Endovascular Treatment of Infra-inguinal Arterial Occlusive Disease in Patients with Diabetes
By Anil Ozen1, Görkem Yiğit1, Bahadir Aytekin1, Mehmet Cahit Saricaoglu2, Ferit Kasimzade1, Hakki Zafer Iscan1Affiliations
doi: 10.29271/jcpsp.2020.11.1180ABSTRACT
Objective: To present the early and mid-term results of PTA for femoropopliteal lesions in diabetic patients, performed by the cardiovascular surgeons.
Study Design: Experimental study.
Place and Duration of Study: Department of Cardiovascular Surgery, Ankara City Hospital, Turkey, from August 2015 to April 2018.
Methodology: Seventy-nine patients with diabetes mellitus (DM) and lower limb arterial occlusive disease underwent endo-interventions causing Rutherford Class 2-5 pedal ischemia. Study end points included ankle brachial index (ABI) and primary patency (PP) evaluated through Kaplan-Meier analyses.
Results: The technical success rate was 92.4% with a mean follow-up period of 13.3 ± 9.2 months. Bailout stenting was required in 27 (34.2%) of the lesions and only 7 (8.9%) patients required percutaneous reintervention at the end of the follow-up period. Kaplan-Meier analysis of the bailout stenting group revealed higher primary patency and lower reintervention rates at 24 months when compared with the PTA group (70.8%, 57.7% and 80.5% 65.9%, respectively).
Conclusion: Endovascular procedures can be performed by cardiovascular surgeons in the early and mid-term with high success and low complication rates in patients with diabetes mellitus.
Key Words: Percutaneous transluminal angioplasty, Endovascular arterial intervention, Diabetes, Femoro-popliteal occlusion, Revascularisation, Lower limb arterial occlusion.
INTRODUCTION
Peripheral vascular disease is more common in diabetic patients.1 There is a possibility of infectious complications and an obstructive disease pattern which occurs more distally and may make endoluminal treatment more difficult. As a result, it is possible that patients with diabetes are more likely to require limb amputations compared to the non-diabetics.2
Patients with chronic limb ischaemia and diabetes mellitus (DM) have a shorter amputation-free survival time than non-diabetic patients with chronic ischemia;3 the 5-year mortality in diabetic patients with chronic limb ischemia is 30%.3,4 Previous studies have shown that patency rates of infrainguinal percutaneous transluminal angioplasty (PTA) are lower in diabetic patients as compared with non-diabetics.
Moreover, DM was found to be an important indicator of loss of the limb.5,6 There are many endovascular treatment approaches available, which need to be evaluated for efficacy.
The aim of this study was to determine the early and mid-term results of PTA for femoropopliteal lesions in diabetic individuals carried out by the cardiovascular surgeons for patency and the need for reinterventions.
METHODOLOGY
It was a single centre, retrospective, single-armed experimental study. Seventy-nine patients with DM, who underwent interventions between August 2015 and April 2018 were included in the study. Adult patients with symptoms of moderate intermittant claudication to diffuse pedal ischemia (Rutherford Class 2 to 5) were eligible for enrollment.
Demographic data were recorded. Preoperative and postoperative ankle brachial index (ABI) were studied. Prior to PTA, all patients were scanned with duplex ultrasound and digital subtraction angiography (DSA). PTAs were performed under local anesthesia with monitorisation by cardiovascular surgeons in the hybrid operating theatre. The study was conducted in accordance with the Helsinki Declaration.
All patients provided written informed consent and the study was approved by the Ethics Commitee of Turkiye Yuksek Ihtisas Training and Research Hospital.
SPSS version 15.0 (SPSS Inc., Chicago, IL, USA) was used for analysis of data. Distribution of continous variables were tested using the Shapiro-Wilk test. Descriptive statistics were presented as median (IQR), with mean ± standard deviation for continuous variables and as number of cases (n) and percentage (%) for nominal variables. Dependent within-group variables (preoperative and postoperative ABIs) were compared using the Wilcoxon test. Kaplan-Meier analyses have been constructed to assess primary patency rates and freedom from reintervention. The p-values below 0.05 were evaluated as statistically significant.
RESULTS
Seventy-nine interventions were performed in 79 patients. The mean age of the study population was 64.1±9.1 (range 33-84 years). The majority (84.8%) of the patients were males. The demographic characteristics of the patients are shown in Table I.
