Effect of Differences in Thorax Volume and Dimensions on CPR-related Injuries
By Nihat Mujdat Hokenek1, Mehmet Ozgur Erdogan2Affiliations
doi: 10.29271/jcpsp.2021.03.267ABSTRACT
Objective: To investigate the relationship between the prevalence of cardiopulmonary resuscitation (CPR) related thoracic injury and patients’ thoracic volume and dimensions.
Study Design: Observational study.
Place and Duration of Study: Kartal Dr. Lütfi Kırdar City Hospital, İstanbul, Turkey, from August 2015 to August 2019.
Methodology: Patients, who were in hospital due to a non-traumatic cause, had experienced cardiac arrest and subsequently had a post-CPR thorax tomography, were included in the study. Thorax dimensions were measured on sagittal, transverse, and longitudinal axes, while thorax volumes were calculated using a 3D computer programme. This data was later compared to trauma findings.
Results: A total of 246 patients were included in the study. The sagittal measurements ranged from 130 – 302 mm, with an average of 228.42 ± 25.61 mm; the transverse measurements ranged from 160-293 mm, average 238.60 ± 22.25 mm, and longitudinal measurements ranged from 99-259 mm, average 187.94 ± 29.76 mm; while thorax volumes were between 4670 – 21512 cc, with an average of 10118.19 ± 2438.01 cc. Trauma was present in 34.1% of patients. Sagittal, longitudinal dimensions, and thorax volume were lower for the group positive for trauma compared to the non-trauma group (p=0.019, p=0.023 and p=0.002). Thorax volume and longitudinal dimensions were found to be lower in patients who experienced rib fractures (p=0.021, p<0.05). Sagittal dimensions were also found to be significantly lower in the group with pneumothorax (p<0.05).
Conclusion: Lower thorax volume and sagittal dimensions were associated with an increased prevalence of traumatic findings.
Key Words: Cardiopulmonary resuscitation, Thoracic injuries, Pneumothorax, Rib fracture.
INTRODUCTION
Despite being in use for around 60 years, the details of the closed-chest cardiac massage CPR method are still disputed.1-3 Nevertheless, the primary component of CPR remains chest pressure applied to patients experiencing cardiac arrest.3,4 Applying this technique, allows CPR to provide cardiac output to the body. Contemporary CPR guidelines advise chest compressions of a specific number and depth.3,4 According to the European Resuscitation Council (ERC) CPR 2015 and 2020 manual, the recommended chest compression depth is 5 – 6 cm, with a range of between 100 – 120 compressions per minute.3,4 Iatrogenic injuries may result due to the pressure applied to the thorax.5-7 While myriad complications may develop as a result of CPR, the most common injuries include those such as rib fracture or sternal fracture.8,9
While CPR related injuries pose a threat to hemodynamic stability, progressive traumatic findings have been found to decrease the chance of circulation normalising.9 As such, minimising risk of trauma during CPR is likely to ease return of spontaneous circulation (ROSC). If variations in thoracic dimensions and volume can be associated with trauma from the application of chest compressions with a depth of 5 – 6 cm, a case can be made for the necessity of personalised CPR.
In particular, we were unable to identify any study in the literature that analysed post-CPR patients’ thoracic dimensions and volume, using a 3D computer programme; and subsequently, investigated the relationship between these parameters and presence of trauma.
The primary aim of this study was to evaluate whether patients’ variations in thoracic volume and dimensions were associated with any difference in trauma outcomes after application of CPR with standard compression depth and to evaluate the relationship between specific injury types and measurements, as well as various other variables such as CPR duration, gender, and age.
METHODOLOGY
This study was designed retrospectively with approval from the Ethics Committee of Kartal Dr. Lutfi Kirdar City Hospital (No. 2019/514/162/1). This retrospective observational cohort analysis used data from adult patients, who were successfully resuscitated in hospital following cardiac arrest without a traumatic cause.
