Protective Modifications in Ophthalmology Practice during COVID-19 Pandemic: Challenges and Lessons Learned
By Mohammad Idris1, Eemaz Nathaniel2Affiliations
doi: 10.29271/jcpsp.2021.01.32ABSTRACT
Ophthalmology is a specialty which involves close contact with patients. Personal protective equipment (PPE) along with modifications in examination techniques and equipment are needed to avoid spread of coronavirus infectious disease (COVID-19) to health professionals. This communication aims to highlight and critically analyse the measures suggested to control this spread. We also highlighted our experience with protective gear modifications. As with any practice, triage is cornerstone. Use of disinfectants, good personal hygiene practices and PPE for patients and staff, must be adopted for safe ophthalmology practices.
Key Words: COVID-19, Ophthalmology, Personal protective equipment (PPE).
Ophthalmology involves procedures and use of instruments like slit lamp, auto-refractors and microscopes, which pose a risk of both surgical and respiratory aerosols.1 Besides respiratory route, one of the other possible routes of spread of COVID-19 is via ocular surfaces and tears, posing risk to ophthalmologists. Conjunctivitis may be the first sign of COVID-19 infection well before the appearance of respiratory symptoms. The first death of health professionals, in fact, was of an ophthalmologist from China, Dr. Li Wenliang, who got the infection from an asymptomatic patient.2
Triage system: We devised a useful triage algorithm to select patients using 3Ps to control overcrowding and to maintain social distancing during lengthy eye examination (Figure 1).
Safety in clinic: It includes minimal conversation between patients and attendants, examination with a magnifying glass using an illuminating source (Figure 2) rather than under slit-lamp with glass or hard plastic screen attached to it; in which, one has to come closer to the patient in selected cases. American Academy of Ophthalmology has recommended covering the mouth, nose, and eyes as the deaths of ophthalmologists and otolaryngologists have been reported in several countries.3