Table I. The demographic characteristics of the patients.
|
Demographical variables |
N |
% |
|
Age (y),Mean ± S.D.Mean |
64.1±9.1 |
|
|
Gender: Male (n) Female (n) |
67 12 |
84.8 15.2 |
|
Hypertension (n) |
51 |
64.6 |
|
Dyslipidemia (n) |
47 |
59.5 |
|
Chronic obstructive pulmonary disease (n) |
14 |
17.7 |
|
Coronary artery disease (n) |
38 |
48.1 |
|
Chronic kidney disease (n) |
6 |
7.6 |
|
Coronary artery bypass grafting (n) |
12 |
15.2 |
|
Current smoker (n) |
55 |
69.6 |
|
Previous percutaneous intervention (n) |
21 |
26.6 |
Table II: Postprocedural details.
|
|
n (%) |
|
Follow-up period (month) |
13.3 ± 9.2 |
|
Complications Hematoma Pseudoaneurysm Infection |
6 (7.6) 3 (3.8) 1 (1.3) 2 (2.5) |
|
Preprocedural ABI Postprocedural ABI |
0.41 (0.35 – 0.48) 0.79 (0.65 – 0.89) |
|
Preprocedural creatinine level |
1.18 ± 1 |
|
Postprocedural creatinine level |
1.28 ± 1.28 |
|
Claudication at control (Rutherford class ≥2) |
18 (22.8) |
|
Freedom from >50% restenosis |
62 (78.5) |
|
Decision after control examination Medical follow-up Surgical intervention Percutaneous intervention |
69 (87.3) 3 (3.8) 7 (8.9) |
|
Values are n (%) or mean ±SD |
|
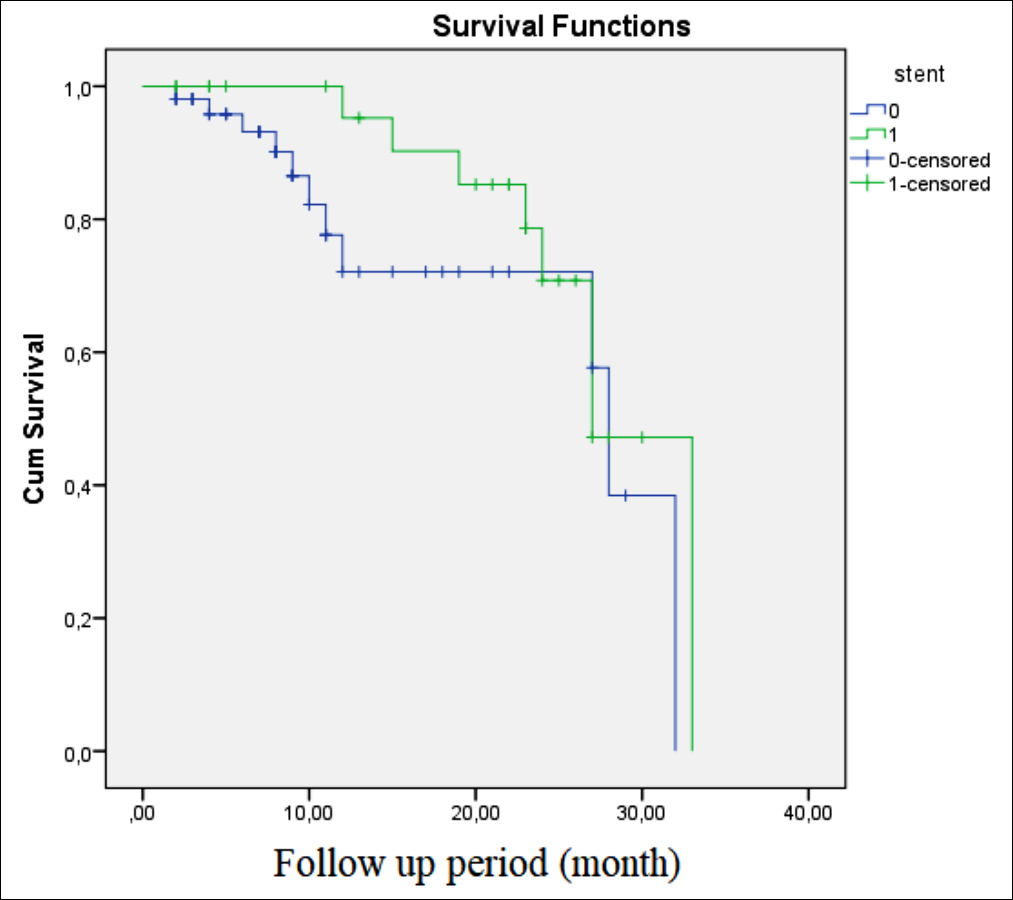 Figure 1 (a): Primary patency rates in bailout stenting group at 24 months (70.8% vs 57.7%, log rank p=0.200).