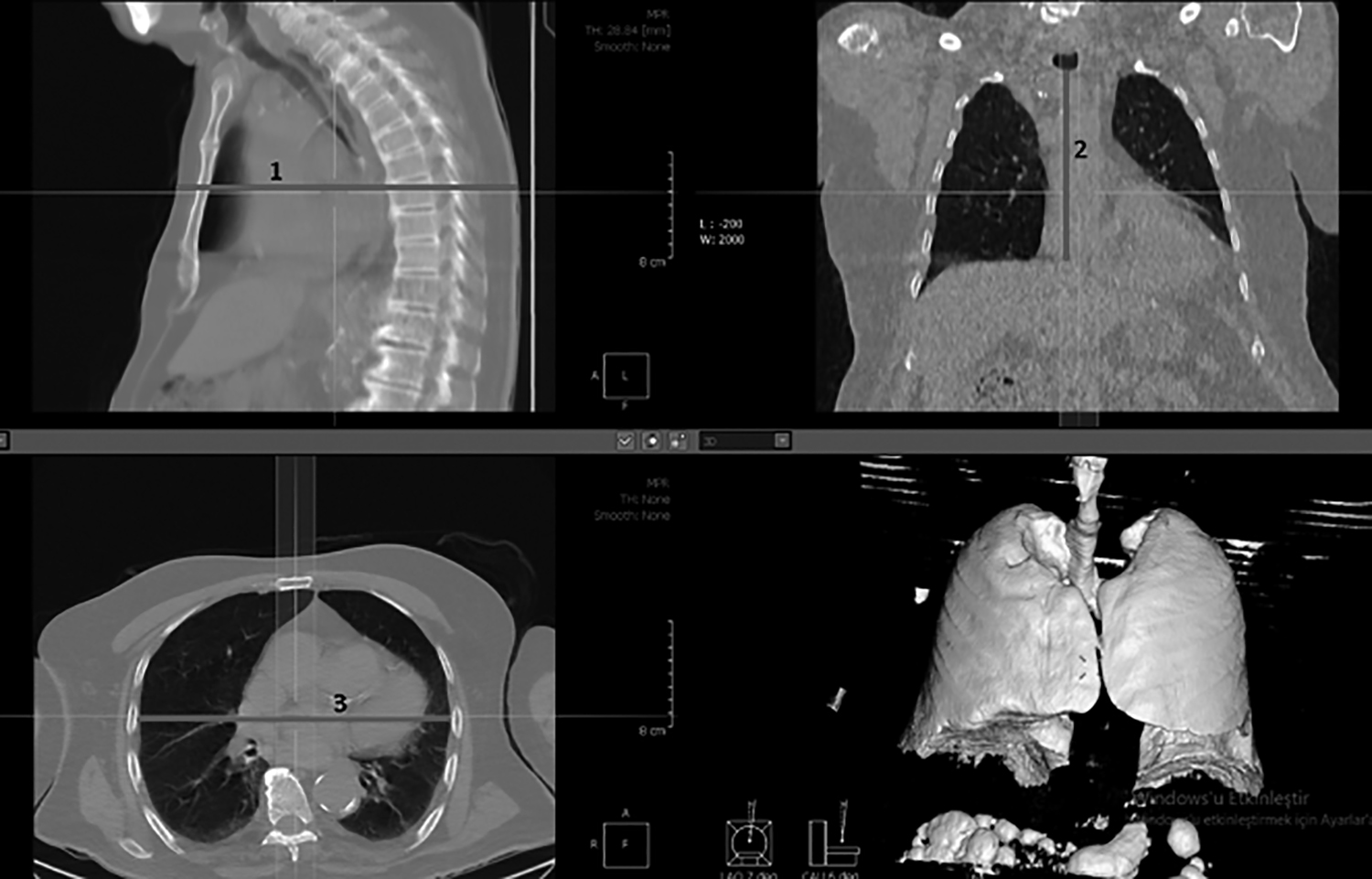 Figure 1: Sagittal diameter (1) in sagittal axis, longitudinal diameter (2) measured in coronal axis and transverdiamaer (3) by axial axis.
Figure 1: Sagittal diameter (1) in sagittal axis, longitudinal diameter (2) measured in coronal axis and transverdiamaer (3) by axial axis.