Modified use of fundus lenses/ophthalmoscope: Fundus lenses and ophthalmoscopes need frequent disinfection. We adopted an alternative method by using tissue paper with a hole according to the size of the lens rim or ophthalmoscope head; like, we apply Opsite draping before surgery (Figure 3). This least-touch technique added to further safety.
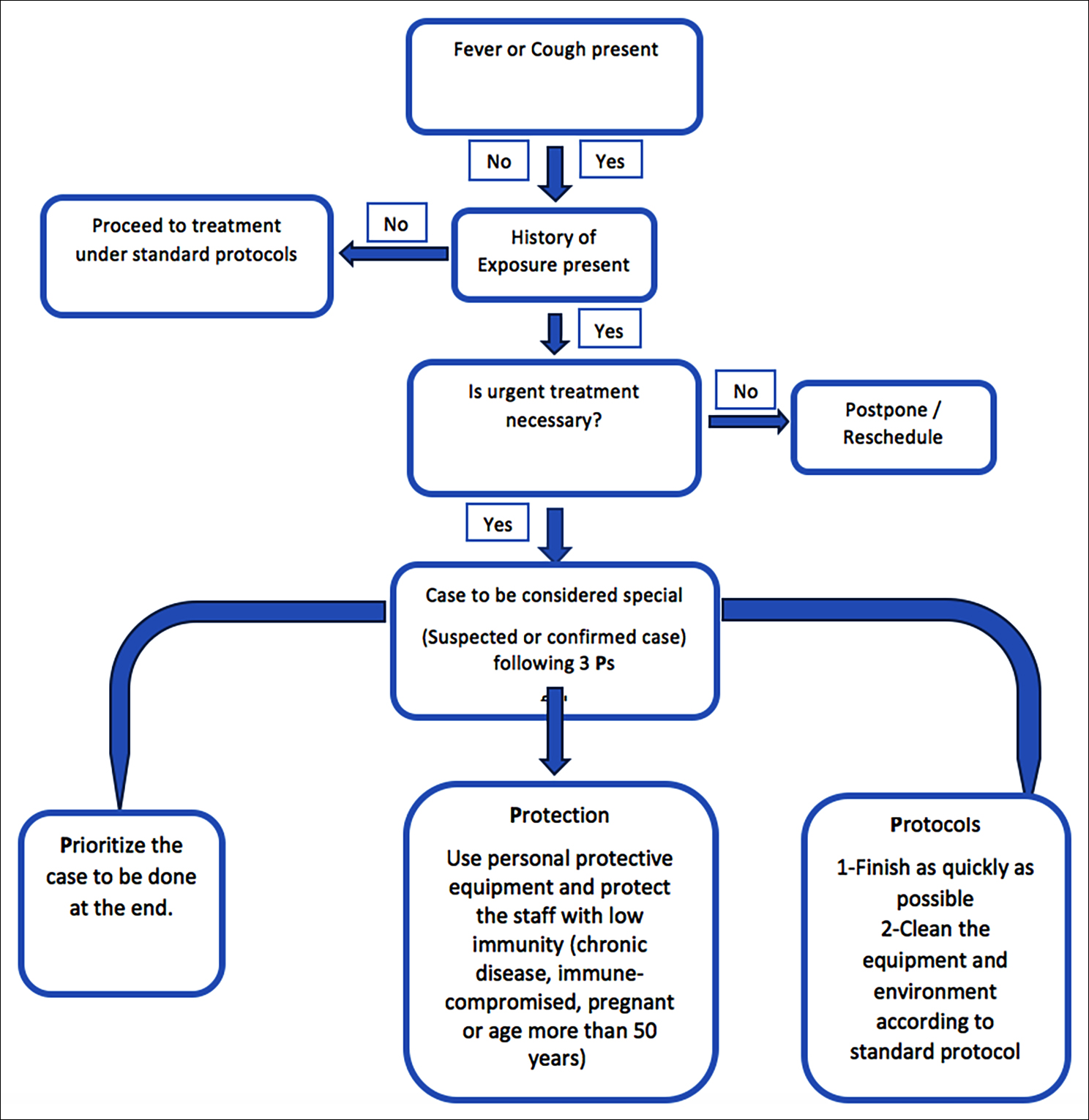 Figure 1: Patient screening algorithm in ophthalmology outpatient clinic.
Figure 1: Patient screening algorithm in ophthalmology outpatient clinic.
 Figure 2: View of right eye through a magnifying glass with illumination held at a distance of 1 metre.
Figure 2: View of right eye through a magnifying glass with illumination held at a distance of 1 metre.
 Figure 3: Tissue paper and plastic sheet with a hole to fit in the fundus lens.
Figure 3: Tissue paper and plastic sheet with a hole to fit in the fundus lens.
Air puff tonometry: It is a non-contact instrument but disrupts the tear film with aerosol generation and spread. Besides preventive steps, placing tonometer in the open area; and the gap between two patients should be more than usual. We suggest the use of a shield into the machine just like in a slit-lamp. The second option is the use of Goldmann tonometer, which is less hazardous.
Modified direct/indirect ophthalmoscopy for emergency cases: Diagnosis of disc swelling in emergency conditions by direct/indirect ophthalmoscopy is important. Positioning plays a vital role in limiting contact. It is preferable to examine patients from the head-end, like ophthalmic surgeons operating in the operating room. Covering the face of the patient with a tissue paper or a piece of plastic with a small hole for visualisation of the fundus may be in place. Both these modifications help reduce the chances of direct contact with the patient, making examination safe.
Problems and challenges in eye clinics: Most of the patients in ophthalmology are either too young or too old, which are difficult cases to assess, as they might not follow instructions properly. Additional precautions with examination should be completed as quickly as possible.4
Rescheduling of patients: Short messaging service (SMS) and telephone calls may be helpful in patient-counselling, treatment and scheduling or rescheduling.
Table I: Challenges faced and solutions for opthalmology practice during COVID-19 pandemic.