Figure 1 (a): Primary patency rates in bailout stenting group at 24 months (70.8% vs 57.7%, log rank p=0.200).
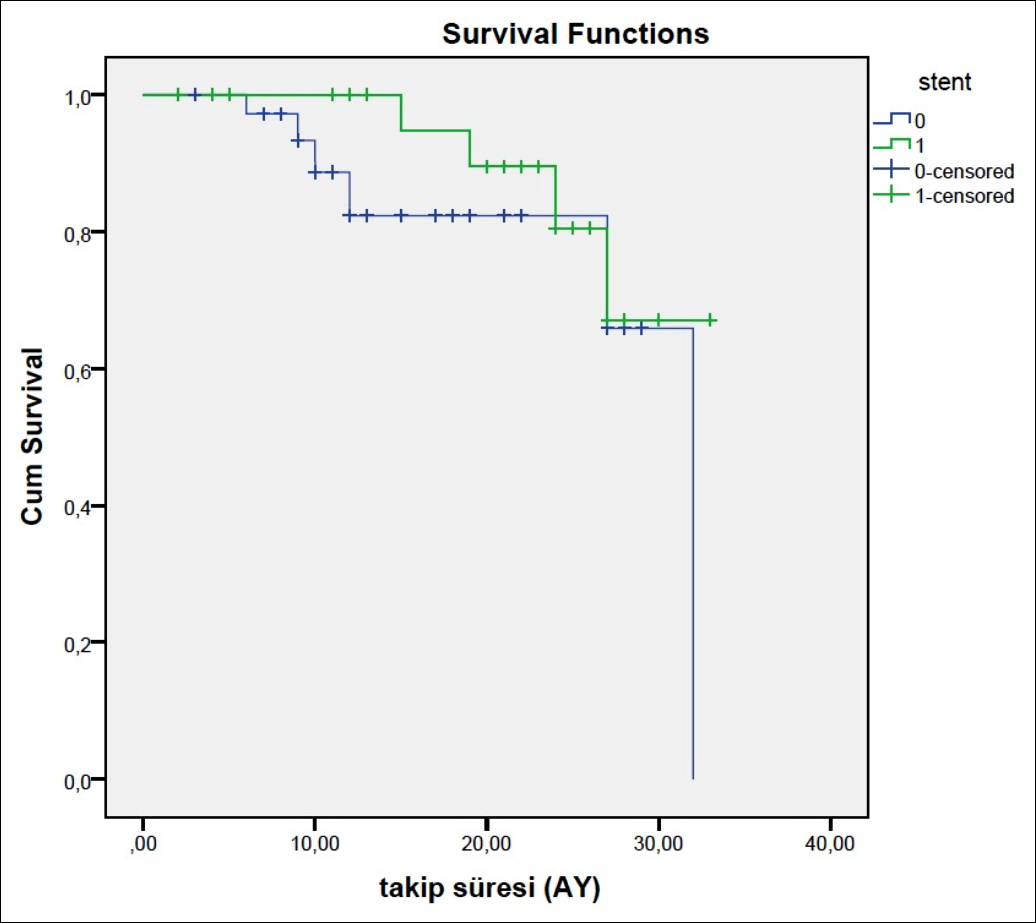 Figure 1 (b): Freedom from reintervention to target lesion rates in bailout stenting group at 24 months (80.5% vs 65.9%, log rank p=0.309).
Figure 1 (b): Freedom from reintervention to target lesion rates in bailout stenting group at 24 months (80.5% vs 65.9%, log rank p=0.309).
The technical success rate of the present study was 92.4% with a mean follow-up period of 13.3 ± 9.2 months. Bailout stenting was required in 27 (34.2%) of lesions and only seven (8.9%) patients needed percutaneous reintervention by the end of the follow-up. Although all patients were preoperatively symptomatic and had claudication, 78.9% of the patients had mild symptoms or were asymptomatic at the end of the follow-up. ABIs were improved significantly in the postprocedural period (p <0.001). During the follow-up, there were no deaths and no amputations were performed. None of the patients withdrew their consent or were lost to follow-up. Postprocedural details are shown in Table II.
Out of the 79 patients, 32 (40.5%) had TASC B lesions; whereas, 29 (36.7%) had TASC A lesions. Furthermore, 16 (20.3%) had TASC C and only two (2.5%) had type D lesions.
Most of the lesions were located at the proximal part of the SFA (63 patients). This was followed by the distal part of the SFA (30 patients). Moreover, 11 patients had lesions located at the popliteal region and only seven had lesions located at the CFA.