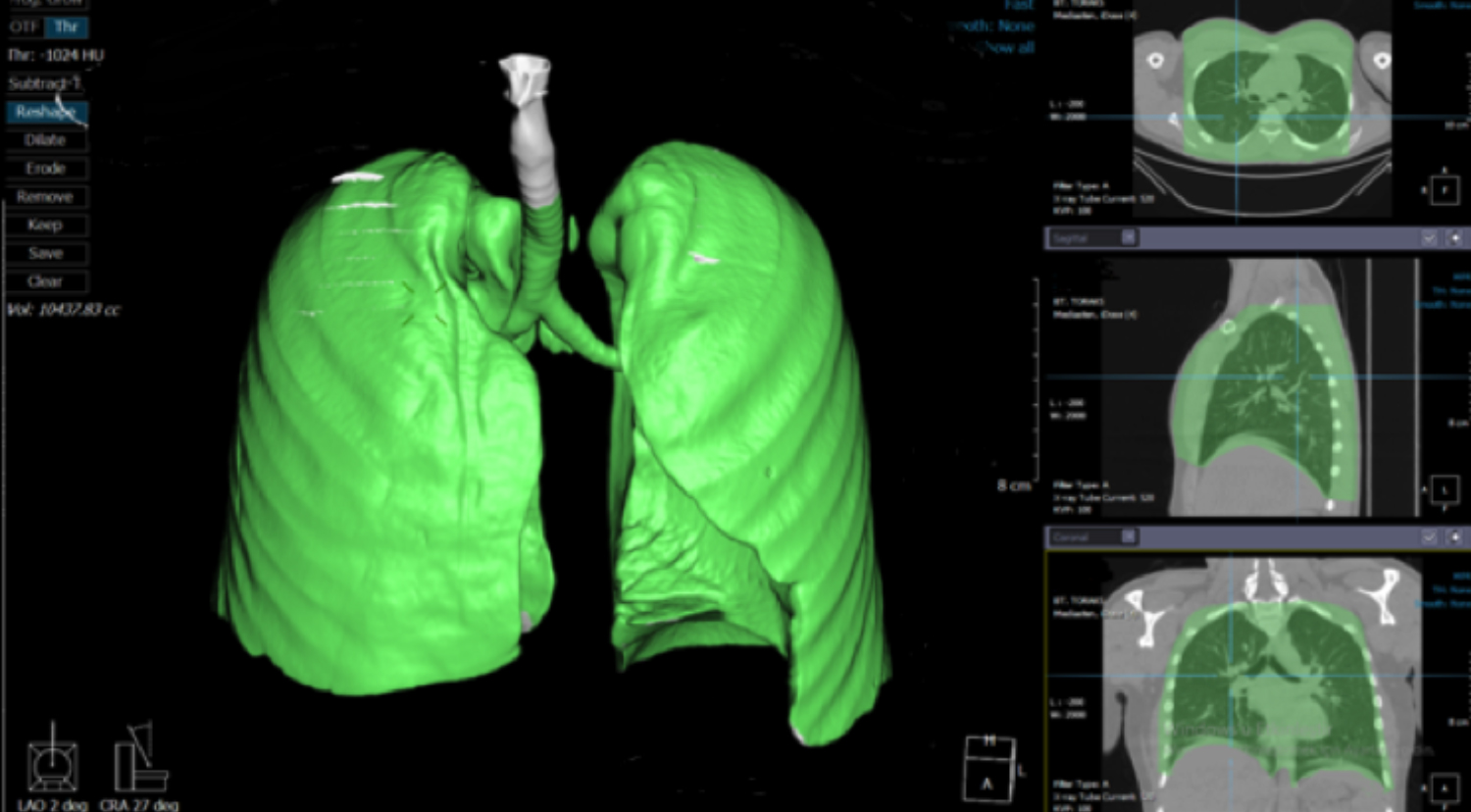 Figure 2; The image produced by the Xelis 3D programme used to measure thorax volume. The highlighgted tissues’ total volume is automatically displayed in the centre of the left edge of the screen.
Figure 2; The image produced by the Xelis 3D programme used to measure thorax volume. The highlighgted tissues’ total volume is automatically displayed in the centre of the left edge of the screen.
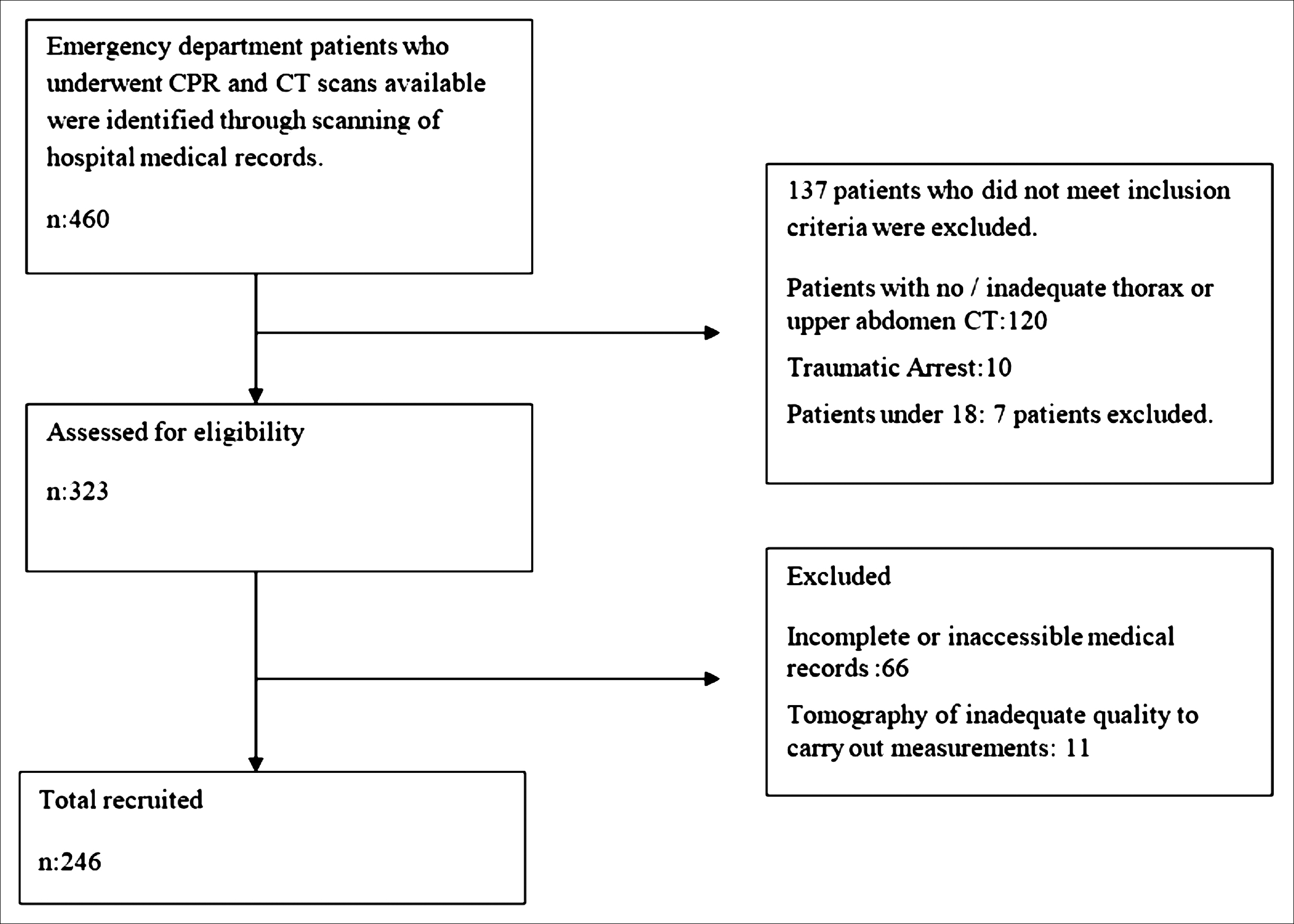 Figure 3: Flowchart of the study.
Figure 3: Flowchart of the study.
Table I: Descriptive characteristics’ distributions.
|
|
|
n (%) |
|
Age (years) |
Min-Max (Median) |
19-103 (75) |
|
Average ± SD |
72.98 ± 15.97 |
|
|
Gender |
Female |
100 (40.7) |
|
Male |
146 (59.3) |
|
|
CPR duration |
Min-Max (Median) |
1-90 (15) |
|
Average ± SD |
22.95 ± 19.57 |
|
|
Sagittal |
Min-Max (Median) |
130-302 (229) |
|
Average ± SD |
228.42 ± 25.61 |
|
|
Transverse |
Min-Max (Median) |
160-293 (240) |
|
Average ± SD |
238.60 ± 22.25 |
|
|
Longitudinal |
Min-Max (Median) |
99-259 (189) |
|
Average ± SD |
187.94 ± 29.76 |
|
|
Thoracic volume |
Min-Max (Median) |
4670-21512 (9706.5) |
|
Average ± SD |
10118.19 ± 2438.02 |
|
|
Trauma Rib fracture |
|
84 (34.1) |
|
|
48 (19.5) |
|
|
Sternum fracture Scalpula fracture |
|
12 (4.9) |
|
|
5 (2.0) |
|
|