|
|
Challenges |
Solutions/suggestions |
|
1 |
Using questionnaires at the triage stage depends totally on the patient or attendant’s true history. In the present situation of fear and uncertainty, the patient or attendant may not give a proper history. |
Counselling of the patient with regard to safety that is needed at the triage. |
|
2 |
Retinal examination involves touching the eyelids. If a patient needs an emergency examination and is COVID-19 positive, it will be very challenging. |
We use disposable tissue paper and a plastic sheet, both with holes equal to the size of the lens/ophthalmoscope. |
|
3 |
Doing eye surgery with a face shield is difficult. An ophthalmic surgeon has to use a microscope or slit-lamp by removing the face shield. It is very difficult to operate with such shields. |
Use of loupe is an alternative option, but it is not possible for emergency repair of cornea or retina. |
|
4 |
Cleaning all the instruments according to WHO guidelines is also a big challenge. There are numerous non-disposable instruments in a single consultant room. Slit-lamp has many parts that need to be cleaned properly for every patient. |
Sufficient time interval between two patients will be needed. A minimum number of patients should be examined. |
|
5 |
Social distancing of 6 feet is impossible in the clinical world and certainly in the small confines of ophthalmic examination lanes. |
One way to practice: It is to have only one person in the room with the patient. |
|
6 |
Some ocular procedures are too lengthy like retinal and oculoplastic procedures with high chances of both surgical and respiratory aerosol spread. In a country like Pakistan, where the availability of proper PPEs is difficult, one must think of the possibility of cross-infection. |
Ophthalmology should be prioritised in provision of PPEs with judicial use. |
|
7 |
Operations under general anesthesia need care and special training. It is better to avoid surgeries performed under general anesthesia; but most of our emergency cases are pediatric trauma cases that must be done under general anesthesia. |
The procedure should be completed as soon as possible. |
|
8
|
Rooms are generally small in ophthalmology. Patients are either too young or old to sit for fundus photo or slit-lamp, so direct/indirect ophthalmoscopy is the only method left. |
Use tissue paper plus plastic sheet to cover eyelid sides to avoid touching eyelid skin with an instrument. |
Role of telemedicine in postoperative care: In our experience, this electronic contact with the patient develops trust between the patient and healthcare provider.
Eye surgery: Only very urgent surgeries like globe perforation, lens-induced glaucoma and fresh retinal detachment surgery are recommended. Ophthalmic surgeons should be aware of involuntary sneeze common with eyelid injections.5 Avoiding the use of loupes or a microscope; and the use of local anesthesia and decreased operative time are the safe strategies.
Educating patients: Hospital official websites should have all guidelines for patients to read before coming to the hospital. As most patients in the developing world have no internet access or they are unaware to internet use,6 we suggest having a large screen in the waiting area with pictorial or video awareness protocols running in a loop.
The challenges and experiences which we faced in the present crisis are summarsed in Table I with some possible suggestions.
CONCLUSION
Ophthalmology is a high-risk specialty due to close (patient/healthcare provider) contact. Proper and necessary patient scheduling as per necessity of ocular examination, time management for patients, use of disinfectants, personal hygiene, and protective measures for patient and staff, must be adopted for safe ophthalmology practices. These important steps towards a safe ophthalmic practice and management will not only be useful in the present wave of infection, but post-pandemic period as a part of the safety manual for ophthalmology professionals.
CONFLICT OF INTEREST:
No conflict of interest was declared by the authors.
AUTHORS’ CONTRIBUTION:
MI: Conceived the review, initiated the literature search, contributed to its draft and coordination.
MI: Conducted literature review, contributed to writing and reviewing the manuscript.
MI, EN: Conducted literature review, and contributed to write-up and critical revision, and approved the final manuscript.
REFERENCES
- Hirschmann MT, Hart A, Henckel J, Sadoghi P, Seil R, Mouton C. COVID-19 coronavirus: Recommended personal protective equipment for the orthopaedic and trauma surgeon. Knee Surg Sports Traumatol Arthrosc 2020; 28(6):1690-8.doi: 10.1007/s00167-020-06022-4.
- Lee KJ. Aao.org. coronavirus-kills-Chinese-whistleblower-ophthalmol. California: American academy of ophthalmology. [cited 2020 Feb 02]. www.aao.org/ headline/coronavirus-kills-chinese-whistleblower-ophthalmol.
- Chen MJ, Chang KJ, Hsu CC, Lin PY, Jui-Ling Liu C. Precaution and prevention of coronavirus disease 2019 infection in the eye. J Chin Med Assoc 2020; 83(7):648-50. doi: 10.1097/JCMA.0000000000000334.
- Xia W, Shao J, Guo Y, Peng X, Li Z, Hu D. Clinical and CT features in pediatric patients with COVID-19 infection: Different points from adults. Pediatr Pulmonol 2020; 55(5):1169-74. doi: 10.1002/ppul.24718.
- Morley AM, Jazayeri F, Ali S, Malhotra R. Factors prompting sneezing in intravenously sedated patients receiving local anesthetic injections to the eyelids. Ophthalmology 2010; 117(5): 1032-6. doi: 10.1016/j.ophtha.2009.09.007.
- Yu AY, Tu R, Shao X, Pan A, Zhou K, Huang J. A comprehensive Chinese experience against SARS-CoV-2 in ophthalmology. Eye Vis (Lond) 2020; 7:19. doi: 10.1186/ s40662-020-00187-2.