The lesion length was 5-10 cm in 23 (29.1%) patients, 10-15 cm in 17 (21.5%) patients, 15-20 cm in 23 (29.1%) patients, 20-25 cm in 12 (15.2%) patients, and longer than 25 cm in only 4 (5.1%) patients.
Kaplan-Meier analysis revealed higher primary patency (70.8%, 57.7%, log rank p=0.200) (Figure 1-a) and freedom from reintervention to target lesion rates in the bailout stenting group at 24 months (80.5% , 65.9%, log rank p=0.309) (Figure 1-b). Although the primary patency rate and freedom from reintervention rate of the bailout stenting group were higher than the PTA group by the end of 24 months, these differences were not statistically significant (p >0.005) according to the Kaplan-Meier analysis.
DISCUSSION
Diabetes mellitus is an important risk factor for PAD that leads to increased mortality and morbidity as well as increased disease course.7 Recently, in many centres, the endovascular approach has been gaining momentum in the treatment of peripheral arterial disease of the lower limbs.8,9 In addition to advances in endovascular technology, surgeons have rapidly gained endovascular surgical skills with good results.10,11
At the study centre, percutaneous revascularisation procedures have been developed in the last five years as primary modality to treat occlusive disease of the lower extremity, with primary surgical bypass devoted to patients failing percutaneous intervention. According to the present results, diabetic individuals showed a decreased primary patency rate (70.8%). This is in agreement with the studies of Black et al. and Ryer et al, supporting that diabetes is an independent indicator of the failure of percutaneous lower extremity attempts.9,12
Although all patients were symptomatic and had claudication prior to intervention, 78.9% of the patients became mildly symptomatic or asymptomatic at the end of the follow-up. ABIs were improved significantly in the postprocedural period.
In a retrospective study after primary PTA in the femoropopliteal segment of lower extremity,13 Lazaris et al. found that technical success rate was decreased to 81% in diabetic patients compared to 93% in non-diabetic patients.13 In addition, they also found increased complication rate in diabetic patients compared to non-diabetics (16.7% , 3.9%), including five cases of arterial perforation, four cases of emergency bypass, and two cases each of reangioplasty and amputation. The technical success rate in the present study was 92.4% with a mean follow-up period of 13.3 ± 8.9 months. Three patients developed hematomas (3.8%) whilst two developed infections (2.5%), and one patient developed pseudoaneurysm of the femoral artery (1.3%). Furthermore, three patients (3.8%) underwent open surgery. Nevertheless, the authors did not come across with any cases of amputations. This may be a result of lower number of patients and shorter follow-up period when compared to other studies.
DeRubertis et al. determined that diabetic patients were more likely to tend to primary failure, thus resulting in a 20.7% reintervention rate and 23.1% percutaneous failure rate, compared with non-diabetics.6 As for this present study, bailout stenting was required in 27 (34.2%) of lesions and only 7 (8.9%) patients needed percutaneous reintervention at the end of the follow-up. The lower ratio of reintervention in this study may be due to the shorter period of follow-up compared to the study of DeRubertis et al.6
In an enrollment of 219 interventions that underwent PTA, Clark et al. determined diabetes to be considerably related with decreased primary patency.14 On the contrary, Baril et al. examined fundamentally claudicants with TASC II classification of femoropopliteal lesions and did not find a relationship between diabetes and restenosis, similar to the present results.15 This present study also revealed no association between diabetes and restenosis according to TASC II classification of femoropopliteal lesions. Moreover, Kaplan-Meier analysis revealed primary patency and freedom from reintervention to target lesion rates as higher in the bailout stenting group at 24 months (70.8% , 57.7% and 80.5% , 65.9%).
The limitations of this study contain its retrospective formation and limited number of patients. However, the authors present these results as cardiovascular surgeons performing PTAs for the last five years, and believe that surgeons should be encouraged to get even more involved in this field.
CONCLUSION
Endovascular interventions can be performed by cardiovascular surgeons in the early and mid-term with high success and low complication rates in patients with diabetes mellitus. Surgeons should be encouraged to participate more in endovascular treatment.
ETHICAL APPROVAL:
Ethics Committee approval was received from Turkiye Yuksek Ihtisas Training and Research Hospital Ethics Commitee.
PATIENTS’ CONSENT:
As the study was designed retrospectively, data was collected from clinical archive after ethical approval.
CONFLICT OF INTEREST:
Authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
AÖ, GY: Study design, data collection, literature review and writing.