Pulmonary contusion |
|
10 (4.1) |
|
Pneumothorax |
|
15 (6.1) |
|
Cardiac tamponade |
|
1 (0.4) |
|
Subcutaneous emphysema |
|
11 (4.5) |
|
Myocardial hematoma/rupture |
|
1 (0.4) |
|
Vertebral fracture |
|
1 (0.4) |
The study was conducted on patients admitted to Kartal Dr. Lütfi Kirdar City hospital between August 2015 and August 2019, with a total duration of 4 years. Patients admitted for non-traumatic causes, which underwent CPR for cardiac arrest and had a CT scan, were included in the study.
The hospital database was scanned retrospectively for patients who underwent CPR and had ROSC with subsequent CT scans. Patients whose cause of cardiac arrest was traumatic, had incomplete medical records, did not have a CT scan, were under 18, or whose CT scan was of insufficient quality to make accurate measurements, were excluded from the study. All patients included were intubated, in the supine position, and supported by a transport ventilator. No mechanical compressors were used in the study.
Patients were evaluated for age, gender, trauma type (rib fracture, sternum fracture, clavicula fracture, scapula fracture, flail chest, costochondral joint pain, pulmonary contusion, pneumothorax, hemothorax, cardiac tamponade, subcutaneous emphysema, myocardial hematoma/rupture, and vertebral fracture), and CPR duration.
