailhan F, Revel M. Scheuermann's disease: An update. Joint Bone Spine 2014; 81(3):209-14
- Kim KT, Lee DH, Cho DC, Sung JK, Kim YB. Preoperative risk factors for recurrent lumbar disc herniation in l5-s1. J Spinal Disord Tech 2015; 28(10):E571-7.
- Yaman ME, Kazancı A, Yaman ND, Baş F, Ayberk G. Factors that influence recurrent lumbar disc herniation. Hong Kong Med J 2017; 23(3):258-63.
- Meredith DS, Huang RC, Nguyen J, Lyman S. Obesity increases the risk of recurrent herniated nucleus pulposus after lumbar microdiscectomy. Spine J 2010; 10(7):575-80.
- Huang W, Han Z, Liu J, Yu L, Yu X. Risk factors for recurrent lumbar disc herniation: A systematic review and meta-analysis. Medicine (Baltimore) 2016; 95(2):e2378.
- Andersen SB, Smith EC, Støttrup C, Carreon LY, Andersen MO. Smoking is an independent risk factor of reoperation due to recurrent lumbar disc herniation. Global Spine J 2018; 8(4):378-81.
- Kim CH, Chung CK, Park CS, Choi B, Kim MJ, Park BJ. Reoperation rate after surgery for lumbar herniated intervertebral disc disease: Nationwide cohort study. Spine (Phila Pa 1976) 2013; 38(7):581-90.
- Chang HK, Chang HC, Wu JC, Tu TH, Fay LY, Chang PY, et al. Scoliosis may increase the risk of recurrence of lumbar disc herniation after microdiscectomy. J Neurosurg Spine 2016; 24(4):586-91.
- Griffith JF, Wang YX, Antonio GE, Choi KC, Yu A, Ahuja AT, et al. Modified pfirrmann grading system for lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2007; 32(24):E708-12.
- Jansson KÅ, Nemeth G, Granath F, Blomqvist P. Surgery for herniation of a lumbar disc in sweden between 1987 and 1999: An analysis of 27,576 operations. J Bone Joint Surg Br 2004; 86(6):841-7.
- Liu N, Chen Z, Qi Q, Shi Z. The relationship of symptomatic thoracolumbar disc herniation and scheuermann’s disease. Eur Spine J 2014; 23(5):1059-66.