MCS: Drafting of work.
FK: Statistical analysis and literature review.
BA, MCS: Data collection.
HZİ: Final review and approval of article.
All authors approved final version of the manuscript.
REFERENCES
- King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care 1998; 21(9):1414-31. doi: 10.2337/ diacare.21.9.1414.
- Jude EB, Oyibo SO, Chalmers N, Boulton AJ. Peripheral arterial diseasein diabetic and nondiabetic patients: A comparison of severity and outcome. Diabetes Care 2001; 24(8):1433-7. doi: 10.2337/diacare.24.8.1433.
- Malmstedt J, Leander K, Wahlberg E, Karlstrom L, Alfredsson L, Swedenborg J, et al. Outcome after leg bypass surgery for critical limb ischemia is poor in patients with diabetes: a population-based cohortstudy. Diabetes Care 2008; 31(5):887-92. doi: 10.2337/dc07-2424.
- Faglia E, Clerici G, Clerissi J, Gabrielli L, Losa S, Mantero M, et al. Early and five-year amputation and survival rate of diabetic patients with critical limb ischemia: Data of a cohort study of 564 patients. Eur J Vasc Endovasc Surg 2006; 32(5):484-90. doi: 10.1016/j.ejvs.2006.03.006.
- Bakken AM, Palchik E, Hart JP, Rhodes JM, Saad WE, Davies MG, et al. Impact of diabetes mellitus on outcomes of superficial femoral arteryendoluminal interventions. J Vasc Surg 2007; 46(5):946-58. doi: 10.1016/j.jvs.2007.06.047.
- DeRubertis BG, Pierce M, Ryer EJ, Trocciola S, Kent KC, Faries PL, et al. Reduced primary patency rate in diabetic patients after percutaneous intervention results from more frequent presentation with limb-threatening ischemia. J Vasc Surg 2008; 47(1):1018. doi: 10.1016/ j.jvs.2007. 09.018.
- Thiruvoipati T, Kielhorn CE, Armstrong EJ. Peripheral artery disease in patients with diabetes: Epidemiology, mechanisms, and outcomes. World J Diabetes 2015; 6(7): 961-9. doi: 10.4239/wjd.v6.i7.961
- Kudo T, Chandra FA, Kwun WH, Haas BT, Ahn SS. Changing pattern of surgical revascularisation for critical limb ischemia over 12 years: Endovascular vs. open bypass surgery. J Vasc Surg 2006; 44(2):304-13. doi: 10.1016/ j.jvs.2006.03.040.
- Black JH, LaMuraglia GM, Kwolek CJ, Brewster DC, Watkins MT,Cambria RP, et al. Contemporary results of angioplasty-based infrainguinal percutaneous interventions. J Vasc Surg 2005; 42(5):932-9. doi: 10.1016/j.jvs.2005.06.024.
- Uğur M, Alp İ, Arslan G, Şenay Ş, Selçuk İ, Selçuk A, et al. Vasküler hastalıkların yönetiminde endovasküler ve hibrid uygulamalar: Kardiyovasküler cerrahi kliniği deneyimleri. Turk Gogus Kalp Dama 2012; 20:230-42.
- Temizkan V, Uçak A, Alp İ, Kardeşoğlu E, Selçuk A, Can MF, et al. Our experiences on endovascular and hybrid treatment of peripheral arterial diseases. Turk Gogus Kalp Dama 2018; 26(2):237-45. doi: 10.5606/tgkdc.dergisi. 2018.13411.
- Ryer EJ, Trocciola SM, Derubertis B, Lam R, Hynecek RL, Karwowski J, et al. Analyses of outcomes following failed endovascular treatment ofchronic limb ischemia. Ann Vasc Surg 2006; 20(4):440-6.
- Lazaris AM, Tsiamis AC, Fishwick G, Bolia A, Bell PR. Clinical outcome ofprimary infrainguinal subintimal angioplasty in diabetic patients with criticallower limb ischemia. J Endovasc Ther 2004; 11(4):447-53. doi: 10.1583/03- 1159.1.
- Clark TW, Groffsky JL, Soulen MC. Predictors of long-term patency after femoropopliteal angioplasty: results from the STAR Registry. J Vasc Interv Radiol 2001; 12:923-33. doi: 10.1583/03-1159.1.
- Baril DT, Marone LK, Kim J, Go MR, Chaer RA, Rhee RY, et al. Outcomesof endovascular interventions for TASC II B and C femoropopliteal lesions. J Vasc Surg 2008; 48(3): 627-33. doi: 10.1016/j.jvs.2008.04.059.