Table II: The relationship of descriptive features and tomography measurements with the presence / absence of trauma.|
|
Trauma (-) (n=162) |
Trauma (+) (n=84) |
p |
|
|
Age (years) |
25th-75th percentiles (Median) |
64.0-75.0 (75) |
65.3-86.8 (75.5) |
b0.944 |
|
Average±SD |
73.15 ± 15.39 |
72.65 ± 17.14 |
||
|
Gender n (%) |
Female |
59 (36.4) |
41 (48.8) |
c0.061 |
|
Male |
103 (63.6) |
43 (51.2) |
||
|
CPR |
25th-75th percentiles (Median) |
5.0-35.0 (15) |
5.0-42.3 (20) |
b0.478 |
|
Average±SD |
22.53 ± 20.14 |
23.76 ± 18.52 |
||
|
Sagittal |
25th-75th percentiles (Median) |
214.0-246.0 (231) |
202.5-244.0 (222.5) |
a0.019* |
|
Average±SD |
231.17 ± 24.15 |
223.13 ± 27.60 |
||
|
Transverse |
25th-75th percentiles (Median) |
227.3-255.0 (240.5) |
215.5-257.5(236) |
a0.128 |
|
Average±SD |
240.28 ± 20.21 |
235.37 ± 25.54 |
||
|
Longitudinal |
25th-75th percentiles (Median) |
172.5-210.3 (194) |
159.3-201.8 (182) |
b0.023 |
|
Average±SD |
190.53 ± 30.14 |
182.95 ± 28.51 |
||
|
Thorax volume |
25th-75th percentiles (Median) |
8830.5-11671.3 (9874) |
7359.0-11179.8 (9307.5) |
b0.002* |
|
Average±SD |
10475.97 ± 2433.54 |
9428.18 ± 2307.83 |
||
|
aStudent t Test; bMannWhitney U Test; cPearsonChi-Square Test; *p<0.05 |
||||
Table III: Distribution of other analysis.
|
|
Pulmonary contusion + n=10 |
Pulmonary contusion – n=236 |
Pnuemothorax + n=15 |
Pneumothorax – n=231 |
Rib fracture n=48 |
Rib fracture n=198 |
p |
|
|
Sagittal |
25th-75th percentiles (Median) |
212.3-245.0 (230) |
198.8-221.3 (212) |
|
|
|
|
b0.040 |
|
|
Average ± SD |
228.98 ± 25.61 |
215.30 ±23.03 |
|
|
|
|
|
|
|
25th-75th percentiles (Median) |
|
|
191-224 (202) |
213-245 (230) |
|
|
a0.004 |
|
|
Average ± SD |
|
|
210.07±23.68 |
229.61±25.32 |
|
|
|
|
Longitudinal |
25th-75th percentiles (Median) |
|
|
|
|
159-200.5 (173.5) |
169-210.3 (191) |
b0.013 |
|
|
Average ± SD |
|
|
|
|
179.38±26.36 |
190.02±30.22 |
|
|
Thorax vol |
25th-75th percentiles (Median) |
|
|
|
|
7219.8-11385 cc (9062) |
8756.3-11477.8 cc (9759) |
b0.021 |
|
|
Average ± SD |
|
|
|
|
9353.04±2487.91 |
10303.68±2395.46 |
|
|
aIndependent sample t-test, bMann-Whitney U-test. |
||||||||
Thorax dimensions were measured using a computer programme. These measurements took the midsternum as a reference point and included skin-to-skin distance on the sagittal axis and midthoracic transverse distance. Sagittal diameter was defined as the anteroposterior distance from the skin on the anterior chest wall to the skin on the back in the transverse section on the midsagittal line. Tranverse distance was measured from the inner surface of the rib to the inner surface of the opposite rib. Additionally, patients’ longitudinal diameter was defined as the distance from the incisurajugularis to the end of the xiphoid process, as measured from the midthorax on the longitudinal axis (Figure 1). Finally, patients’ thoracic volumes were measured using a 3D computer programme (Xelis 3D). This programme can accurately identify the volume and dimensions of the even smallest nodule of any organ.10,11
Tomography scans were evaluated by a radiologist. Each patient was analysed with the 16-channel Siemens Emotion 16 CT scanner. The infinitt picture archiving and communication systems (PACS) software was used to evaluate the tomography scans. Thoracic volumes were calculated using the post-process programme in Xelis 3D Imaging Software (Infinitt Healthcare, Korea). Thorax volume was measured using two methods within this software. To assess the density of tissues, the threshold was initially set as minus 1024, which ensured that all tissue components were included. Subsequently, the inferior border of the thorax was defined as the upper border of the diaphragm, while ensuring that the lateral costas were included. Furthermore, the superior border was defined as the C7 – C8 intervertebral space. Accordingly, the upper margin was drawn in a circular manner following the first costa in order to include the whole cavity (Figure 2).
The borders were manually selected when measuring thorax volumes. Though likely trivial, this did introduce a certain amount of subjectivity and thus potential margin of error. Sample size was determined according to the number of cases within 4 years, while taking similar papers’ populations as a base.12
The included patients were separated into two groups: traumatic and non-traumatic patients. Thoracic measurements of each group were evaluated to identify any potential differences. After this, patients were divided into individual subgroups, according to the specific type of traumatic injury, with these subgroups again being analysed in terms of relationship to thoracic measurements.
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) software, version 20.0. Descriptive statistical methods were used, while evaluating research data (average, standard deviation, median, frequency, ratio, 25th percentile, 75th percentile). Quantitative data was evaluated for fit to a normal distribution using the Shapiro-Wilk test, and subsequently evaluated graphically. Normally distributed data was evaluated using the Student’s t-test, when comparing two groups; while the Mann-Whitney U-test was used in comparisons of two groups of non-normally distributed data. Qualitative data was compared using the Pearson’s Chi-squared test. A significance threshold of p<0.05 was used.
RESULTS
The hospital database was scanned for patients admitted between August 2015 and August 2019 who underwent CPR and had a thorax CT available. These patients were subsequently contacted. One hundred and thirty-seven patients, whose medical records did not fit the inclusion criteria as well as patients who had incomplete records or a tomography of insufficient quality for measurement, were excluded. The study was carried out on the remaining 246 patients. A flowchart of the patients’ inclusion/exclusion process is displayed in Figure 3.
The study was carried out on 246 patients admitted to Kartal Dr. Lutfi Kirdar City Hospital Emergency Department between 2016 and 2019, of which 40.7% (n=100) were women, while 59.3% were men (n=146). While patients’ ages ranged from 19 to 103, the average age was 72.98 ± 15.97 years. The detailed data is displayed in Table I.
CPR durations ranged from between 1 and 90 minutes, with an average of 22.95 ± 19.57 minutes. Sagittal measurements varied between 130 mm and 302 mm, averaging 228.42 ± 25.61 mm. Tranverse measurements were between 160 mm and 293 mm, with an average of 238.60 ± 22.25 mm. Longitudinal measurements ranged from 99 mm to 259 mm, with an average of 187.94 ± 29.76 mm. Thorax volumes ranged from 4670 cc to 21512 cc, with an average of 10118.19 ± 2438.02 cc.
Trauma was present in 34.1% (n=84) of cases. When tomography results were analysed according to traumatic pathology, rib fractures (19.5%, n=48), sternum fractures (4.9%, n=12), scapula fractures (2.0%, n=5), pulmonary contusions (4.1%, n=10), pneumothorax (6.1%, n=15), cardiac tamponade (0.4%, n=1), subcutaneous emphysema (4.5%, n=11), myocardial hematoma/rupture (0.4%, n=1), and vertebral fractures (0.4%, n=1) were identified.
No statistically significant differences were found between the trauma and non-trauma groups in terms of average age, gender, CPR duration, or transverse measurements (p>0.05, Table II).
Sagittal, longitudinal dimensions and thorax volume were found to be significantly lower in the trauma group compared to the non-trauma group (p=0.019, p=0.023, and p=0.002, respectively).
In this study, the primary purpose was to evaluate the difference between trauma outcomes in the two groups. Secondarily, when group variables were analysed according to type of trauma, some other results were found. For example, when patients were split into groups according to rib fracture (n=48) or no-rib fracture (n=198), longitudinal measurements were found to be significantly lower in the group that experienced rib fractures (p=0.013). Likewise, thorax volumes were found to be significantly lower in the rib fracture group (p=0.021). When split into two groups according to presence of pneumothorax, sagittal measurements were found to be significantly lower in the pneumothorax group (p=0.004). Similarly, when grouped according to development of pulmonary contusions, sagittal measurements were yet again found to be lower in the pneumothorax positive group (p=0.040). The significant results are summarised in Table III. Other analyses resulted in no statistically significant results.
DISCUSSION
This study is the first in the literature to analyse the relationship between CPR related iatrogenic injuries in in-hospital cardiac arrest patients with thoracic volume and dimension measurements.
CPR can be resulted in life-threatining serious injuries.13-15 Evaluation of these injuries by using computer tomography has benefits to true diagnose.12,16
According to these results, CPR-related trauma was found to be significantly higher in patients with lower thorax volumes and sagittal measurements (p=0.002, p<0.05). Increased depth of cardiac pressure may be related to the development of injuries. The 2015 and 2020 ESC guidelines defined a range of depth of 5 – 6 cm for chest compressions to address this issue.2,3 The limitation to a maximum of 6 cm, while potentially reducing the incidence of thoracic injuries, may still cause serious thoracic injury in patients with low thoracic diameters and volumes.
A previously conducted study showed that 50 – 60 mm depth of chest compressions was associated with a higher rate of traumatic injuries when compared to earlier guidelines.17 Another study showed that 40.3 – 55 mm depth was the optimal range in order to minimize injury in patients.5 It is proposed that variations in patients’ anatomy and proportions should be taken into account when debating the optimal range. The results of the present study suggest that use of individualized compression depths may decrease the risk of traumatic injury.
In a separate CPR study conducted on 274 patients with an average age of 62.7±15.1 years, increasing age and CPR duration was found to be significantly correlated with risk of skeletal chest injuries.18 The present results found that there was no significant difference in injuries according to CPR duration or age (p>0.05). The authors attribute this finding to the fact that the population consisted of in-hospital patients of advanced age (72.98±15.97 years).
This study results point to CPR related trauma being significantly more common in patients with lower thorax volumes and sagittal measurements (p=0.002, p<0.05). Use of compressions of a lower depth in patients with smaller thorax dimensions and volume may decrease CPR-related injury and subsequently mortality from thorax trauma. If a system is developed to produce individualised CPR routines that provide optimum cardiac output with compression depths that present minimal risk of trauma, improvements in ROSC and normalisation of hemodynamics will likely improve survival in patients.
The use of lower depth chest compressions has been shown to be effective in children, a patient group with similarly smaller thorax dimensions and volume.19,20 Accordingly, it could be assumed that lower depth CPR could be effective in adult patients with smaller thorax dimensions and volumes. Furthermore, a fear of injuring patients with deep compressions may cause incompliance with recommendations and use of inappropriately shallow compressions. Ideal compression depth should be determined according to individual patients and, while it should provide sufficient circulation to support ROSC, it should not be a cause for increases in patient mortality.
This study found that patients experiencing pneumothorax and pulmonary contusion had significantly lower sagittal dimensions (p<0.05). This data suggests that a standard compression depth increases intrathoracic trauma in patients with smaller sagittal dimensions.
When the relationship between rib fracture and thoracic measurements was analysed, thoracic volumes and longitudinal dimensions were found to be significantly lower in the group with rib fractures (p<0.05). This again suggests that standard compression depths increase rib fracture incidence as thorax dimensions and volume decrease. This similarly supports the idea that low volume and dimensions correlate with increased thoracic trauma.
This study has a number of limitations. Firstly, the study was designed retrospectively. Furthermore, the patients included in the study were generally of advanced age, which may limit the applicability of this findings. Additionally, cardiac tamponade, myocardial hematoma/rupture, and vertebral fracture cases were severely limited (one case each), preventing specific conclusions about these types of trauma. The compression depth used during CPR was also not measured in our study. Despite this, all CPR applications carried out in the hospital were performed by experienced professional healthcare providers educated according to current guidelines. Measurement of compression depth in future studies may allow more objective data collection. Finally, the borders were manually defined when measuring thorax volumes. Though minimal, this does introduce a certain amount of error and subjectivity.
Future studies conducted prospectively on a larger population with more cases may provide more benefit to the literature.
CONCLUSION
CPR-related thoracic injury incidence is higher in patients with low thoracic volume and dimensions when compression depth and frequency are standardised. According to the results of this study, patients with lower thorax volumes and sagittal dimensions are at increased risk of CPR- related injury. The discussion of individualised compression depths may provide benefit to the continued development of resuscitation techniques.
ACKNOWLEDGEMENT:
We are thankful to Radiology Department of the Hospital, especially to Dr. Aytug Genc for his support on evaluating tomography scans.
ETHICAL APPROVAL:
The study was approved by the Institutional Ethics Committee of Kartal Dr. Lutfi Kirdar City Hospital.
PATIENTS’ CONSENT:
The data were collected retrospectively from Hospital Automation System and Archives, after obtaining ethical approval. The need for signed informed consent was waived due to retrospective design of the study.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS' CONTRIBUTION:
NMH: Conceptualisation, methodology, software, writing-reviewing and editing, investigation.
MOE: Conceptualisation, methodology, writing-original draft preparation, supervision, investigation, data curation, validation.
All authors had access to the manuscript at every stage of the preparation. They approved and uploaded the manuscript all together.
REFERENCES
- Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed-chest cardiac massage. Jama 1960; 173(10):1064-7. doi: 10.1001/jama.1960.03020280004002.
- Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, et al. Part 7: adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015; 132(18_suppl_2): S444-S64. doi: 10.1161/CIR.0000000000000261.
- Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, et al. Part 3: adult basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2020; 142(16_Suppl_2):S366-S468. doi: 10.1161/CIR.0000000000000916.
- Kleinman ME, Brennan EE, Goldberger ZD, Swor RA, Terry M, Bobrow BJ, et al. Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015; 132(18_suppl_2):S414-S35. doi: 10.1161/CIR.0000000 000000259.
- Kim HI, Cha KC, Chung WJ, Noh YI, Kim OH, Cha YS, et al. Effect of chest compression on skeletal chest injuries: A retrospective study. Eur J Emer Med 2020; 27(1):59-63. doi: 10.1097/MEJ.0000000000000617.
- Rudinská LI, Hejna P, Ihnát P, Tomášková H, Smatanová M, Dvořáček I. Intra-thoracic injuries associated with cardiopulmonary resuscitation–Frequent and serious. Resuscitation 2016; 103:66-70. doi: 10.1016/j.resuscitation.2016.04.002.
- Kashiwagi Y, Sasakawa T, Tampo A, Kawata D, Nishiura T, Kokita N, et al. Computed tomography findings of complications resulting from cardiopulmonary resuscitation. Resuscitation 2015; 88:86-91. doi: 10.1016/j.resuscitation.2014. 12.022.
- Olds K, Byard RW, Langlois NE. Injuries associated with resuscitation–an overview. J Forensic Legal Med 2015; 33:39-43. doi.org/10.1016/j.jflm.2015.04.003
- Azeli Y, Olazabal JVL, García MIM, Bardají A. Understanding the adverse hemodynamic effects of serious thoracic ınjuries during cardiopulmonary resuscitation: A review and approach based on the campbell diagram. Frontiers Physiol 2019; 10. doi: 10.3389/fphys.2019.01475.
- Park BH, Sung HH, Jeong BC, Seo SI, Jeon SS, Lee HM, et al. Tumor size is associated with compensatory hypertrophy in the contralateral kidney after radical nephrectomy in patients with renal cell carcinoma. Int Urol Nephrol 2016; 48(6):977-83. doi: 10.1007/s11255-016-1250-y.
- Park BH, Jeong BC, Jeon SS, Seo SI, Lee HM, Choi HY, et al. Volumetric measurement of compensatory hypertrophy in the contralateral normal kidney by the tumor growth. World J Urol 2016; 34(1):63-8. doi: 10.1007/s00345-015-1551-2.
- Viniol S, Thomas RP, König A, Betz S, Mahnken A. Early whole-body CT for treatment guidance in patients with return of spontaneous circulation after cardiac arrest. Emergency Radiology 2020; 27(1):23-9. doi: 10.1007/s10140- 019-01723-x.
- Friberg N, Schmidbauer S, Walther C, Englund E. Skeletal and soft tissue injuries after manual and mechanical chest compressions. Eur Heart J Qualaity Care Clin Outcomes 2019; 5(3):259-65. doi: 10.1093/ehjqcco/qcy062.
- Oh JH, Kim HI. Analysis of the cardiopulmonary resuscitation-related complications based on computed tomography. J Korean Society Emerg Med 2020; 31(5):431-9.
- Karasek J, Blankova B, Doubkova A, Pitasova T, Nahalka D, Bartes T, et al. CPR related injuries. European Heart J 2020; 41(Supplement_2):ehaa946. 1827.
- Zaidi HQ, Li S, Beiser DG, Tataris KL, Sharp WW. The utility of computed tomography to evaluate thoracic complications after cardiopulmonary resuscitation. Resuscitation Plus 2020; 3:100017. doi.org/10.1016/j.resplu.2020.100017.
- Young N, Cook B, Gillies M. New resuscitation guidelines may result in an increased incidence of severe chest wall injury, and lead to prolonged length of stay in the Intensive Care Unit. Resuscitation 2011; 82(10):1355. doi: 10.1016/j.resuscitation.2011.06.011.
- Stiell IG, Brown SP, Nichol G, Cheskes S, Vaillancourt C, Callaway CW, et al. What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients? Circulation 2014; 130(22):1962-70. doi: 10.1161/cırculatıonaha.114.008671.
- Atkins DL, Berger S, Duff JP, Gonzales JC, Hunt EA, Joyner BL, et al. Part 11: Pediatric basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015; 132(18_suppl_2):S519-S25.
- Topjian AA, Raymond TT, Atkins D, Chan M, Duff JP, Joyner Jr BL, et al. Part 4: Pediatric basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatric 20201; 147(Suppl 1):e2020038505D.